Last Updated on November 17, 2025 by Ugurkan Demir

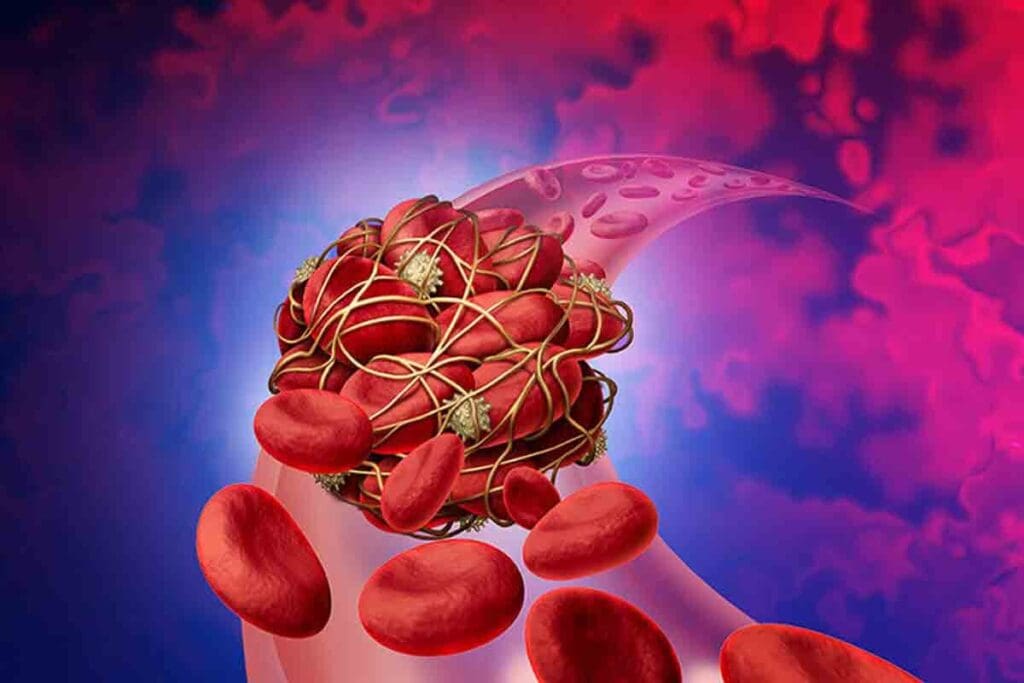
Blood clots can sneak up on you, causing serious problems. At LivHospital, we know how vital it is to spot the signs early. A blood clot happens when blood thickens and turns into a semi-solid mass. This can happen naturally to stop bleeding or abnormally inside blood vessels.
Spotting clot symptoms early is key. If not treated, blood clots can cause big health issues. LivHospital aims to give top-notch care and support to international patients. We’re here to help you grasp the causes and warning signs of blood clots.

Blood clotting is a vital process that prevents excessive bleeding. But, it can become dangerous when clots form inappropriately. We will explore how blood clots form, when they become problematic, and where they commonly occur.
The normal clotting process is a complex series of events. It involves multiple cell types and proteins. When a blood vessel is injured, the body’s first response is to constrict the vessel to reduce blood flow.
Platelets then adhere to the injury site, forming a platelet plug. The coagulation cascade is activated. This results in the formation of fibrin, a protein that reinforces the platelet plug, creating a stable clot.
Key components of the normal clotting process include:
While clotting is a natural response to injury, it can become dangerous when it occurs inappropriately or excessively. Abnormal clot formation can lead to conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke. These conditions can be life-threatening and require immediate medical attention.
“Thrombosis is a major cause of morbidity and mortality worldwide, and understanding its mechanisms is critical for developing effective prevention and treatment strategies.”
Thrombosis Expert
Blood clots can form in various parts of the body. They most commonly occur in the deep veins of the legs (DVT) and in the arteries. Arterial thrombosis can lead to heart attacks and strokes, while venous thrombosis is associated with DVT and PE.
| Location | Type of Thrombosis | Potential Complications |
| Deep Veins (Legs) | Venous Thrombosis (DVT) | Pulmonary Embolism (PE) |
| Arteries | Arterial Thrombosis | Heart Attack, Stroke |
Blood clots can form due to genetics, lifestyle, and environment. Knowing these risk factors helps identify who’s at higher risk. It also guides how to prevent them.
Genetics are key in blood clotting. If your family has a history of blood clots, you might be at risk too. Certain genes, like Factor V Leiden, can raise your risk.
Age matters a lot. The risk of blood clots goes up after 40. Women, on estrogen therapy or pregnant, face a higher risk too.
Smoking and using substances also raise clot risk. Smoking harms blood vessel linings. Some substances can affect blood clotting and heart health.
