At LivHospital, we know that getting a bone marrow transplant is scary. This big medical step has many parts — from tests before the transplant to recovery afterwards. Many patients often wonder, how long is bone marrow transplant and what the full process involves.
A bone marrow transplant saves lives by putting healthy stem cells into your body. These cells replace old or sick bone marrow that can’t make enough blood cells. Our team is here to help you through every step, making sure you get the care and support you need.
We’ll guide you through what happens from start to finish in the transplant process — including preparation, the procedure itself, and the healing phase. At LivHospital, our goal is to help you achieve the best possible outcome and a smooth recovery.
Key Takeaways
- Understand the stages involved in a bone marrow transplant.
- Learn about the preparation required before the transplant.
- Discover what happens during the transplant procedure.
- Find out what to expect during the recovery phase.
- Get insights into the extensive care provided by LivHospital.
Understanding Bone Marrow Transplantation
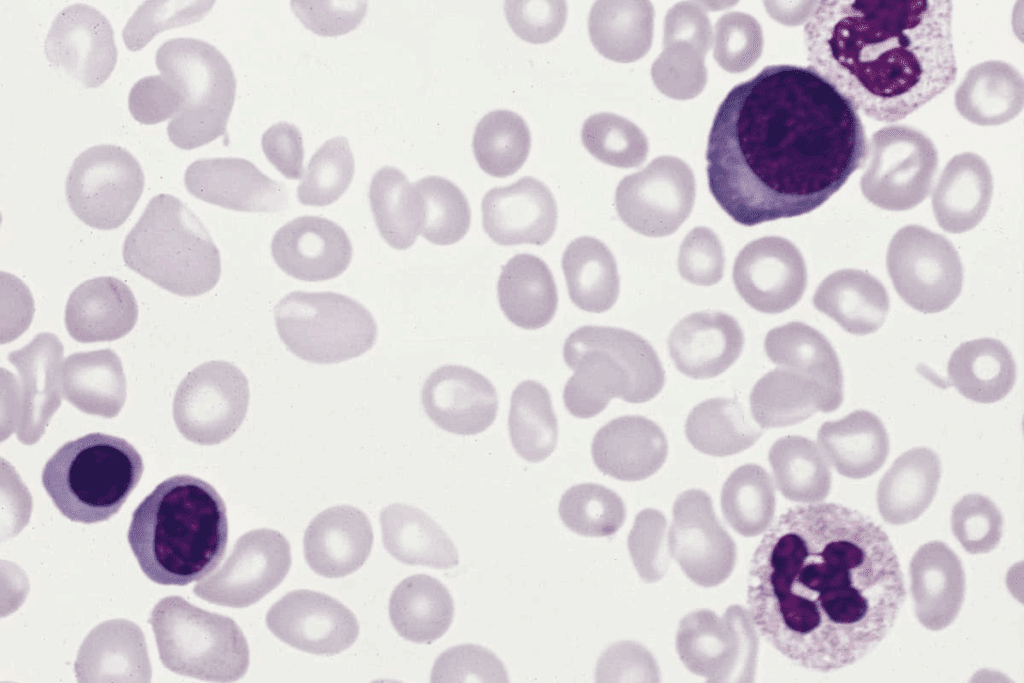
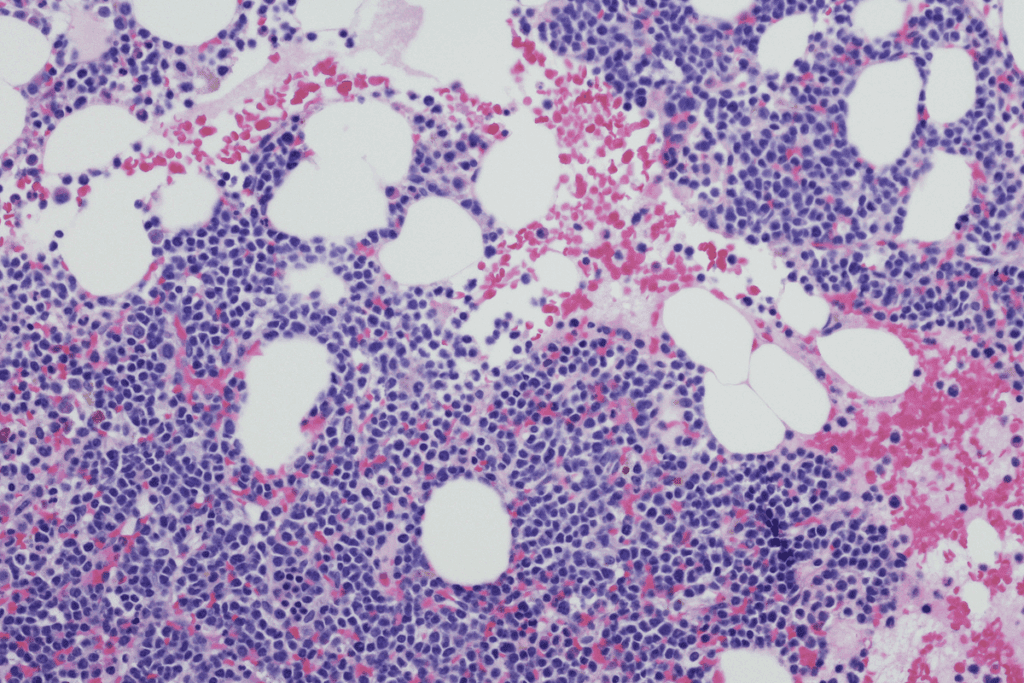
To understand bone marrow transplantation, we must first learn about bone marrow. It’s the spongy tissue in some bones that makes blood cells. These cells carry oxygen, fight infections, and stop bleeding.
