
Recent medical statistics show that hysterectomy is a common procedure in the United States, with over 600,000 operations performed annually.
Two primary techniques—robotic-assisted hysterectomy and laparoscopic hysterectomy—fall under minimally invasive surgery. Both methods reduce recovery time, minimize scarring, and lower the risk of complications compared to traditional open surgery.
It’s important for patients and healthcare providers to understand the differences between these minimally invasive surgery options. This knowledge helps in choosing the safest and most effective treatment plan tailored to each patient.
Key Takeaways
- Robotic and laparoscopic hysterectomy are both used for uterus removal.
- The choice between the two techniques depends on several factors, including the patient’s condition and the surgeon’s expertise.
- Both methods are considered minimally invasive, reducing recovery time.
- Robotic assisted hysterectomy offers enhanced precision and flexibility.
- Laparoscopic hysterectomy is a more traditional approach with a established track record.
Understanding Hysterectomy: A Brief Overview

Hysterectomy is a common surgery in women’s health. It involves removing the uterus and sometimes other tissues.
This surgery has been key in gynecologic care for many years. It’s done for reasons like uterine cancer, severe endometriosis, and uterine prolapse.
Types of Hysterectomy Procedures
There are different types of hysterectomy procedures. Each has its own reasons and benefits.
- Total Hysterectomy: Removal of the entire uterus, including the cervix.
- Partial Hysterectomy: Removal of the upper part of the uterus, leaving the cervix intact.
- Radical Hysterectomy: Removal of the uterus, cervix, part of the vagina, and sometimes lymph nodes, often performed in cases of cancer.
The choice of hysterectomy depends on the patient’s condition and the surgeon’s judgment.
Evolution of Surgical Techniques
Hysterectomy surgery has changed a lot over time. Now, there’s a big move towards less invasive methods.
Techniques like laparoscopic and robotic-assisted surgeries are becoming more common. They offer smaller cuts, less pain, and faster healing.
“The advancement in surgical techniques has transformed the standard of care for patients undergoing hysterectomy, providing more options and better results.”
The changes in hysterectomy surgery aim to improve patient care. They aim to make recovery faster and life better for women after the surgery.
The Fundamentals of Minimally Invasive Surgery in Gynecology
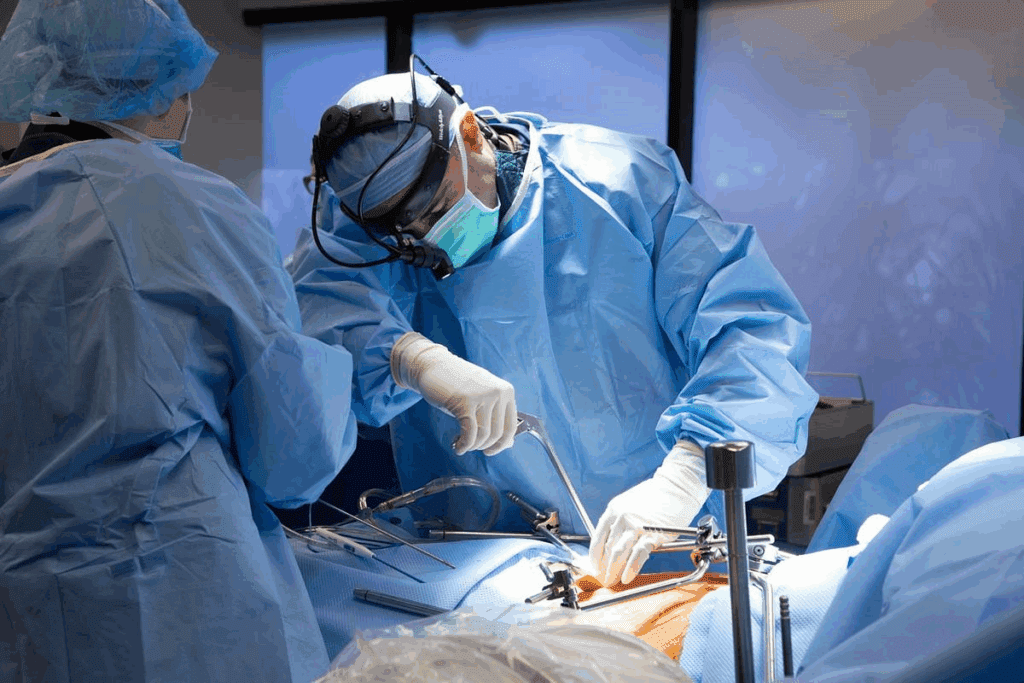
Minimally invasive surgery has changed gynecology for the better. It offers patients less painful options than traditional surgery. This method cuts down on recovery time, reduces pain, and lowers the chance of complications.
