We often think anemia means low iron. But anemia of chronic disease (ACD) can happen even with normal iron. It’s linked to long-term illnesses like infections, autoimmune diseases, and cancer.
At Liv Hospital, we know ACD is a unique condition. We focus on understanding its causes and symptoms. Our team aims to offer innovative, patient-focused care for ACD.
ACD is a complex issue for people with chronic diseases. It’s key to grasp its underlying causes for proper treatment. We’ll dive into the essential facts and causes of ACD, guiding you through this complex condition.
Key Takeaways
- Anemia of chronic disease can occur with normal iron levels.
- ACD is linked to chronic illnesses, such as infections and autoimmune diseases.
- Liv Hospital provides thorough care for ACD patients.
- Understanding ACD’s causes and symptoms is vital for diagnosis and treatment.
- ACD needs a special approach, unlike iron deficiency anemia.
What Happens When You Have Anemia With Normal Iron Levels
Anemia with normal iron levels is a complex issue. It involves chronic disease and how the body makes red blood cells. Anemia of Chronic Disease (ACD) is when people have anemia but their iron levels are normal. This is often linked to chronic inflammation and disease.

The Paradox of Normal Iron but Low Hemoglobin
In ACD, people might have low hemoglobin but normal iron levels. Or, they might have a low red blood cell count with normal iron stores. This happens because inflammation can cause anemia, even without iron deficiency.
Inflammation makes it hard for the body to use stored iron for making red blood cells. This leads to anemia.
“In anemia of inflammation, you may have a normal or sometimes increased amount of iron stored in your body tissues, but a low level of iron in your blood. Inflammation may prevent your body from using stored iron to make enough healthy red blood cells, leading to anemia.”
-Doctors note.
How ACD Differs from Iron Deficiency Anemia
ACD is different from Iron Deficiency Anemia (IDA). IDA is caused by not having enough iron. But ACD is caused by chronic inflammation and disease.
The main difference is how the body uses iron. In IDA, iron stores are low. In ACD, iron stores are normal or even high.
| Characteristics | Anemia of Chronic Disease (ACD) | Iron Deficiency Anemia (IDA) |
| Iron Stores | Normal or Elevated | Depleted |
| Cause | Chronic Inflammation/Disease | Insufficient Iron |
| Hemoglobin Levels | Low | Low |
Prevalence and Impact on Quality of Life
ACD is common in people with chronic diseases. This includes chronic inflammatory diseases, infections, cancer, and kidney disease. The impact on quality of life is significant.
Symptoms include fatigue, weakness, and shortness of breath. These symptoms make managing the underlying condition harder.
ACD affects patients physically and emotionally. It’s important to understand ACD to develop effective management strategies. These strategies should address both the anemia and the underlying chronic disease.
Anemia of Chronic Disease Causes and Underlying Conditions
Anemia of Chronic Disease (ACD) is a complex condition linked to various chronic illnesses and inflammatory processes. It’s not just a simple deficiency but a multifaceted disorder. It arises from chronic diseases, including autoimmune conditions, infections, cancer, and kidney disease.
Chronic Inflammatory Diseases
Chronic inflammatory diseases are a significant cause of ACD. Conditions such as rheumatoid arthritis and inflammatory bowel disease (IBD) lead to persistent inflammation. This inflammation affects iron utilization and red blood cell production.
This inflammation triggers the production of hepcidin, a protein that regulates iron metabolism. It reduces available iron for erythropoiesis.
Chronic Infections
Chronic infections, including tuberculosis and HIV/AIDS, can also lead to ACD. These infections cause prolonged inflammation. This disrupts normal iron homeostasis and impairs red blood cell production.
The body’s response to chronic infection can lead to anemia despite adequate iron stores.
Cancer and Malignancies
Cancer and its treatment are associated with ACD. The inflammation and metabolic changes caused by malignancies affect iron metabolism and erythropoiesis. Treatments like chemotherapy can further suppress bone marrow activity, contributing to anemia.
Kidney Disease and Other Chronic Conditions
Chronic kidney disease (CKD) is another significant underlying condition that can lead to ACD. The kidneys produce erythropoietin, a hormone essential for red blood cell production. In CKD, reduced erythropoietin production and chronic inflammation contribute to anemia.
Other chronic conditions, such as chronic heart failure and diabetes, can also contribute to the development of ACD.
Here’s a summary of the underlying conditions that can lead to ACD:
| Underlying Condition | Mechanism Leading to ACD |
| Chronic Inflammatory Diseases | Persistent inflammation affects iron utilization |
| Chronic Infections | Prolonged inflammation disrupts iron homeostasis |
| Cancer and Malignancies | Inflammation and metabolic changes affecting erythropoiesis |
| Chronic Kidney Disease | Reduced erythropoietin production and chronic inflammation |
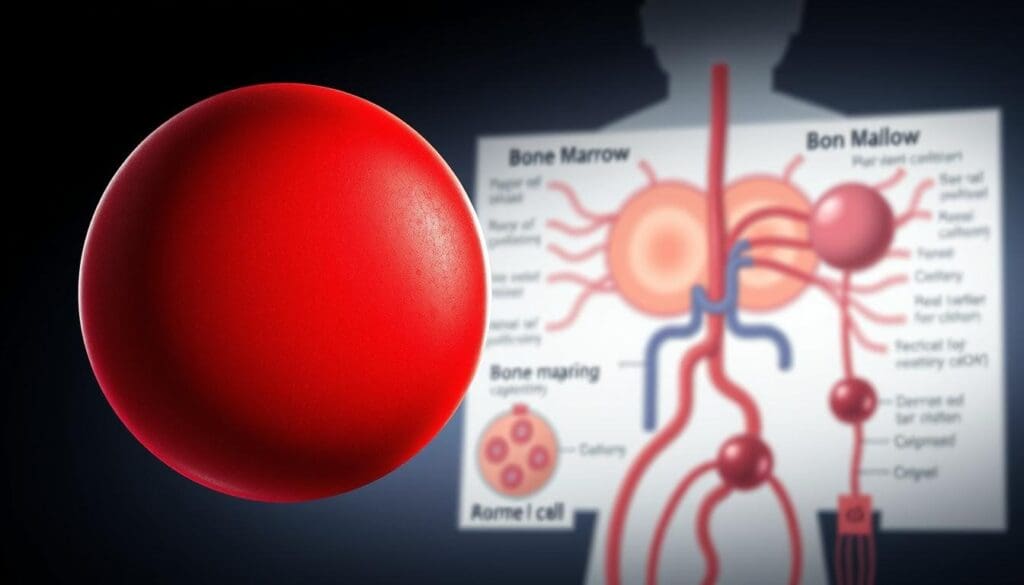
How Inflammation Creates Anemia Despite Normal Iron Stores
Inflammation can cause anemia even with normal iron levels. This is called Anemia of Chronic Disease (ACD). Chronic inflammation messes with how the body uses iron and makes red blood cells.