What is Bone Marrow and Why is it Important?
Bone marrow is key to making blood cells. It makes red blood cells for oxygen, white blood cells for fighting infections, and platelets for clotting.
Types of Bone Marrow Transplants
There are two main types of bone marrow transplants: autologous and allogeneic.
- Autologous Transplants: Use the patient’s own bone marrow or stem cells. These are collected, stored, and then given back after treatment.
- Allogeneic Transplants: Use bone marrow or stem cells from a donor. The donor can be a family member, an unrelated donor, or umbilical cord blood.
Common Conditions Requiring Bone Marrow Transplants
Bone marrow transplants treat serious conditions, including:
- Leukemia: A cancer of the blood or bone marrow.
- Lymphoma: A cancer of the lymphatic system.
- Multiple Myeloma: A cancer of plasma cells in the bone marrow.
- Aplastic Anemia: A condition where the bone marrow fails to produce blood cells.
- Inherited Blood Disorders: Such as sickle cell disease and thalassemia.
These conditions often need bone marrow transplantation as a possible cure.
The Complete Bone Marrow Transplant Timeline
A bone marrow transplant is more than one step. It’s a long process that can take months. It includes getting ready, the transplant itself, and recovery.
Overview of the Multi-Stage Process
The bone marrow transplant process has many stages:
- Initial Consultation: Checking if the patient is a good candidate for a transplant.
- Pre-Transplant Preparation: Finding a donor, placing a catheter, and starting treatment.
- The Transplant: When stem cells are infused into the patient.
- Post-Transplant Recovery: Watching for problems and helping the patient get better.
From Initial Consultation to Full Recovery
The journey to full recovery is long. Here’s what happens:
- Initial Evaluation: Checking the patient’s health and planning the next steps.
- Pre-Transplant Phase: Finding a donor and getting the patient ready physically and mentally.
- Transplantation: The day the stem cells are infused.
- Recovery Phase: Care after the transplant, including hospital stays and check-ups.
Factors Affecting Transplant Duration
Many things can change how long a bone marrow transplant takes:
- Patient’s Overall Health: Health before the transplant can affect how fast they recover.
- Type of Transplant: Using your own cells or a donor’s can change the timeline.
- Donor Availability: Finding a good match can take a lot of time.
- Complications: Problems during or after the transplant can make recovery longer.
Pre-Transplant Phase: Preparation and Testing
Pre-transplant preparation is a detailed process. It includes tests and evaluations to check if a patient is ready for a bone marrow transplant. This phase is key to see if the patient can have the transplant and to find any risks.
Initial Evaluation and Eligibility Assessment
The first step is a thorough check of the patient’s health and their condition. We do blood tests, imaging, and other tests to see if they can have the transplant.
Eligibility criteria look at the patient’s age, health, and disease stage. We also check if they are physically and emotionally ready for the transplant.
Finding a Compatible Donor
Finding a donor who matches the patient is very important. We look for a donor with the same human leukocyte antigen (HLA) as the patient. This can be a family member or someone else, and we use special tests to find the best match.
Finding a donor can take a lot of time. We work with national and international registries to find a good match.