Let’s look at these risk factors in a clear format:
| Risk Factor | Description | Prevention Tips |
| Genetic Predisposition | Family history of clotting disorders | Know your family history, consult a doctor |
| Age | Risk increases after 40 | Regular check-ups, stay active |
| Immobility | Prolonged sitting or bed rest | Take regular breaks to move, exercise |
| Smoking | Damages blood vessel lining | Quit smoking, avoid secondhand smoke |
Knowing these risk factors and taking steps to prevent them can lower your clot risk. Being aware of clot signs is key to getting quick medical help if needed.
Many health conditions can make blood clots more likely. Some medical conditions can change how blood clots. We will look at key conditions that raise blood clot risk.
Heart problems, like atrial fibrillation and heart failure, increase blood clot risk. Atrial fibrillation causes blood to pool in the heart, forming clots. Heart failure, with an inefficient heart, also leads to clot formation due to poor blood flow.
“Atrial fibrillation is a major risk factor for stroke, which is often caused by blood clots,” says recent research. Managing heart diseases with medicine and lifestyle changes is key to lowering blood clot risk.
Cancer and blood disorders can also raise blood clot risk. Some cancers, like pancreatic cancer, produce substances that make blood clot more easily. Blood disorders, including thrombophilia, affect blood clotting, increasing clot risk.
Autoimmune conditions, like lupus and antiphospholipid syndrome, increase blood clot risk. These conditions cause the immune system to produce antibodies that make blood clot more easily. Managing these conditions through treatment and lifestyle changes is vital to reduce blood clot risk.
“Autoimmune disorders can significantly increase the risk of thrombosis, making it critical to manage these conditions effectively.”
Recent surgery or trauma also raises blood clot risk. Surgery can damage blood vessels, causing clots. Trauma, leading to immobility, is another risk factor for blood clots. Knowing the risks of surgery and trauma helps in taking steps to prevent blood clots.
It’s important to know the signs of blood clots in your limbs. Blood clots in the deep veins of your legs or arms are called deep vein thrombosis (DVT). If not treated, they can cause serious problems.
DVT symptoms can be different for everyone. But common signs include swelling, pain, redness, and warmth in the affected limb. You might feel a persistent ache or throbbing sensation that doesn’t get better with rest. It’s key to watch for these signs and notice any changes in your body.
It can be hard to tell if you have DVT or just muscle pain. Muscle pain usually gets better with rest and might feel stiff or crampy. But DVT pain stays the same or gets worse over time.
As a medical expert once said,
“The key to diagnosing DVT is not just recognizing its symptoms but understanding the risk factors and being vigilant, specially in high-risk patients.”
If you notice any of these, get medical help right away:
Getting help early can make a big difference. If you’re not sure about your symptoms, talk to a doctor.
Knowing the signs of pulmonary embolism is key to getting help fast. Pulmonary embolism (PE) happens when a blood clot goes to the lungs. This can be very dangerous. We’ll look at the warning signs of PE, how they differ from other lung problems, and why you need to see a doctor right away.
Pulmonary embolism shows up with sudden and severe symptoms. Common signs include:
Telling PE symptoms apart from other lung problems can be hard. Symptoms often look similar. But, PE symptoms come on fast and are very severe.
For example, asthma or COPD can make it hard to breathe. But, sharp chest pain or coughing up blood points more to PE. Knowing the difference is important for getting the right treatment.
Some PE symptoms need you to get help right away. If you or someone else has:
Call emergency services or get to the hospital fast. Quick treatment can make a big difference in PE cases.
We stress the importance of knowing these dangerous lung clot symptoms. And acting fast when they happen.
Many people think blood clots only happen in the legs. But they can also form in the brain, heart, abdomen, and kidneys. This can lead to serious and life-threatening conditions. It’s important to know the signs of blood clots in these areas to get medical help fast.
A blood clot in the brain can cause a stroke. This is a serious condition that needs immediate treatment. Look out for these symptoms:
If you or someone you know has these symptoms, get emergency medical care right away.
Blood clots in the heart can cause a heart attack. This is when blood flow to the heart muscle is blocked. Look for these signs:
Calling emergency services quickly can help a lot.
Blood clots in the abdomen can cause severe pain and other problems. Watch for these symptoms:
These symptoms need quick medical evaluation to find the cause and treatment.
Blood clots can also affect other organs like the kidneys. Symptoms vary by organ. For kidney clots, look out for:
Some life situations make us more likely to get blood clots. It’s important to know these situations so we can take steps to prevent them. Knowing the causes of blood clots helps us stay safe.
Being in bed for a long time after surgery or in the hospital raises our risk of blood clots. This is true for surgeries like hip, knee, or abdomen operations. Doctors often give advice on how to move and stay safe, like exercises or wearing compression stockings.