The Critical Role of Hepcidin
Hepcidin is a protein that controls iron in the body. When inflammation happens, hepcidin levels go up. This makes less iron available for making red blood cells. This is a big reason why anemia can happen even with enough iron.
Trapped Iron: Available but Inaccessible
High hepcidin levels stop iron from being released from storage. This means iron is trapped and can’t be used to make hemoglobin, even if there’s enough.
Suppressed Red Blood Cell Production
Inflammation also stops red blood cells from being made. Cytokines, which are made during inflammation, can stop the hormone needed for red blood cells from being made. This makes anemia worse.
Shortened Red Blood Cell Survival
Inflammation also makes red blood cells last shorter. This means red blood cells are taken out of the body faster than they can be made, making anemia worse.
In conclusion, inflammation causes anemia in several ways. It increases hepcidin, traps iron, stops red blood cell production, and shortens their life. Knowing these effects helps doctors diagnose and treat Anemia of Chronic Disease better.
Recognizing Symptoms and Clinical Presentation
Anemia of chronic disease has symptoms that can really affect a person’s life. These signs can be similar to other anemia types, making it hard to diagnose without a detailed check-up.
Common Symptoms of ACD
People with anemia of chronic disease often feel tired, weak, and pale. They might also have shortness of breath and feel dizzy. This is because their bodies don’t get enough oxygen due to fewer red blood cells or less hemoglobin.
Some might also have a fast heartbeat, body aches, and even faint. It’s important to remember that these signs can also be from the chronic disease itself.
When Symptoms Overlap With the Underlying Disease
The symptoms of ACD can be tricky because they can also be signs of the chronic disease. For example, someone with chronic kidney disease might feel tired from both the anemia and the kidney issue. This makes it hard to know what’s causing the symptoms.
Doctors need to look at the whole picture to figure out if it’s ACD or the chronic disease causing the symptoms.
Severity Spectrum: Mild to Severe Manifestations
The symptoms of ACD can vary a lot. Some people might only feel a little tired, while others might be very weak and have trouble breathing. This can really affect their daily life and how well they feel.
| Symptom Severity | Common Symptoms | Impact on Daily Life |
| Mild | Minimal fatigue, slight pallor | Little to no impact |
| Moderate | Noticeable fatigue, shortness of breath on exertion | Some impact on daily activities |
| Severe | Debilitating fatigue, significant shortness of breath at rest | Significant impact, may require assistance |
How Symptoms Differ from Iron Deficiency Anemia
ACD and iron deficiency anemia can have similar symptoms, but there are differences. Iron deficiency anemia often causes cravings for non-food items and restless legs. ACD symptoms can be more subtle and might be overshadowed by the chronic disease..
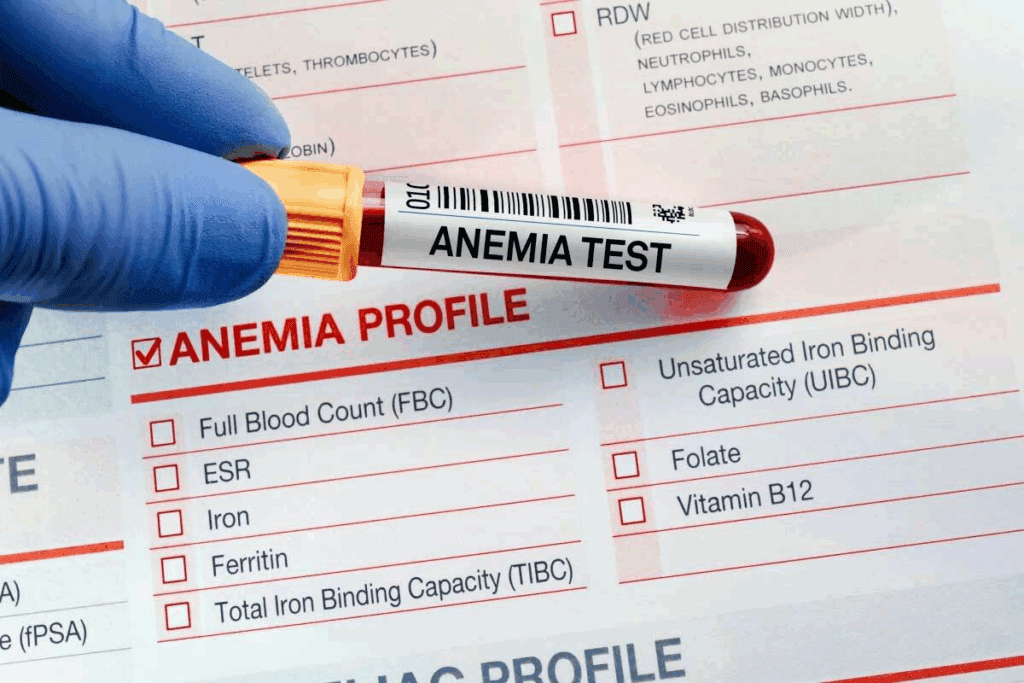
Diagnosis: Identifying Anemia of Chronic Disease With Normal Iron
Diagnosing anemia of chronic disease, even with normal iron, is complex. Doctors use a detailed approach to spot ACD.
Key Laboratory Findings and Patterns
Several tests are key to diagnosing ACD. These include:
- Complete Blood Count (CBC) to check hemoglobin and hematocrit
- Iron studies to look at serum iron, ferritin, and transferrin saturation
- Inflammatory markers like C-reactive protein (CRP) to measure inflammation
People with ACD often have normocytic anemia. Their red blood cells are normal size but fewer in number. Iron tests show low serum iron and low transferrin saturation, but ferritin is normal or high. This means they have enough stored iron.
| Laboratory Test | Typical Findings in ACD |
| Hemoglobin | Decreased |
| Serum Iron | Low |
| Ferritin | Normal or Elevated |
| Transferrin Saturation | Low |
| CRP | Elevated |
Differential Diagnosis and Ruling Out Other Causes
It’s important to rule out other anemia types, like iron deficiency anemia. Doctors look at lab results and the patient’s situation carefully.
“The diagnosis of ACD needs careful thought, mainly in patients with long-term diseases. It’s key to tell ACD apart from other anemias to treat it right.”
— Clinical Hematology Expert
When to Suspect ACD Despite Normal Iron Tests
Thinking ACD might be present with normal iron levels needs a deep understanding. Doctors should think of ACD in patients with ongoing inflammation or infections, even with normal iron tests.
Advanced Diagnostic Approaches
At times, more detailed tests are needed to confirm ACD. These might include:
- Checking hepcidin levels, often high in ACD
- Looking at erythropoietin levels to see how the bone marrow reacts to anemia
- Exploring the chronic condition causing ACD
By using clinical insight, lab results, and advanced tests, doctors can accurately diagnose and treat ACD, even with normal iron levels.