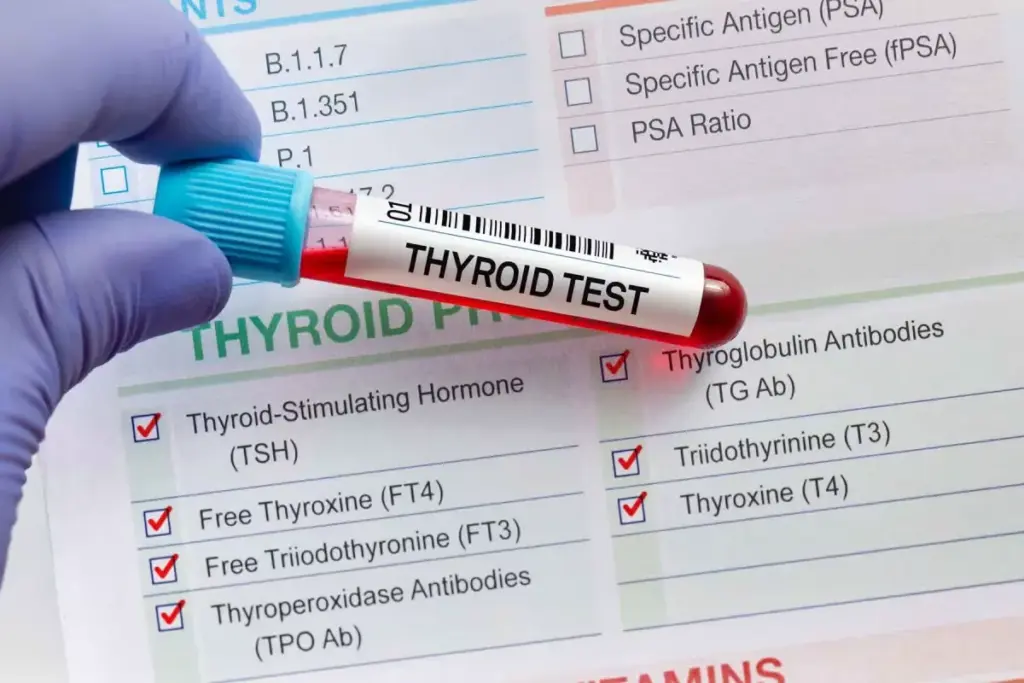
Pre-Transplant Testing and Examinations
Before the transplant, we do tests to check the patient’s health. These tests include cardiac evaluations, pulmonary function tests, and infectious disease screening.
We also do psychological evaluations to see if the patient is mentally ready for the transplant. This way, we make sure we cover all health aspects before the transplant.
How Long is Bone Marrow Transplant Preparation?
The bone marrow transplant preparation is complex. It includes medical checks, finding a donor, and mental support. This step is key to making sure the transplant goes well and is safe.
Timeline for Donor Matching
Finding a compatible donor is the first step. The time it takes can change based on several things. It might take weeks or even months to find a donor.
We use special typing to find the best donor for the patient. After finding a donor, we do more tests to make sure they match. This whole process is important and takes time.
Central Venous Catheter Placement
Another key part is putting in a central venous catheter (CVC). This catheter is used for giving medicine and blood products. It’s placed under local anesthesia and takes about 30 to 60 minutes.
Putting in a CVC is a precise step to avoid problems. Our team makes sure it’s done right and the patient is comfortable.
Physical and Psychological Preparation
Physical prep is also critical. Patients have many tests to check their health. This includes heart and lung tests to find any risks.
Mental prep is just as important. The transplant can be tough on the mind. We offer counseling and support groups to help with stress and anxiety. We want patients to be ready physically and mentally.
By focusing on each part of prep, we aim for a successful transplant and a good recovery for our patients.
How is a Bone Marrow Transplant Performed: Collection Methods
Getting stem cells is key in bone marrow transplants. There are several ways to do this. The method chosen depends on the patient’s health, the transplant type, and if a donor is available.
Bone Marrow Harvesting Procedure
Bone marrow harvesting takes stem cells directly from the bone. It’s done from the hip bone, under general or local anesthesia. A small incision is made, and a needle is used to get the stem cells.
This surgery is done in an operating room and lasts 1-2 hours. The patient or donor is given anesthesia to reduce pain. After, the bone marrow is processed to get the stem cells ready for transplant.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is non-surgical. It gets stem cells from the blood. Before, the donor or patient takes meds to release stem cells into the blood. Then, apheresis is used to collect and return the blood.
This process can take hours and might need several sessions. It’s less invasive than bone marrow harvesting and allows for quicker recovery.
Umbilical Cord Blood Collection
Umbilical cord blood collection gets stem cells from the umbilical cord and placenta after birth. It’s used when a donor is needed and cord blood is available. The cord blood is then frozen and stored for later use.
Cord blood is a good source of stem cells. It’s readily available and less likely to cause graft-versus-host disease. But, it might not have enough stem cells for adult patients.
