Last Updated on November 17, 2025 by Ugurkan Demir

If you’re looking for the right dr for blood clots, it’s important to know who specializes in treating them. Getting a blood clot diagnosis can be worrying, but finding the right expert ensures safe and effective care.
A hematologist is the main dr for blood clots. They specialize in diagnosing and managing conditions like deep vein thrombosis (DVT) and pulmonary embolism (PE). At Liv Hospital, we make sure patients get personalized treatment from qualified specialists who understand every aspect of blood clot care.
When you meet your dr for blood clots, ask about your risk factors, treatment options, and long-term prevention. For trusted information on DVT, visit the Mayo Clinic’s DVT page to learn more about how these conditions are treated.
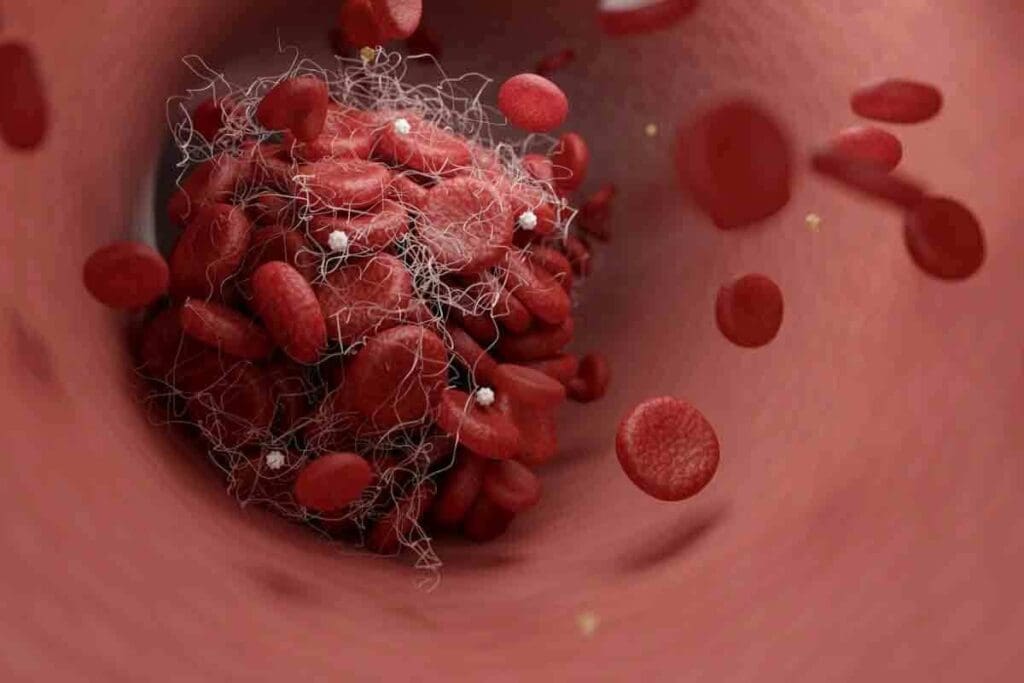
Blood clots can form in different parts of the body. They can lead to serious health issues like deep vein thrombosis (DVT) and pulmonary embolism (PE). These conditions are dangerous and need quick medical help.
DVT happens when a blood clot forms in the deep veins, usually in the legs. Symptoms include swelling, pain, and discoloration. If not treated, DVT can cause serious problems.
PE occurs when a clot travels to the lungs and blocks blood flow. It’s a life-threatening condition that needs immediate medical care. Symptoms include shortness of breath, chest pain, and a fast heart rate.
Several factors can increase the risk of blood clots. These include genetic predisposition, staying immobile for a long time, and certain medical conditions like cancer or heart disease. Knowing these risk factors is key to preventing blood clots.
It’s important to recognize the warning signs of blood clots. These include sudden swelling, pain, or trouble breathing. If you experience these symptoms, seek medical help right away.
| Condition | Symptoms | Dangers |
| DVT | Swelling, pain, discoloration | Clot can break loose, leading to PE |
| PE | Shortness of breath, chest pain, rapid heart rate | Life-threatening; can cause death |

Hematologists are experts in handling blood clotting disorders. They are key in diagnosing and managing blood clot conditions.