Treatment Strategies and Management Options
Anemia of chronic disease (ACD) treatment focuses on managing the underlying inflammation. It’s not just about iron levels. ACD treatment involves a wide approach, including treating the inflammation’s cause.
Targeting the Underlying Condition
The main goal in treating ACD is to tackle the chronic condition causing inflammation. By addressing the root cause, we can help improve anemia or its symptoms. This might involve different treatments, like anti-inflammatory drugs or specific cancer therapies.
When Iron Therapy Is Helpful (and When It’s Not)
Iron therapy isn’t always the answer for ACD. The problem isn’t usually a lack of iron but the body’s inability to use it because of inflammation. But, if there’s also iron deficiency, iron supplements can help. It’s important to check for iron deficiency before starting therapy.
Erythropoiesis-Stimulating Agents
In some cases of ACD, erythropoiesis-stimulating agents (ESAs) are used. ESAs help make more red blood cells. This can improve hemoglobin levels and reduce the need for blood transfusions.
Emerging Therapies Targeting Inflammation
New research is exploring therapies that target ACD’s inflammatory pathways. One area of interest is developing drugs that affect hepcidin levels. Hepcidin is key in ACD because it controls iron availability.
| Treatment Approach | Description | Benefit |
| Targeting Underlying Condition | Managing the chronic condition causing inflammation | Potential alleviation of anemia |
| Iron Therapy | Supplementation in cases of co-existing iron deficiency | Improved iron levels |
| Erythropoiesis-Stimulating Agents | Stimulating red blood cell production | Improved hemoglobin levels |
| Emerging Therapies | Targeting inflammatory pathways and hepcidin modulation | Potential new treatment options |
Conclusion
Anemia of Chronic Disease (ACD) is a complex issue. It happens in people with ongoing inflammation, infection, or cancer. Even with normal iron levels, ACD can be hard to diagnose.
The body can’t use stored iron because of inflammation. This leads to fewer red blood cells being made.
It’s important to know if anemia causes inflammation or if it’s the other way around. In ACD, inflammation leads to anemia. Conditions that cause low iron and inflammation make things even more complicated.
It’s possible for patients to have anemia even with normal iron levels, which is a key sign of ACD. To diagnose this, doctors need to do detailed tests and evaluations. Treatment aims to manage the underlying cause, and may include special drugs or therapies.
Understanding ACD is key for doctors to give the right care. Recognizing the link between chronic disease, inflammation, and anemia helps improve patient outcomes and quality of life.
FAQ
Can you have anemia with normal iron levels?
Yes, it’s possible to have anemia even with normal iron levels. This is called Anemia of Chronic Disease (ACD). It happens when long-term inflammation messes with how the body uses iron and makes red blood cells.
What is Anemia of Chronic Disease (ACD)?
ACD is anemia that happens in people with long-term illnesses. This includes chronic inflammatory diseases, infections, cancer, and kidney disease. It’s when someone has anemia but their iron levels are normal, caused by ongoing inflammation.
How does inflammation cause anemia in ACD?
Inflammation leads to anemia in ACD by messing with iron use and red blood cell making. The body’s fight against inflammation makes hepcidin, a protein that controls iron. This makes iron hard to use for making red blood cells.
What are the symptoms of ACD?
Symptoms of ACD can vary and might seem like the disease itself. Common signs include feeling tired, weak, and short of breath. How bad these symptoms are can vary a lot.
How is ACD diagnosed?
Doctors use tests like complete blood count, iron studies, and inflammatory markers to diagnose ACD. It’s important to check for other anemia causes and think of ACD in people with long-term illnesses, even if iron tests seem normal.
Can iron therapy help in ACD?
Iron therapy might not work in ACD because the problem isn’t a lack of iron. It’s because inflammation stops the body from using iron. But, sometimes iron therapy can help if there’s also a lack of iron.
What are the treatment options for ACD?
Treating ACD means managing the underlying illness and using drugs to help make more red blood cells. New treatments that target inflammation are also being looked into.
Can ACD be treated by targeting the underlying condition?
Yes, treating the underlying illness is key in managing ACD. By controlling the chronic illness, anemia can be improved, and overall health can get better.
Is ACD a common condition?
ACD is fairly common, mainly in people with long-term illnesses. How common it is can depend on the illness and the group being studied.
How does ACD impact quality of life?
ACD can really affect someone’s quality of life, if not treated well. Symptoms like fatigue, weakness, and shortness of breath can make everyday tasks hard and affect overall happiness.
7 Key Causes of Acute on Chronic Anemia and Acute Blood Loss Anemia
Acute anemia means a quick drop in red blood cells. This makes it hard for tissues and organs to get enough oxygen. Knowing what causes and shows these problems is key for the best care.
Our team at Liv Hospital is dedicated to exceptional care for anemia patients. We make sure to give full support and care for those with sudden drops in hemoglobin and signs of shock.
Key Takeaways
- Understanding the causes of acute on chronic anemia and acute blood loss anemia is key for quick action.
- Liv Hospital’s expert teams offer full care for complex anemia cases.
- Spotting signs of shock and sudden drops in hemoglobin is critical for the best results.
- Acute anemia can cause serious problems if not treated right away.
Understanding Anemia: Basic Concepts and Classifications
Anemia is when there are fewer red blood cells or less hemoglobin. It’s a big health issue that needs to be understood well. It can happen for many reasons, like chronic diseases, not getting enough nutrients, or losing blood suddenly.
We’ll look at what anemia is, starting with its definition and how it works. The World Health Organization says anemia is when hemoglobin is below 13 g/dL in men and 12 g/dL in non-pregnant women. This is how doctors know if someone has anemia.
Definition and Pathophysiology of Anemia
Anemia isn’t just one thing; it’s a group of problems with red blood cells. It can be because of not getting enough iron, vitamin B12, or folate. Knowing how these issues happen is key.
The body tries to make up for not having enough red blood cells in different ways. For example, it might pump more blood or make blood vessels wider. This helps get oxygen to important parts of the body when there’s not enough red blood cells.
How Anemia is Characterized in Clinical Practice
Doctors use tests and physical checks to find anemia. They look at a complete blood count (CBC) to see if hemoglobin and red blood cells are okay. These tests help figure out if someone has anemia and how bad it is.
Finding out why someone has anemia is also important. Doctors might do more tests like checking for iron or looking at the bone marrow. Knowing the cause helps decide how to treat it.
| Parameter | Male | Female (Non-Pregnant) |
| Hemoglobin (g/dL) | < 13 | < 12 |
| Hematocrit (%) | < 39 | < 36 |
Understanding anemia helps doctors diagnose and treat it better. This improves how patients do. Anemia and not having enough blood can be even harder to deal with, but with the right care, patients can get better.
Acute on Chronic Anemia: Definition and Mechanism
Chronic anemia can worsen quickly with an acute event. Acute on chronic anemia is a serious condition that needs quick action.
What Constitutes Chronic Anemia
Chronic anemia means your body has too little hemoglobin for a long time. It can happen due to not enough nutrients, chronic diseases, or genetic issues. For example, iron deficiency anemia is common and can be treated.