Duration of Collection Procedures
The time it takes to collect stem cells varies. Bone marrow harvesting is 1-2 hours. Peripheral blood stem cell collection can take hours to a day. Umbilical cord blood collection happens right after birth and doesn’t add to the transplant time.
Knowing about the different stem cell collection methods and their times helps prepare patients and donors. Each method has its benefits and challenges, and the choice depends on individual needs.
Conditioning Therapy: Purpose and Timeline
Conditioning therapy is a key step before a bone marrow transplant. It uses high-dose chemotherapy and sometimes radiation. This process gets the body ready for the new stem cells by removing diseased cells and weakening the immune system.
Chemotherapy Process
The chemotherapy process is central to conditioning therapy. We use strong chemotherapy drugs to kill cancer cells and get the bone marrow ready for the transplant. The drugs and doses depend on the patient’s health, the transplant type, and other factors.
Chemotherapy can cause side effects like nausea, tiredness, and hair loss. Our medical team watches over patients to help with these side effects and keep them comfortable.
Role of Radiation Therapy
Radiation therapy is sometimes added to chemotherapy in conditioning therapy. It kills any cancer cells left in the body, making the bone marrow ready for the transplant. Whether to use radiation therapy depends on the disease type and stage.
Duration and Side Effects
Conditioning therapy lasts from a few days to a week. Its side effects can be tough, including tiredness, nausea, diarrhea, and hair loss. Our team offers full care to handle these side effects, with medicines and supportive therapies.
After conditioning therapy, patients are ready for the bone marrow transplant. The transplant’s success depends on how well the conditioning therapy prepared the body for the new stem cells.
Bone Marrow Transplant Procedure: The Transplantation Day
“Day 0” is a big day for patients getting a bone marrow transplant. It’s when they get stem cells in their body. This marks the end of a long wait and the start of their healing journey.
What Happens on “Day 0”
Patients usually go to the hospital early on this day. The stem cell infusion process is quick, taking 30 minutes to a few hours. This depends on the patient’s needs and the amount of stem cells.
The stem cells are given through a special line in the vein, like a blood transfusion. The medical team watches closely to keep the patient safe and comfortable.
The Stem Cell Infusion Process
The stem cell infusion is a key part of the transplant. The stem cells go to the bone marrow to make new blood cells. This is vital for fixing the bone marrow and helping the patient get better.
While the infusion happens, doctors watch for any bad reactions. They are ready to handle any problems that might come up.
Duration of the Actual Transplant
The actual infusion takes 30 minutes to a few hours. But the whole day is longer because of getting ready and watching the patient after.
| Procedure | Duration |
| Pre-infusion preparation | 1-2 hours |
| Stem cell infusion | 30 minutes to a few hours |
| Post-infusion monitoring | 1-2 hours |
Immediate Post-Infusion Monitoring
Right after the infusion, patients are watched closely for any problems. This can take a few hours. It’s important to keep them safe and make sure the transplant works.
The medical team looks for signs of the transplant working. They also check how the patient is doing. They adjust care as needed to help with recovery.
Post-Transplant Recovery Timeline
Recovering from a bone marrow transplant is a detailed process. It needs a good care plan. The recovery journey has several stages, each with its own timeline and needs.
Hospital Stay Duration
The time spent in the hospital after a transplant varies. Patients usually stay for 2-4 weeks. This time is key for watching the patient’s health and handling any quick problems.
Our medical team is always there, day and night. They make sure the patient is safe and comfortable.
Engraftment Process and Timeline
Engraftment is when the new stem cells start making blood cells. It’s a big step in recovery. Usually, it happens in 2-4 weeks after the transplant.
Patients have regular blood tests to track engraftment. Our team looks for signs like more white blood cells. This helps us know when it’s time to leave the hospital.
Monitoring for Complications
After a transplant, patients face risks like infections and graft-versus-host disease (GVHD). Our team keeps a close eye on these risks. They do regular check-ups and tests to spot problems early.
This way, we can act fast to manage any issues. It helps the patient recover better.
The Medical Team’s Role During Recovery
The medical team plays a big role in recovery. We take care of symptoms, prevent infections, and watch for engraftment or complications. We also support patients and their families emotionally and psychologically.
By working closely with patients, we can customize care. This ensures the best results for each patient.
Long-Term Recovery and Follow-Up
After a bone marrow transplant, patients start a critical recovery phase. This phase is key for the transplant’s success and the patient’s health. It requires careful monitoring and follow-up care.
The First 100 Days After Transplant
The first 100 days are very important. The patient’s immune system starts to recover. We watch for signs of engraftment, infection, or GVHD.