Hematologists know a lot about blood and its disorders. They can handle both bleeding and clotting issues. This makes them the top choice for blood clot problems.
Key areas of expertise for hematologists include:
Hematologists have a lot of training in internal medicine and hematology. Their education usually includes:
| Degree | Field of Study | Typical Duration |
| MD or DO | Medicine | 4 years |
| Residency | Internal Medicine | 3 years |
| Fellowship | Hematology | 2-3 years |
Hematologists are very important in managing clotting disorders. They work with patients to understand their condition and create a treatment plan. They also keep track of how the patient is doing.
Their role is not just about treatment but also education and preventive care. By knowing the causes of clotting disorders, hematologists can give personalized care to their patients.
Treating blood clots often needs a team effort. Doctors beyond hematologists play key roles. They help give patients the care they need.
Vascular surgeons focus on the vascular system. They treat blood clots in veins and arteries. They can remove clots through surgery.
They use both surgery and less invasive methods. This helps keep blood flowing and stops more clots. They work with other doctors to find the best treatment.
Key procedures performed by vascular surgeons include:
Interventional radiologists use imaging to guide treatments. They are experts in treating blood clots with minimal risk. They use advanced imaging for precise treatment.
They are key in complex cases. Their skills help patients who don’t respond to standard treatments.
Cardiologists and pulmonologists treat heart and lung clots. Cardiologists handle heart-related clots. Pulmonologists treat lung clots.
They work with hematologists for targeted care. Their input is critical for patients with serious clots.
Primary care physicians may start treating blood clots. They handle simple cases. They guide on medication and watch the patient’s health.
If the case gets complex, they refer patients to specialists. Specialists provide further evaluation and treatment.
To find out what’s causing clotting disorders, doctors do a few things. They check the body, run tests, and use imaging studies. This way, they can figure out why clotting is happening and how to treat it.
The first step is an initial check-up and physical exam. The doctor will look over your medical history and ask about your symptoms. They will also do a physical exam to see if there are any signs of clotting, like swelling or redness.
Key components of the initial assessment include:
Blood tests are very important for finding clotting disorders. These tests check how well the blood clots and can spot problems.
Common blood tests used in diagnosis include:
Imaging studies help doctors see blood clots and where they are. They use ultrasound, CT scans, and MRIs for this.
Each imaging modality has its advantages:
| Imaging Modality | Advantages |
| Ultrasound | Non-invasive, quick, and cost-effective |
| CT Scans | High-resolution images, useful for detecting clots in deep veins |
| MRIs | Detailed images, useful for diagnosing clots in complex cases |
Genetic screening might be suggested for some clotting disorders. It looks for genetic changes that can lead to blood clots.
“Genetic screening can help identify individuals at risk of hereditary clotting disorders, allowing for early intervention and preventive measures.”
By using these methods together, doctors can accurately diagnose clotting disorders. They can then create treatment plans that fit each patient’s needs.
When you have blood clots, you need a treatment plan that fits your situation. It’s important to manage blood clots well to avoid more problems and prevent them from coming back.
Anticoagulant medications are key in treating blood clots. They stop the clot from growing and help prevent new ones. Common ones are warfarin, apixaban, rivaroxaban, and dabigatran.
| Medication | Use | Monitoring Required |
| Warfarin | Long-term anticoagulation | Yes, regular INR checks |
| Apixaban | Prevention of stroke and systemic embolism | No routine monitoring |
| Rivaroxaban | Treatment of DVT and PE | No routine monitoring |
| Dabigatran | Prevention of stroke and systemic embolism | No routine monitoring |
Thrombolytic therapy is for severe blood clots, like big DVTs or PEs. It uses drugs to break down the clot.
Key considerations for thrombolytic therapy include:
Surgery is for cases where other treatments don’t work. It might include removing the clot or putting in a vena cava filter.
Surgical options are considered based on:
Stopping blood clots from coming back is key. This includes staying active, keeping a healthy weight, and not sitting too long.
Additional preventive measures may involve:
When you have Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE), finding the right doctor is key. These conditions need special care. The right doctor can greatly improve your health.