The National Institute of Health says knowing why you have it is key to managing it well.
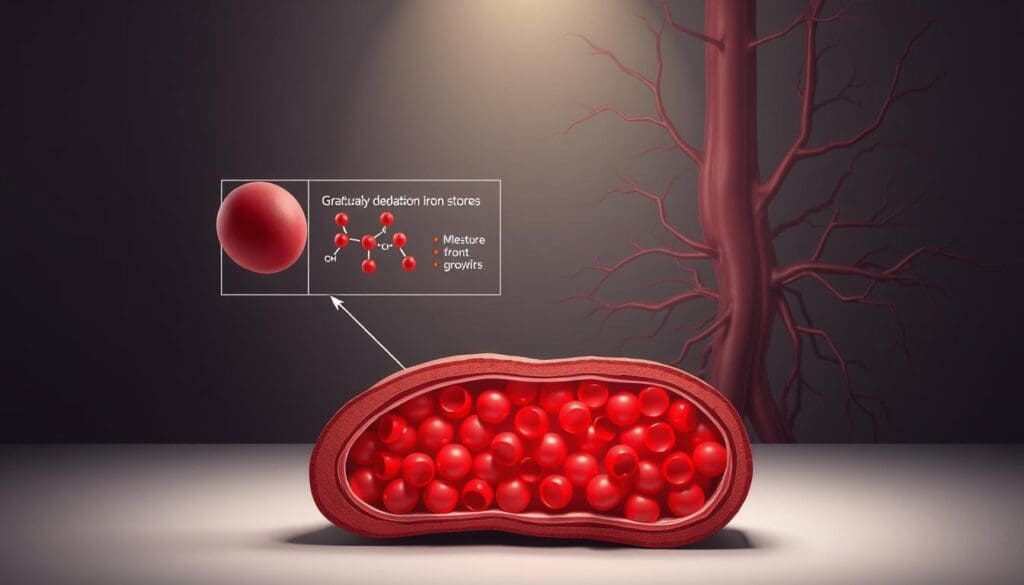
How Acute Events Trigger Worsening of Chronic Anemia
Events like bleeding, surgery, or injury can make chronic anemia worse. These can quickly lower your hemoglobin levels, making things harder for you.
For instance, someone with iron deficiency anemia might see their hemoglobin drop fast after surgery or injury.
The Physiological Impact of Rapid Hemoglobin Decline
When hemoglobin drops quickly, it affects your body a lot. Your heart and lungs try to make up for it by working harder. But if it drops too much, your organs might not get enough oxygen.
This can lead to serious problems, like organ failure.
Doctors need to understand acute on chronic anemia to help patients quickly. Spotting the signs early helps prevent serious issues.
Acute Blood Loss Anemia: Criteria and Presentation
Acute blood loss anemia happens when hemoglobin levels drop quickly. This can be due to trauma, surgery, or bleeding in the gut. It’s a serious condition that needs quick diagnosis and treatment.
Diagnostic Criteria for Acute Blood Loss Anemia
To diagnose acute blood loss anemia, doctors look for a sudden drop in hemoglobin. They check for signs like a fast heart rate, low blood pressure, and hemoglobin levels under 7 g/dL. Medical studies show these signs help spot patients who need urgent care.
Clinical Signs of Significant Blood Loss
Signs of significant blood loss include a fast heart rate, low blood pressure, and less urine. People might also feel dizzy, weak, or have trouble breathing. Spotting these signs early is key to managing the condition well.
Differentiating Acute from Chronic Blood Loss
Telling acute from chronic blood loss is important for the right treatment. Acute blood loss happens suddenly, while chronic develops over time. Knowing the type of blood loss helps doctors plan the best treatment.
Doctors stress that early detection and action are vital for managing acute blood loss anemia. We’ll look at how to manage it in the next sections.
7 Key Causes of Acute on Chronic Anemia
It’s important to know what causes acute on chronic anemia. This condition happens when someone with chronic anemia gets worse suddenly. This can be very serious if not treated right away.
1. Gastrointestinal Bleeding in Patients with Chronic Anemia
Gastrointestinal bleeding is a big reason for acute on chronic anemia. People with chronic anemia face serious risks if they bleed in their gut. This bleeding can come from ulcers, varices, or tumors.
2. Heavy Menstruation Exacerbating Iron Deficiency
Heavy periods can make anemia worse, mainly in women with iron deficiency. Losing a lot of blood can make symptoms like tiredness and shortness of breath worse.
3. Trauma or Surgery in Chronically Anemic Patients
Getting hurt or having surgery can make anemia worse in people who are already anemic. The blood lost during these events can lower hemoglobin levels, making things harder.
4. Medication-Induced Bleeding in Chronic Kidney Disease
People with chronic kidney disease might take medicines that can cause bleeding. This bleeding can make their anemia worse.
The other three key causes include:
- Chronic Inflammatory Diseases: Diseases like rheumatoid arthritis can cause chronic inflammation. This can make anemia worse.
- Cancer and Its Treatment: Some cancers and their treatments can cause both chronic and acute anemia.
- Infections: Severe infections can cause acute anemia in people with chronic anemia.
It’s key for doctors to know these causes to manage acute on chronic anemia well. Understanding the triggers helps them find the right treatments to help patients.
Gastrointestinal Bleeding: A Leading Cause of Acute Blood Loss
Gastrointestinal bleeding can quickly cause acute blood loss anemia, a serious condition. It’s a major medical emergency that can come from different parts of the GI tract.
We know that GI bleeding can be divided by where it starts in the GI tract. Knowing this helps us diagnose and treat it better.
Upper GI Sources: Ulcers, Varices, and Erosions
Upper GI bleeding often comes from peptic ulcers, varices, and mucosal erosions. Peptic ulcers are usually caused by Helicobacter pylori or NSAIDs. Varices are big veins in the esophagus that bleed easily. Erosions are small lesions that can also bleed a lot.
To manage upper GI bleeding, we first stabilize the patient. Then, we use endoscopy to find and possibly treat the bleeding source.
Lower GI Sources: Diverticulosis, Hemorrhoids, and Malignancies
Lower GI bleeding can come from diverticulosis, hemorrhoids, and cancers. Diverticulosis is when small pouches in the colon wall bleed. Hemorrhoids are swollen veins in the anus that bleed during bowel movements. Cancers can also cause GI bleeding.
To diagnose lower GI bleeding, we use clinical exams, imaging, and endoscopy. These help find where the bleeding is and how bad it is.
Management Approaches for GI Bleeding
Managing GI bleeding includes starting with resuscitation, finding the bleeding source, and treating it. Endoscopy is key for both finding and fixing the problem.
For severe bleeding, we might need more treatments like angiographic embolization or surgery. A team effort from gastroenterologists, surgeons, and radiologists is vital.