Regular appointments help us track the patient’s progress. We address any complications quickly.
- Regular blood tests to monitor blood cell counts and detect any abnormalities.
- Medications to prevent infection and GVHD.
- Nutritional counseling to ensure adequate nutrition during recovery.
3-6 Month Recovery Milestones
After the first 100 days, the immune system keeps improving. We see big milestones in the 3-6 month period. Energy levels improve, and infection risk decreases.
But, we must stay alert for late transplant effects.
Key aspects of this phase include:
- Gradual tapering of immunosuppressive medications under close supervision.
- Ongoing monitoring for signs of GVHD or disease relapse.
- Resumption of normal activities, with guidance on safe exercise and lifestyle choices.
6-12 Month Recovery Process
By 6-12 months, many patients see a big improvement in their immune function. We keep a close eye on their health. We adjust treatment plans as needed to manage side effects or complications.
During this period, patients often report:
- Improved overall well-being and increased energy.
- Return to many pre-transplant activities, with some restrictions.
- Ongoing follow-up care to address any emerging issues.
Long-Term Follow-Up Schedule
Long-term care is vital for managing transplant effects and ensuring health. We create a follow-up schedule tailored to each patient’s needs.
Our care plan includes regular check-ups and monitoring for complications. We also support managing long-term side effects. By working closely with our patients, we aim to improve their recovery and quality of life post-transplant.
Conclusion: The Bone Marrow Transplant Journey
A bone marrow transplant is a complex process that needs a lot of care and support. We’ve looked at the different steps in the marrow transplant procedure. This includes everything from the first meeting to the long recovery period.
The bone marrow transplant process starts with careful preparation. This includes finding a compatible donor and preparing the body for the transplant. We talked about how important it is to have a good match and the ways to collect bone marrow.
It’s key for patients and their families to understand the bone marrow transplant journey. Knowing what to expect helps them make better decisions about their care.
Support is essential at every step. Our team is committed to providing top-notch care and support. We believe that with the right care, patients can have a better quality of life and successful outcomes.
FAQ
How long does a bone marrow transplant take?
The time it takes for a bone marrow transplant varies. It depends on the type of transplant, the patient’s health, and any complications. Generally, it can take several months to a year or more.
What is the bone marrow transplant procedure?
The bone marrow transplant process includes several steps. These are the pre-transplant evaluation, donor matching, conditioning therapy, stem cell collection, and infusion. The transplant itself takes a few hours. But the whole process is complex and needs careful preparation and follow-up care.
How is a bone marrow transplant performed?
The transplant involves infusing healthy stem cells into the patient’s bloodstream. These stem cells come from a donor’s bone marrow, blood, or umbilical cord. The procedure is done in a hospital, where the patient is closely watched for any issues.
What is conditioning therapy in a bone marrow transplant?
Conditioning therapy is a treatment given before the transplant. It’s high-dose chemotherapy and/or radiation to destroy the diseased bone marrow. This prepares the body for the new stem cells. The treatment’s duration and side effects vary based on the patient’s condition and the transplant type.
How long is the hospital stay after a bone marrow transplant?
The hospital stay after a transplant varies. It depends on the patient’s condition and any complications. Usually, patients stay in the hospital for weeks to a few months.
What is the engraftment process in a bone marrow transplant?
Engraftment is when the transplanted stem cells start making new blood cells. This happens a few weeks after the transplant. The medical team watches the patient’s blood counts to make sure engraftment is successful.
How long does it take to recover from a bone marrow transplant?
Recovery from a bone marrow transplant can take months to a year or more. The first 100 days are very important. Patients need close monitoring and follow-up care to manage complications and ensure successful engraftment.
What is the long-term follow-up schedule after a bone marrow transplant?
Long-term care is key after a bone marrow transplant. Patients need regular check-ups with their medical team. This includes blood tests, imaging studies, and other exams to monitor their health and catch any complications early.
Can I find a compatible donor for a bone marrow transplant?
Finding a compatible donor depends on several factors. These include the patient’s genetic makeup and the availability of donors. We work with patients and their families to find donors and conduct matching tests for the best outcome.
What are the possible complications of a bone marrow transplant?
Bone marrow transplants can have complications. These include graft-versus-host disease, infections, and organ damage. Our medical team closely monitors patients to reduce these risks and ensure the best outcome.
References
- Majhail, N. S., & Farnia, S. H. (2018). The blood and marrow transplant clinical trials network: A decade of progress. Biology of Blood and Marrow Transplantation, *24*(6), 1119–1124. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5993710/