Key Principles of Minimally Invasive Techniques
Minimally invasive surgery in gynecology follows key principles. These include:
- Minimizing tissue trauma and disruption is crucial for better patient outcomes.
- Reducing the size and number of incisions
- Utilizing advanced surgical instrumentation and technology
- Enhancing visualization through laparoscopy or robotic systems
By following these principles, surgeons can get great results. They do this while making the surgery less hard on patients.
Benefits Compared to Traditional Open Surgery
Minimally invasive surgery in gynecology has many benefits. Some key advantages are:
- Reduced Recovery Time: Patients usually stay in the hospital less and get back to normal faster.
- Less Postoperative Pain: Smaller cuts mean less pain and discomfort for patients.
- Improved Cosmetic Outcomes: This method often leaves less noticeable scars.
- Lower Risk of Complications: It can lower the risk of infections and other issues seen with open surgery.
Patient Selection Criteria
Not every patient is right for minimally invasive surgery. The criteria include:
- Medical history and current health status
- The nature and complexity of the gynecological condition
- Previous surgical history and presence of adhesions
- Patient preferences and expectations
A detailed check by a healthcare expert is key. It helps decide the best surgery for each patient.
Laparoscopic Hysterectomy Explained
The laparoscopic approach to hysterectomy has changed gynecological surgery. It’s a less invasive option compared to traditional open surgery. This method uses small incisions for laparoscopic instruments to perform the surgery.
The Surgical Technique and Approach
Laparoscopic hysterectomy is done under general anesthesia. The surgeon makes small incisions in the abdomen, about 0.5 to 1 cm long. A laparoscope, a thin tube with a camera and light, is used to see the pelvic organs on a video monitor.
Laparoscopic instruments are then used through other incisions to remove the uterus. The procedure needs precise surgeon control and manual dexterity to safely remove the uterus.
Equipment and Instruments Used
The success of laparoscopic hysterectomy relies on the right equipment and instruments. The main tools include:
- Laparoscope with high-definition camera
- Laparoscopic graspers and dissectors
- Electrosurgical units for cutting and coagulation
- Suturing devices for closure
| Instrument | Function |
| Laparoscope | Provides visualization of the pelvic cavity |
| Laparoscopic Graspers | Used to grasp and manipulate tissues |
| Electrosurgical Units | Enable cutting and coagulation of tissues |
Surgeon Control and Manual Dexterity
The success of laparoscopic hysterectomy depends on the surgeon’s skill. This includes manual dexterity and understanding the anatomy from two-dimensional images.
Surgeons need special training for laparoscopic procedures. They must learn to use laparoscopic instruments and handle the unique challenges of laparoscopic surgery, like limited depth perception and the need for precise control.
Robotic Hysterectomy: Technological Advancements
Robotic hysterectomy uses advanced systems like the da Vinci Surgical System. This technology has changed gynecological surgery a lot. It makes surgeries more precise, improves how doctors see the area, and helps patients recover faster.
The da Vinci Surgical System Components
The da Vinci Surgical System is a top-notch robotic tool for complex surgeries. It has several parts that work together for a smooth surgery.
- Surgeon Console: This is where the surgeon sits and works. It has a 3D, high-definition screen for a clear view of the surgery area.
- Robotic Arms: The system has robotic arms with surgical tools. These arms move like the surgeon’s hands, allowing for precise work.
- Patient-Side Cart: This cart holds the robotic arms and is by the patient. It has tools that can be changed during surgery.
Surgeon Console and Control Mechanisms
The surgeon console is made to reduce fatigue and improve control. It has:
- 3D Visualization: Gives a detailed view of the surgery area, helping with precision.
- Hand Controls: These controls let the surgeon move the robotic arms with precision, making small movements easier.
- Foot Pedals: Foot pedals control functions like electrocautery and camera movements, keeping the surgeon focused.
Robotic Arms and Instrument Capabilities
The robotic arms are key to the da Vinci Surgical System. They offer:
| Feature | Description | Benefit |
| Instrument Variety | Many surgical tools are available, like scissors and electrocautery tools. | More versatility during surgery. |
| Precision | The tools are made for precise movements and control. | Better surgical accuracy. |
| Range of Motion | The arms can move in ways human hands can’t. | More dexterity in complex surgeries. |
The advancements in robotic hysterectomy, like the da Vinci Surgical System, have greatly improved gynecological surgery. They make surgeries more precise, improve visualization, and help patients recover faster.