In summary, GI bleeding is a serious cause of acute blood loss anemia that needs quick action. By knowing where the bleeding starts and using the right treatments, we can help patients better.
Gynecological Causes of Severe Anemia
Gynecological issues are a big reason for severe anemia in women. They affect their quality of life and health. We will look at the gynecological causes of anemia, focusing on those that lead to a lot of blood loss or affect hemoglobin levels.
Menorrhagia and Its Impact on Hemoglobin Levels
Menorrhagia is when menstrual bleeding is too heavy or lasts too long. It’s a common cause of iron deficiency anemia in women. The blood loss depletes iron stores, lowering hemoglobin production.
This condition affects women’s health and daily lives. It causes fatigue, weakness, and shortness of breath.
Key factors contributing to menorrhagia include:
- Hormonal imbalances
- Uterine fibroids
- Endometriosis
- Coagulation disorders
Postpartum Hemorrhage and Acute Anemia
Postpartum hemorrhage (PPH) is a leading cause of acute anemia in new mothers. PPH is when a woman loses more than 500 mL of blood after delivery. This can quickly lead to severe anemia if not managed right away.
The sudden blood loss can cause a quick drop in hemoglobin levels. This puts the mother at risk of hypovolemic shock and other complications.
Risk factors for PPH include:
- Prolonged labor
- Multiple gestations
- Previous history of PPH
- Coagulopathy
Gynecological Malignancies and Chronic Blood Loss
Gynecological malignancies, like cervical, endometrial, and ovarian cancers, can cause chronic blood loss. This leads to anemia. The irregular bleeding from these cancers may not always be recognized as a symptom, delaying diagnosis and treatment.
Common symptoms of gynecological malignancies include:
- Abnormal vaginal bleeding
- Pelvic pain
- Abdominal bloating
Early detection and treatment of these conditions are key to managing anemia. They improve outcomes for women affected by these gynecological causes.
Trauma and Surgical Complications Leading to Anemia and Hypovolemia
Trauma or surgical issues can cause a lot of blood loss. This leads to anemia and hypovolemia. We will look into how these problems contribute to these conditions.
Traumatic Injuries
Trauma can damage blood vessels and organs, causing blood loss. This loss can make a person anemic, with too few red blood cells or hemoglobin.
People hurt in trauma need quick medical help. It’s important to spot blood loss early and act fast.
Post-Surgical Bleeding
After surgery, bleeding can also cause anemia and hypovolemia. It’s key to catch and manage this bleeding quickly.
Keeping an eye on patients for bleeding signs is vital. If needed, surgery or special agents can help stop the bleeding.
The Relationship Between Anemia and Hypovolemic Shock
Anemia and hypovolemia can cause hypovolemic shock. This is a serious condition where blood doesn’t circulate well. Knowing how anemia and hypovolemia lead to shock is important for care.
We’ll see how these conditions cause shock and why quick treatment is critical. Early action can greatly help patients.
| Cause | Effect on Blood Loss | Resulting Condition |
| Traumatic Injuries | Significant blood loss | Anemia and Hypovolemia |
| Post-Surgical Bleeding | Excessive bleeding | Anemia and Hypovolemia |
Clinical Manifestations of Acute Blood Loss Anemia
It’s important to know the signs of acute blood loss anemia to get treatment quickly. This condition can show mild to severe symptoms, based on how much and how fast blood is lost.
Immediate Signs and Symptoms
Right away, you might feel your heart beating faster, your blood pressure drop, and not pee as much. These are your body’s ways to try and keep up with the blood loss.
Key immediate signs include:
- Tachycardia: An increased heart rate to maintain cardiac output.
- Hypotension: Low blood pressure due to reduced blood volume.
- Decreased urine output: A sign of inadequate renal perfusion.
Compensatory Mechanisms and Their Clinical Presentation
The body tries to fight off acute blood loss by tightening blood vessels, beating the heart faster, and focusing blood flow on essential areas.
| Compensatory Mechanism | Clinical Presentation |
| Vasoconstriction | Pale or cool extremities |
| Increased Heart Rate | Tachycardia |
| Redirection of Blood Flow | Decreased peripheral pulses |
Complications Including Shock and Organ Dysfunction
Severe blood loss can cause shock and damage to organs. Hypovolemic shock happens when there’s not enough blood to circulate properly.
Potential complications include:
- Hypovolemic shock: Severe hypotension leading to inadequate organ perfusion.
- Organ dysfunction: Ischemia and dysfunction of vital organs such as the kidneys, heart, and brain.
Spotting these signs early is key to starting the right treatment and avoiding lasting harm.
Diagnostic Approach to Acute and Chronic Anemia
Diagnosing anemia, whether acute or chronic, needs a detailed approach. This includes many laboratory tests and imaging studies. We will look at how healthcare providers use these methods to identify and treat anemia well.
Laboratory Investigations: Beyond Hemoglobin Levels
Hemoglobin levels are key in diagnosing anemia. But, other lab tests give more insight into the cause and severity. Complete Blood Count (CBC) is a basic test that checks different blood parts, like red and white blood cells, and platelets.
The Reticulocyte Count is also important. It shows how the bone marrow is responding to anemia by counting young red blood cells. This test helps tell if the anemia is due to not making enough blood cells or making too many.
Imaging Studies for Locating Bleeding Sources
Imaging studies are vital for finding where bleeding is coming from in acute blood loss anemia. Endoscopy lets doctors see inside the gut to find ulcers or varices that might be bleeding.
Other tools like Computed Tomography (CT) scans and Angiography help find bleeding spots in different parts of the body. They guide doctors to where they need to act.
Specialized Tests for Underlying Chronic Conditions
For chronic anemia, specific tests are needed to find the cause. For example, Iron studies help spot iron deficiency anemia. Vitamin B12 and Folate levels are key for diagnosing megaloblastic anemia.
In some cases, a Bone Marrow Biopsy is needed to diagnose bone marrow problems. These tests are essential for creating a treatment plan that fits the patient’s needs.
Management Strategies for Patients with Acute on Chronic Anemia
Managing acute on chronic anemia needs a detailed plan. It covers both urgent and ongoing needs. This condition is tough because it deals with sudden blood loss and long-term anemia.
Emergency Interventions for Acute Blood Loss
When there’s sudden blood loss, acting fast is key. Fluid resuscitation and blood transfusions help. They keep blood flow and oxygen to important organs.
“The initial assessment and management of acute blood loss anemia should focus on identifying the source of bleeding and controlling it to prevent further blood loss.”
-Specialists highlight.
Blood Transfusion Protocols and Considerations
Blood transfusions are vital for managing acute on chronic anemia. Deciding to transfuse depends on the patient’s health, blood levels, and heart disease.
| Clinical Condition | Hemoglobin Threshold | Transfusion Decision |
| Stable, no cardiovascular disease | <7 g/dL | Consider transfusion |
| Unstable or cardiovascular disease | <8 g/dL | Likely to require transfusion |
Treatment of Underlying Chronic Anemia Causes
Fixing the cause of chronic anemia is key for long-term care. This might mean iron supplementation for iron deficiency, or erythropoiesis-stimulating agents for other types. Other treatments may also be needed.