Pregnancy and after having a baby increase blood clot risk. This is because of changes in blood and more pressure on veins. Women should watch for signs of blood clots and talk to their doctor. Drinking water, moving often, and taking medicine as directed can help.
Traveling far, like by plane or car, means sitting for a long time. This can lead to blood clots. To avoid this, drink water, stretch, and wear compression stockings. If you’re at high risk, talk to your doctor before you travel.
Having COVID-19 can make blood clots more likely. This is because of the body’s reaction to the virus and staying in bed. People who had COVID-19 should watch for signs of blood clots and see a doctor if they have any. Those in the hospital with severe COVID-19 are at even higher risk and may get medicine to prevent clots.
| High-Risk Situation | Risk Factors | Preventive Measures |
| After Surgery or Hospitalization | Prolonged immobility, type of surgery | Exercises, compression stockings, anticoagulant medication |
| During Pregnancy and Postpartum | Changes in blood clotting, increased venous pressure | Staying hydrated, regular movement, anticoagulant medication if prescribed |
| Long-Distance Travel | Prolonged sitting | Staying hydrated, regular breaks to move, compression stockings |
| COVID-19 Infection | Inflammatory response, potentially immobility | Awareness of blood clot signs, seeking medical attention if symptoms occur, anticoagulant therapy in severe cases |
Knowing about these high-risk situations and taking steps to prevent blood clots is key. This way, we can lower our risk and get help quickly if needed.
It’s vital to diagnose blood clots correctly for effective treatment. Blood clots can be deadly if not treated quickly. We’ll look at how to diagnose, treat, and recover from blood clots.
Doctors use physical checks, medical history, and imaging tests to find blood clots. Ultrasound is a key test for leg clots. For lung clots, a CT pulmonary angiogram (CTPA) is often used.
Other tests include:
These tools help doctors find and understand blood clots. This guides the right treatment.
Treating blood clots often means using blood thinners. These drugs stop clots from growing and prevent new ones. Common blood thinners are:
In severe cases, thrombolytic therapy might be used. This therapy dissolves clots directly.
Some patients need surgery or interventional procedures. These include:
These options are for when blood thinners don’t work or are not suitable.
Recovering from a blood clot means ongoing care to avoid future problems. Patients need to watch for:
| Follow-up Care | Description | Frequency |
| INR monitoring | Checking the international normalized ratio to ensure appropriate blood thinning | Regular, as advised by healthcare provider |
| Compression stockings | Wearing compression stockings to reduce swelling and pain | Daily, as prescribed |
| Lifestyle modifications | Making changes to diet, exercise, and smoking habits | Ongoing |
Managing blood clots well needs a full plan, from diagnosis to follow-up. Knowing these steps helps patients and doctors work together to reduce risks and improve health.
Knowing the signs of blood clots can save lives. We’ve talked about different symptoms that can show up in the legs, arms, lungs, and brain.
Getting help early is key to avoiding serious problems. At LivHospital, we offer top-notch care and support for international patients. We stress the need for prevention and quick medical action if symptoms don’t go away or get worse.
By understanding the risks and taking steps to prevent blood clots, people can lower their chances of getting them. We urge everyone to watch their health closely and get medical help right away if they notice anything odd.
Signs of blood clots include swelling and pain in a limb. You might also notice warmth and redness. Shortness of breath, chest pain, and coughing up blood are symptoms of pulmonary embolism.
Look out for swelling, pain, or discoloration in your legs or arms. Difficulty breathing, chest pain, or a rapid heartbeat are also warning signs. If you notice these, get medical help right away.
Blood clot risk factors include genetics and age. Being immobile, smoking, and having cancer or heart disease also increase your risk. Recent surgery or trauma can also play a role.
While some risks can’t be changed, there are steps you can take. Stay active, avoid smoking, and manage health conditions. These actions can lower your risk of blood clots.
DVT is a blood clot in the deep veins, usually in the legs. Doctors use ultrasound or other tests to diagnose it.
Symptoms of PE include shortness of breath and chest pain. You might also cough up blood or have a fast heartbeat.
Blood clot treatment often involves anticoagulant medications. Sometimes, surgery or interventional procedures are needed.
Untreated blood clots can cause serious problems. These include pulmonary embolism, stroke, and damage to organs.
Yes, you can have a blood clot without feeling any symptoms. It’s important to know your risk factors and take preventive steps.
To lower your risk of blood clots while traveling, stay hydrated and move often. Wearing compression stockings can also help.
Yes, certain conditions like cancer, heart disease, and autoimmune disorders raise your risk of blood clots.
If you think you have a blood clot, get medical help right away. Quick treatment can prevent serious problems.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!