Surgical Incisions and Anatomical Access
The way surgeons make incisions and access the body changes between laparoscopic and robotic hysterectomy. This affects how well patients do after surgery. It’s important for doctors and patients to understand these differences.
Number and Size of Incisions
Laparoscopic hysterectomy needs 3 to 4 small cuts, each 0.5 to 1.5 cm long. Robotic hysterectomy, like with the da Vinci Surgical System, also has small cuts but they’re even smaller, about 0.8 to 1.2 cm. The exact number of cuts depends on the surgery’s complexity and the surgeon’s style.
Robotic surgery might need a bit bigger cut for the camera, about 1 to 2 cm. The other cuts are smaller. The size and number of cuts can affect how the scars look and how quickly you recover.
Port Placement Differences
Where the ports go is key in both surgeries. Laparoscopic surgery lets the surgeon choose based on the patient’s body. Robotic surgery has a set way because of the robotic arms. The ports are placed to avoid problems and get the best view of the area being operated on.
Cosmetic Outcomes and Scarring
Scarring and how the surgery looks are big worries for many patients. Both laparoscopic and robotic hysterectomy have smaller cuts than open surgery. This means less noticeable scars. But, robotic surgery might have a slight edge in making scars less visible.
In summary, both laparoscopic and robotic hysterectomy are better than open surgery for looking good and scarring less. But, the size of the cuts and where they are placed can affect how much scarring there is and how happy the patient is.
Operative Differences: Precision and Technique
Robotic and laparoscopic hysterectomy procedures have key differences. These differences are mainly in instrument precision and tissue manipulation. They greatly affect the surgical technique and results.
Instrument Range of Motion
The range of motion of surgical tools is very important in hysterectomy. Robotic systems give better instrument range of motion. This lets for more detailed work in the pelvic area.
This is very helpful when you need to carefully cut around important parts.
- Robotic instruments can rotate 360 degrees, giving more flexibility.
- Laparoscopic instruments have limited degrees of freedom, making complex tasks harder.
Tissue Manipulation and Dissection
Tissue manipulation and dissection are key steps in hysterectomy. Robotic systems help with careful handling of tissues. This is because they offer precise control.
This precision lowers the chance of tissue damage. It also makes dissection more accurate.
- The robotic system’s better visualization helps find tissue planes.
- Precise control lets for gentle tissue handling.
Suturing and Knot-Tying Capabilities
The skill to do suturing and knot-tying well is very important in hysterectomy. Robotic systems make these tasks better with their easy-to-use controls and clear vision.
Key benefits include:
- Improved dexterity for complex suturing tasks.
- Enhanced visualization for accurate knot-tying.
3D Visualization vs. 2D Visualization
The way we see during hysterectomy surgery really matters. The main difference is between robotic and laparoscopic methods. This difference comes down to the technology used for seeing.
Laparoscopic Imaging Limitations
Laparoscopic surgery uses 2D images. This can make it hard for surgeons to see depth. It’s tough to judge how far apart things are, which can affect surgical precision.
Seeing in 2D can lead to more problems. Surgeons need a lot of skill to work around this lack of depth.
Robotic Enhanced Depth Perception
Robotic surgery, on the other hand, uses 3D visualization. This makes seeing depth much better. It helps surgeons understand where everything is in 3D.
The 3D visualization in robotic systems helps surgeons see better. This means they can do more precise work, like cutting and sewing.
Impact on Surgical Precision
3D vision in robotic surgery means better surgical precision. This is key in complex surgeries. Accurate work is very important.
Research shows 3D vision leads to fewer problems and better results. The precision it offers is a big plus in today’s surgery.
Surgeon Ergonomics and Learning Curve
Robotic systems are changing how surgeons do complex surgeries like hysterectomies. They make surgeries more comfortable and less tiring for surgeons. This could make surgical care better overall.
Physical Demands on Surgeons
Laparoscopic surgery is less invasive but can be very demanding. Surgeons need to control instruments precisely and use rigid tools. This can cause surgeon fatigue, which might make the surgery less safe.
Robotic systems aim to lessen this strain. They let surgeons work in a more natural way. This reduces the chance of getting tired or uncomfortable during long surgeries.