Liv Hospital’s Approach to Anemia Management
At our hospital, we manage anemia in a detailed way. We handle sudden blood loss and long-term anemia. Our personnel works with patients to create plans that meet their needs and improve their quality of life
We combine emergency care, transfusion rules, and chronic disease management. Our goal is to give the best care to patients with acute-on-chronic anemia.
Conclusion: Importance of Prompt Recognition and Treatment
Prompt recognition and treatment of anemia are key to avoiding complications and improving patient health. We’ve talked about the causes of acute on chronic anemia and acute blood loss anemia. This shows why quick action is necessary.
Effective treatment of anemia starts with finding and fixing the root cause. This approach helps lower the risk of serious problems. It also makes life better for those with anemia.
The role of treatment is huge, as early medical help can greatly change patient results. At Liv Hospital, we focus on managing anemia well. We give patients the care and support they need to get better and live well.
Understanding anemia’s causes and effects helps us aim for better patient results and healthcare. Our emphasis on quick recognition and treatment shows our dedication to top-notch healthcare services.
FAQ
What is acute on chronic anemia?
Acute on chronic anemia happens when someone with long-term anemia suddenly gets worse. This can happen due to a sudden event like a lot of blood loss.
What are the causes of acute blood loss anemia?
Acute blood loss anemia can come from many sources. These include bleeding in the stomach, injuries, surgery problems, and issues like heavy periods or bleeding after childbirth.
How is anemia characterized in clinical practice?
Doctors use tests like the complete blood count (CBC) and hemoglobin levels to spot anemia. They also look at physical signs and the patient’s medical history.
What are the symptoms of acute blood loss anemia?
Symptoms include feeling dizzy, tired, and short of breath. In serious cases, it can lead to shock and problems with organs.
How is gastrointestinal bleeding managed in patients with anemia?
Doctors treat bleeding in the stomach by using endoscopies, medicines, and sometimes surgery. The goal is to stop the bleeding and help the body get more blood.
What is the role of blood transfusion in managing acute on chronic anemia?
Blood transfusions are key in treating acute on chronic anemia. They quickly increase red blood cells and help tissues get enough oxygen.
How does Liv Hospital approach to anemia management?
Liv Hospital uses a team of doctors to manage anemia. They find and treat the cause, and provide emergency care and support as needed.
What is the importance of prompt recognition and treatment of anemia?
Quick action is vital to avoid serious problems. It helps patients get better and reduces the risk of long-term health issues.
Can anemia due to hemorrhage be treated with iron supplements alone?
Iron supplements can help with iron deficiency anemia. But for anemia from bleeding, they might not be enough. Blood transfusions are often needed.
How does anemia of acute blood loss differ from chronic anemia?
Acute blood loss anemia is sudden and caused by a lot of blood loss. Chronic anemia takes longer to develop, often due to ongoing blood loss or other health issues.
References
7 Key Causes of Acute on Chronic Anemia and Acute Blood Loss Anemia
Acute anemia means a quick drop in red blood cells. This makes it hard for tissues and organs to get enough oxygen. Knowing what causes and shows these problems is key for the best care.
Our team at Liv Hospital is dedicated to exceptional care for anemia patients. We make sure to give full support and care for those with sudden drops in hemoglobin and signs of shock.
Key Takeaways
- Understanding the causes of acute on chronic anemia and acute blood loss anemia is key for quick action.
- Liv Hospital’s expert teams offer full care for complex anemia cases.
- Spotting signs of shock and sudden drops in hemoglobin is critical for the best results.
- Acute anemia can cause serious problems if not treated right away.
Understanding Anemia: Basic Concepts and Classifications
Anemia is when there are fewer red blood cells or less hemoglobin. It’s a big health issue that needs to be understood well. It can happen for many reasons, like chronic diseases, not getting enough nutrients, or losing blood suddenly.
We’ll look at what anemia is, starting with its definition and how it works. The World Health Organization says anemia is when hemoglobin is below 13 g/dL in men and 12 g/dL in non-pregnant women. This is how doctors know if someone has anemia.
Definition and Pathophysiology of Anemia
Anemia isn’t just one thing; it’s a group of problems with red blood cells. It can be because of not getting enough iron, vitamin B12, or folate. Knowing how these issues happen is key.
The body tries to make up for not having enough red blood cells in different ways. For example, it might pump more blood or make blood vessels wider. This helps get oxygen to important parts of the body when there’s not enough red blood cells.
How Anemia is Characterized in Clinical Practice
Doctors use tests and physical checks to find anemia. They look at a complete blood count (CBC) to see if hemoglobin and red blood cells are okay. These tests help figure out if someone has anemia and how bad it is.
Finding out why someone has anemia is also important. Doctors might do more tests like checking for iron or looking at the bone marrow. Knowing the cause helps decide how to treat it.
| Parameter | Male | Female (Non-Pregnant) |
| Hemoglobin (g/dL) | < 13 | < 12 |
| Hematocrit (%) | < 39 | < 36 |
Understanding anemia helps doctors diagnose and treat it better. This improves how patients do. Anemia and not having enough blood can be even harder to deal with, but with the right care, patients can get better.
Acute on Chronic Anemia: Definition and Mechanism
Chronic anemia can worsen quickly with an acute event. Acute on chronic anemia is a serious condition that needs quick action.
What Constitutes Chronic Anemia
Chronic anemia means your body has too little hemoglobin for a long time. It can happen due to not enough nutrients, chronic diseases, or genetic issues. For example, iron deficiency anemia is common and can be treated.
The National Institute of Health says knowing why you have it is key to managing it well.
How Acute Events Trigger Worsening of Chronic Anemia
Events like bleeding, surgery, or injury can make chronic anemia worse. These can quickly lower your hemoglobin levels, making things harder for you.
For instance, someone with iron deficiency anemia might see their hemoglobin drop fast after surgery or injury.
The Physiological Impact of Rapid Hemoglobin Decline
When hemoglobin drops quickly, it affects your body a lot. Your heart and lungs try to make up for it by working harder. But if it drops too much, your organs might not get enough oxygen.
This can lead to serious problems, like organ failure.
Doctors need to understand acute on chronic anemia to help patients quickly. Spotting the signs early helps prevent serious issues.
Acute Blood Loss Anemia: Criteria and Presentation
Acute blood loss anemia happens when hemoglobin levels drop quickly. This can be due to trauma, surgery, or bleeding in the gut. It’s a serious condition that needs quick diagnosis and treatment.
Diagnostic Criteria for Acute Blood Loss Anemia
To diagnose acute blood loss anemia, doctors look for a sudden drop in hemoglobin. They check for signs like a fast heart rate, low blood pressure, and hemoglobin levels under 7 g/dL. Medical studies show these signs help spot patients who need urgent care.
Clinical Signs of Significant Blood Loss
Signs of significant blood loss include a fast heart rate, low blood pressure, and less urine. People might also feel dizzy, weak, or have trouble breathing. Spotting these signs early is key to managing the condition well.
Differentiating Acute from Chronic Blood Loss
Telling acute from chronic blood loss is important for the right treatment. Acute blood loss happens suddenly, while chronic develops over time. Knowing the type of blood loss helps doctors plan the best treatment.
Doctors stress that early detection and action are vital for managing acute blood loss anemia. We’ll look at how to manage it in the next sections.
7 Key Causes of Acute on Chronic Anemia
It’s important to know what causes acute on chronic anemia. This condition happens when someone with chronic anemia gets worse suddenly. This can be very serious if not treated right away.
1. Gastrointestinal Bleeding in Patients with Chronic Anemia
Gastrointestinal bleeding is a big reason for acute on chronic anemia. People with chronic anemia face serious risks if they bleed in their gut. This bleeding can come from ulcers, varices, or tumors.
2. Heavy Menstruation Exacerbating Iron Deficiency
Heavy periods can make anemia worse, mainly in women with iron deficiency. Losing a lot of blood can make symptoms like tiredness and shortness of breath worse.
3. Trauma or Surgery in Chronically Anemic Patients
Getting hurt or having surgery can make anemia worse in people who are already anemic. The blood lost during these events can lower hemoglobin levels, making things harder.
4. Medication-Induced Bleeding in Chronic Kidney Disease
People with chronic kidney disease might take medicines that can cause bleeding. This bleeding can make their anemia worse.
The other three key causes include:
- Chronic Inflammatory Diseases: Diseases like rheumatoid arthritis can cause chronic inflammation. This can make anemia worse.
- Cancer and Its Treatment: Some cancers and their treatments can cause both chronic and acute anemia.
- Infections: Severe infections can cause acute anemia in people with chronic anemia.
It’s key for doctors to know these causes to manage acute on chronic anemia well. Understanding the triggers helps them find the right treatments to help patients.
Gastrointestinal Bleeding: A Leading Cause of Acute Blood Loss
Gastrointestinal bleeding can quickly cause acute blood loss anemia, a serious condition. It’s a major medical emergency that can come from different parts of the GI tract.
We know that GI bleeding can be divided by where it starts in the GI tract. Knowing this helps us diagnose and treat it better.
Upper GI Sources: Ulcers, Varices, and Erosions
Upper GI bleeding often comes from peptic ulcers, varices, and mucosal erosions. Peptic ulcers are usually caused by Helicobacter pylori or NSAIDs. Varices are big veins in the esophagus that bleed easily. Erosions are small lesions that can also bleed a lot.
To manage upper GI bleeding, we first stabilize the patient. Then, we use endoscopy to find and possibly treat the bleeding source.
Lower GI Sources: Diverticulosis, Hemorrhoids, and Malignancies
Lower GI bleeding can come from diverticulosis, hemorrhoids, and cancers. Diverticulosis is when small pouches in the colon wall bleed. Hemorrhoids are swollen veins in the anus that bleed during bowel movements. Cancers can also cause GI bleeding.
To diagnose lower GI bleeding, we use clinical exams, imaging, and endoscopy. These help find where the bleeding is and how bad it is.
Management Approaches for GI Bleeding
Managing GI bleeding includes starting with resuscitation, finding the bleeding source, and treating it. Endoscopy is key for both finding and fixing the problem.
For severe bleeding, we might need more treatments like angiographic embolization or surgery. A team effort from gastroenterologists, surgeons, and radiologists is vital.
In summary, GI bleeding is a serious cause of acute blood loss anemia that needs quick action. By knowing where the bleeding starts and using the right treatments, we can help patients better.
Gynecological Causes of Severe Anemia
Gynecological issues are a big reason for severe anemia in women. They affect their quality of life and health. We will look at the gynecological causes of anemia, focusing on those that lead to a lot of blood loss or affect hemoglobin levels.
Menorrhagia and Its Impact on Hemoglobin Levels
Menorrhagia is when menstrual bleeding is too heavy or lasts too long. It’s a common cause of iron deficiency anemia in women. The blood loss depletes iron stores, lowering hemoglobin production.
This condition affects women’s health and daily lives. It causes fatigue, weakness, and shortness of breath.
Key factors contributing to menorrhagia include:
- Hormonal imbalances
- Uterine fibroids
- Endometriosis
- Coagulation disorders
Postpartum Hemorrhage and Acute Anemia
Postpartum hemorrhage (PPH) is a leading cause of acute anemia in new mothers. PPH is when a woman loses more than 500 mL of blood after delivery. This can quickly lead to severe anemia if not managed right away.
The sudden blood loss can cause a quick drop in hemoglobin levels. This puts the mother at risk of hypovolemic shock and other complications.
Risk factors for PPH include:
- Prolonged labor
- Multiple gestations
- Previous history of PPH
- Coagulopathy
Gynecological Malignancies and Chronic Blood Loss
Gynecological malignancies, like cervical, endometrial, and ovarian cancers, can cause chronic blood loss. This leads to anemia. The irregular bleeding from these cancers may not always be recognized as a symptom, delaying diagnosis and treatment.
Common symptoms of gynecological malignancies include:
- Abnormal vaginal bleeding
- Pelvic pain
- Abdominal bloating
Early detection and treatment of these conditions are key to managing anemia. They improve outcomes for women affected by these gynecological causes.
Trauma and Surgical Complications Leading to Anemia and Hypovolemia
Trauma or surgical issues can cause a lot of blood loss. This leads to anemia and hypovolemia. We will look into how these problems contribute to these conditions.
Traumatic Injuries
Trauma can damage blood vessels and organs, causing blood loss. This loss can make a person anemic, with too few red blood cells or hemoglobin.
People hurt in trauma need quick medical help. It’s important to spot blood loss early and act fast.
Post-Surgical Bleeding
After surgery, bleeding can also cause anemia and hypovolemia. It’s key to catch and manage this bleeding quickly.
Keeping an eye on patients for bleeding signs is vital. If needed, surgery or special agents can help stop the bleeding.
The Relationship Between Anemia and Hypovolemic Shock
Anemia and hypovolemia can cause hypovolemic shock. This is a serious condition where blood doesn’t circulate well. Knowing how anemia and hypovolemia lead to shock is important for care.
We’ll see how these conditions cause shock and why quick treatment is critical. Early action can greatly help patients.
| Cause | Effect on Blood Loss | Resulting Condition |
| Traumatic Injuries | Significant blood loss | Anemia and Hypovolemia |
| Post-Surgical Bleeding | Excessive bleeding | Anemia and Hypovolemia |
Clinical Manifestations of Acute Blood Loss Anemia
It’s important to know the signs of acute blood loss anemia to get treatment quickly. This condition can show mild to severe symptoms, based on how much and how fast blood is lost.