Training Requirements and Adaptation
The learning curve for laparoscopic and robotic hysterectomies differs. It depends on the surgeon’s experience and training. Robotic systems are easier to learn, thanks to their intuitive controls and better visuals.
“Robotic surgery has the chance to shorten the learning curve for complex surgeries. This makes it easier for surgeons who are new to laparoscopic techniques.”
Impact on Surgeon Fatigue and Performance
Surgeon fatigue is a big concern in surgery. It can affect how well a surgery goes. Robotic systems help by making surgeries less tiring for surgeons. This is good for complex and long surgeries.
Research shows robotic surgery’s ergonomic benefits. It leads to better focus and fewer mistakes. This improves patient safety and surgery results.
Patient Recovery and Clinical Outcomes
Recovery after hysterectomy can differ based on the surgery type. Laparoscopic and robotic surgeries are both minimally invasive. Yet, they have unique aspects that affect how patients heal.
Hospital Stay Duration Comparison
Both laparoscopic and robotic hysterectomies lead to shorter hospital stays than open surgery. But, the exact time can differ between these two methods.
| Surgical Method | Average Hospital Stay |
| Laparoscopic Hysterectomy | 1-2 days |
| Robotic Hysterectomy | 1 day |
Post-Operative Pain Management
Managing pain well is key for recovery. Robotic hysterectomy often causes less pain. This is because it uses smaller cuts and less tissue damage.
Complication Rates and Types
Both laparoscopic and robotic hysterectomies have low complication rates. Yet, the types of problems can vary. Robotic surgery might lower the risk of some issues because of its precise nature.
- Laparoscopic: Higher risk of bleeding and infection
- Robotic: Lower risk of bleeding, but possible mechanical issues
Return to Normal Activities Timeframe
Patients usually heal faster with minimally invasive surgeries. The time to get back to normal activities varies. But, most can do so within a few weeks.
Return to normal activities: 2-4 weeks for both, with some studies showing robotic surgery might be quicker.
In summary, both laparoscopic and robotic hysterectomies have benefits for recovery and outcomes. Yet, there are differences that might influence the choice of surgery. Knowing these differences is key for making the right decision.
Specific Applications in Minimally Invasive Surgery
Gynecological surgery is moving towards less invasive methods. This change means patients face less recovery time and fewer complications. These new methods are being used for complex cases.
Complex Hysterectomy Cases
Complex hysterectomies, like those with large fibroids or endometriosis, are now done with less invasive techniques. These methods allow for precise dissection and removal of the uterus. This reduces the risk of complications.
Robotic-assisted surgery is very helpful in these cases. It offers better visualization and dexterity.
Pelvic Reconstructive Procedures
Minimally invasive surgery is also used for pelvic reconstructive procedures. For example, sacrocolpopexy for pelvic organ prolapse. These procedures need precise dissection and suturing.
Robotic or laparoscopic instruments help achieve this. The benefits include shorter recovery times and less pain for patients.
Oncologic Applications
In gynecologic oncology, minimally invasive surgery is used for treating cancers. The da Vinci Surgical System is a robotic platform used for these surgeries. It allows for precise tumor removal.
Studies show that in some cases, this method leads to fewer complications and quicker recovery. It does so without compromising cancer treatment outcomes.
Minimally invasive surgery’s use in these areas shows its versatility. It has the power to improve patient outcomes for many gynecological conditions.
Cost Considerations and Healthcare Economics
When deciding on a hysterectomy, cost is a big factor. It looks at the initial cost, ongoing expenses, insurance, and how cost-effective each method is.
Initial Investment and Equipment Costs
Robotic systems cost a lot more than laparoscopic tools at first. For example, the da Vinci Surgical System is very expensive. This can be a big problem for hospitals.
Key costs associated with robotic systems include:
- Purchase price of the robotic system
- Maintenance and upgrade costs
- Training for surgeons and staff
Per-Procedure Expenses
The cost of each robotic hysterectomy can change a lot. It depends on how many surgeries are done and what materials are used. Laparoscopic surgeries are usually cheaper because they don’t need special robotic tools.
Factors influencing per-procedure expenses include:
- Cost of disposable instruments
- Operating room time
- Length of hospital stay
Insurance Coverage and Reimbursement
Insurance and how it covers costs are also important. Different policies can change how much patients have to pay out of pocket.
Cost-Effectiveness Analysis
Looking at how much each method costs is key. It includes direct costs like equipment and hospital stay, and indirect costs like recovery time. Some studies say robotic surgery might be more expensive upfront but could lead to faster recovery and fewer complications.