Immediate Signs and Symptoms
Right away, you might feel your heart beating faster, your blood pressure drop, and not pee as much. These are your body’s ways to try and keep up with the blood loss.
Key immediate signs include:
- Tachycardia: An increased heart rate to maintain cardiac output.
- Hypotension: Low blood pressure due to reduced blood volume.
- Decreased urine output: A sign of inadequate renal perfusion.
Compensatory Mechanisms and Their Clinical Presentation
The body tries to fight off acute blood loss by tightening blood vessels, beating the heart faster, and focusing blood flow on essential areas.
| Compensatory Mechanism | Clinical Presentation |
| Vasoconstriction | Pale or cool extremities |
| Increased Heart Rate | Tachycardia |
| Redirection of Blood Flow | Decreased peripheral pulses |
Complications Including Shock and Organ Dysfunction
Severe blood loss can cause shock and damage to organs. Hypovolemic shock happens when there’s not enough blood to circulate properly.
Potential complications include:
- Hypovolemic shock: Severe hypotension leading to inadequate organ perfusion.
- Organ dysfunction: Ischemia and dysfunction of vital organs such as the kidneys, heart, and brain.
Spotting these signs early is key to starting the right treatment and avoiding lasting harm.
Diagnostic Approach to Acute and Chronic Anemia
Diagnosing anemia, whether acute or chronic, needs a detailed approach. This includes many laboratory tests and imaging studies. We will look at how healthcare providers use these methods to identify and treat anemia well.
Laboratory Investigations: Beyond Hemoglobin Levels
Hemoglobin levels are key in diagnosing anemia. But, other lab tests give more insight into the cause and severity. Complete Blood Count (CBC) is a basic test that checks different blood parts, like red and white blood cells, and platelets.
The Reticulocyte Count is also important. It shows how the bone marrow is responding to anemia by counting young red blood cells. This test helps tell if the anemia is due to not making enough blood cells or making too many.
Imaging Studies for Locating Bleeding Sources
Imaging studies are vital for finding where bleeding is coming from in acute blood loss anemia. Endoscopy lets doctors see inside the gut to find ulcers or varices that might be bleeding.
Other tools like Computed Tomography (CT) scans and Angiography help find bleeding spots in different parts of the body. They guide doctors to where they need to act.
Specialized Tests for Underlying Chronic Conditions
For chronic anemia, specific tests are needed to find the cause. For example, Iron studies help spot iron deficiency anemia. Vitamin B12 and Folate levels are key for diagnosing megaloblastic anemia.
In some cases, a Bone Marrow Biopsy is needed to diagnose bone marrow problems. These tests are essential for creating a treatment plan that fits the patient’s needs.
Management Strategies for Patients with Acute on Chronic Anemia
Managing acute on chronic anemia needs a detailed plan. It covers both urgent and ongoing needs. This condition is tough because it deals with sudden blood loss and long-term anemia.
Emergency Interventions for Acute Blood Loss
When there’s sudden blood loss, acting fast is key. Fluid resuscitation and blood transfusions help. They keep blood flow and oxygen to important organs.
“The initial assessment and management of acute blood loss anemia should focus on identifying the source of bleeding and controlling it to prevent further blood loss.”
-Specialists highlight.
Blood Transfusion Protocols and Considerations
Blood transfusions are vital for managing acute on chronic anemia. Deciding to transfuse depends on the patient’s health, blood levels, and heart disease.
| Clinical Condition | Hemoglobin Threshold | Transfusion Decision |
| Stable, no cardiovascular disease | <7 g/dL | Consider transfusion |
| Unstable or cardiovascular disease | <8 g/dL | Likely to require transfusion |
Treatment of Underlying Chronic Anemia Causes
Fixing the cause of chronic anemia is key for long-term care. This might mean iron supplementation for iron deficiency, or erythropoiesis-stimulating agents for other types. Other treatments may also be needed.
Liv Hospital’s Approach to Anemia Management
At our hospital, we manage anemia in a detailed way. We handle sudden blood loss and long-term anemia. Our personnel works with patients to create plans that meet their needs and improve their quality of life
We combine emergency care, transfusion rules, and chronic disease management. Our goal is to give the best care to patients with acute-on-chronic anemia.
Conclusion: Importance of Prompt Recognition and Treatment
Prompt recognition and treatment of anemia are key to avoiding complications and improving patient health. We’ve talked about the causes of acute on chronic anemia and acute blood loss anemia. This shows why quick action is necessary.
Effective treatment of anemia starts with finding and fixing the root cause. This approach helps lower the risk of serious problems. It also makes life better for those with anemia.
The role of treatment is huge, as early medical help can greatly change patient results. At Liv Hospital, we focus on managing anemia well. We give patients the care and support they need to get better and live well.
Understanding anemia’s causes and effects helps us aim for better patient results and healthcare. Our emphasis on quick recognition and treatment shows our dedication to top-notch healthcare services.
FAQ
What is acute on chronic anemia?
Acute on chronic anemia happens when someone with long-term anemia suddenly gets worse. This can happen due to a sudden event like a lot of blood loss.
What are the causes of acute blood loss anemia?
Acute blood loss anemia can come from many sources. These include bleeding in the stomach, injuries, surgery problems, and issues like heavy periods or bleeding after childbirth.
How is anemia characterized in clinical practice?
Doctors use tests like the complete blood count (CBC) and hemoglobin levels to spot anemia. They also look at physical signs and the patient’s medical history.
What are the symptoms of acute blood loss anemia?
Symptoms include feeling dizzy, tired, and short of breath. In serious cases, it can lead to shock and problems with organs.
How is gastrointestinal bleeding managed in patients with anemia?
Doctors treat bleeding in the stomach by using endoscopies, medicines, and sometimes surgery. The goal is to stop the bleeding and help the body get more blood.
What is the role of blood transfusion in managing acute on chronic anemia?
Blood transfusions are key in treating acute on chronic anemia. They quickly increase red blood cells and help tissues get enough oxygen.
How does Liv Hospital approach to anemia management?
Liv Hospital uses a team of doctors to manage anemia. They find and treat the cause, and provide emergency care and support as needed.
What is the importance of prompt recognition and treatment of anemia?
Quick action is vital to avoid serious problems. It helps patients get better and reduces the risk of long-term health issues.
Can anemia due to hemorrhage be treated with iron supplements alone?
Iron supplements can help with iron deficiency anemia. But for anemia from bleeding, they might not be enough. Blood transfusions are often needed.
How does anemia of acute blood loss differ from chronic anemia?
Acute blood loss anemia is sudden and caused by a lot of blood loss. Chronic anemia takes longer to develop, often due to ongoing blood loss or other health issues.
References
- Best Practice BMJ: Anemia of chronic disease – Symptoms, diagnosis and treatment. BMJ Best Practice. https://bestpractice.bmj.com/topics/en-us/95




