Key elements of a cost-effectiveness analysis include:
- Comparative costs of the procedures
- Outcomes in terms of patient recovery and complications
- Long-term cost implications
Clinical Decision Making: Selecting the Appropriate Approach
The choice between laparoscopic and robotic hysterectomy depends on many factors. These factors affect the surgery’s outcome and the patient’s recovery.
Patient-Specific Factors
When choosing a surgical approach, patient-specific factors are key. These include:
- Medical History: Patients with a history of previous surgeries or certain medical conditions may benefit from one approach over the other.
- Anatomical Considerations: The size and location of the uterus, as well as any adhesions or other anatomical factors, can influence the choice of surgical technique.
- Overall Health: The patient’s overall health and any risks associated with the surgery are also considered.
Surgeon Experience and Preference
The surgeon’s experience and preference are also important. Their expertise can greatly impact the surgery’s outcome.
Surgeon training and familiarity with the equipment are essential for effective clinical decision making.
Institutional Resources and Availability
Institutional resources, including equipment and trained staff, can also influence the choice. Hospitals with advanced robotic systems may prefer robotic hysterectomy for certain cases. The availability of trained personnel and support staff is critical for the success of either surgical approach.
By considering these factors, healthcare providers can make informed decisions. These decisions optimize patient outcomes.
Conclusion: Making an Informed Decision
It’s important to know the differences between laparoscopic and robotic hysterectomy. This knowledge helps patients and doctors choose the best surgery. They can consider what each patient needs and what the surgery might do.
Choosing between these surgeries depends on many things. These include the patient’s health, the surgeon’s skill, and what resources are available. Each surgery has its good points and things to think about. Knowing these helps ensure the best results for the patient.
Patients can make a smart choice by looking at the pros and cons of each surgery. This way, they can pick what’s best for them. This leads to better health outcomes for everyone involved.
FAQ
What is the main difference between robotic and laparoscopic hysterectomy?
The main difference is in the surgical method and technology. Laparoscopic surgery uses manual tools with 2D views. Robotic surgery, on the other hand, uses the da Vinci System for 3D views and precise robotic arms.
What are the benefits of minimally invasive surgery in gynecology?
Minimally invasive surgery has many benefits. It leads to quicker recovery, less pain, and smaller cuts. This means better looks and fewer risks of problems.
How does the da Vinci Surgical System enhance robotic hysterectomy?
The da Vinci System gives 3D views and better depth perception. It also has robotic arms for precise control. This makes dissection, suturing, and tissue manipulation more accurate.
What are the key differences in surgical incisions between laparoscopic and robotic hysterectomy?
Laparoscopic surgery uses many small cuts. Robotic surgery needs a few small cuts for the arms and a bigger cut for removing the specimen. The size and number of cuts affect how the area looks and scars.
How does surgeon ergonomics impact laparoscopic and robotic hysterectomy?
Robotic surgery is easier on the surgeon, reducing strain and fatigue. The surgeon works from a console. Laparoscopic surgery requires more manual skill and can be harder physically.
What are the patient recovery differences between laparoscopic and robotic hysterectomy?
Both surgeries are quicker to recover from than open surgery. Robotic surgery might cause less pain and shorter stays in the hospital. This is because it’s more precise and causes less tissue damage.
How do cost considerations impact the choice between laparoscopic and robotic hysterectomy?
Robotic surgery is more expensive because of the da Vinci System and procedure costs. Insurance and payment plans can also affect the choice.
What factors influence clinical decision making when selecting between laparoscopic and robotic hysterectomy?
Many things matter, like the patient’s needs, the surgeon’s skills, and what resources are available. The choice depends on the patient’s situation, the surgery’s complexity, and the surgeon’s experience.
Are there specific applications where robotic hysterectomy is preferred over laparoscopic hysterectomy?
Yes, robotic surgery is better for complex cases, pelvic repairs, and cancer surgeries. It offers better precision, 3D views, and tool control.
How does the learning curve for robotic hysterectomy compare to laparoscopic hysterectomy?
Robotic surgery’s learning curve is shorter because of the da Vinci System’s ease of use. Yet, both need special training and skills to master.
Reference
- Sinha, R., et al. (2018). Comparison of Robotic and Laparoscopic Hysterectomy for Large Uteri. Journal of Minimally Invasive Gynecology. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6328360/



