If you’re diagnosed with DVT or PE, your primary care doctor might send you to a specialist. Doctors like hematologists or vascular surgeons are experts in these areas. You should see a specialist if your condition is serious, if you’re facing complications, or if your primary doctor suggests it.
When looking at a doctor’s experience with blood clots, check their qualifications, experience with similar cases, and patient outcomes. Ask questions like: How many patients with DVT or PE have you treated? What treatments do you usually use? Are you current with the latest research and guidelines?
It’s important to know your insurance when looking for specialist care. Make sure your insurance covers the specialist’s services and understand any costs. Some plans need a referral from your primary doctor. It’s vital to clear up these details to avoid surprise medical bills.
For complex or severe DVT or PE cases, getting a second opinion is wise. A second opinion can give you more insight into your condition and treatment options. It can also give you peace of mind and help you make better decisions about your care. Don’t be afraid to ask your doctor if they think a second opinion is a good idea.
Getting a blood clot diagnosis is just the start. It’s key to ask your hematologist the right questions. This helps you understand your condition fully. You’ll learn about the cause of your blood clots, if there’s an underlying condition, and your risk for future clots. Also, you’ll find out if your family members should be tested.
It’s important to ask your hematologist about the cause of your blood clots. Was it from a specific event or an underlying condition? Your hematologist can tell if it’s a temporary issue or a chronic problem.
Common causes of blood clots include:
Some conditions can raise your risk of blood clots. Your hematologist can check for conditions like Factor V Leiden or Antiphospholipid Syndrome. Knowing about these can help you understand your diagnosis better.
Knowing your risk for future clots is key to managing your condition. Your hematologist can assess your risk based on your history, genetics, and lifestyle. Ask about ways to lower your risk, like lifestyle changes or medications.
| Risk Factor | Description | Preventive Measures |
| Family History | Having a first-degree relative with a history of blood clots | Genetic testing, closer monitoring |
| Previous Clots | Having had a blood clot previously | Anticoagulant therapy, lifestyle modifications |
| Obesity | Being significantly overweight | Weight loss programs, exercise |
If you’ve had a blood clot, you might wonder if your family is at risk. Ask your hematologist if your family should be tested for clotting disorders. This is very important if you have a genetic condition that could be passed down.
Talking about your family history with your hematologist can give you insights into risks and precautions for your relatives.
When you’re diagnosed with blood clots, knowing your treatment plan is key to getting better. Blood clot treatment varies. It depends on the type of clot, where it is, and your health.
How long you’ll be treated is a big worry for many. Treatment time can change a lot. Anticoagulant medications are often used to stop the clot from getting bigger and to prevent new ones.
For example, people with Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE) might take these meds for 3 to 6 months or more. This depends on their risk factors and any health conditions they have.
“The length of anticoagulation therapy should be tailored to each patient. It depends on their risk of getting another clot and their risk of bleeding.”
Dr. Jane Smith, Hematologist
| Condition | Typical Treatment Duration | Medication Protocol |
| DVT | 3-6 months | Anticoagulants (e.g., Warfarin, Rivaroxaban) |
| PE | 3-6 months or longer | Anticoagulants (e.g., Apixaban, Dabigatran) |
It’s important to handle side effects of anticoagulant meds well. Common side effects include bleeding risks. These can be from small bruises to serious bleeding.
Patients should watch their health closely and tell their doctor about any bleeding or bruising. Blood tests are done regularly to check the meds’ effectiveness and to lower the risk of bad side effects.
It’s often needed to avoid activities to prevent the clot from moving and causing more problems. How long and what activities to avoid depend on the clot’s severity and your health.
Usually, doctors tell patients to avoid strenuous activities and heavy lifting for a while. As you get better, these limits can be eased.
Changing your lifestyle is key in managing blood clots and stopping them from coming back. Patients are often told to quit smoking, keep a healthy weight, and stay hydrated.
It’s important to keep up with regular check-ups with your doctor. This helps track your progress and adjust your treatment as needed.
Recovery from DVT or PE doesn’t stop after treatment. It’s important to keep getting care to prevent more problems. This care helps manage any ongoing issues.
Regular check-ups are key to long-term care. How often you see your doctor depends on your situation. At first, you might see them every few months. Later, it might be less often as you get better.
At these visits, your doctor checks how you’re doing. They look for any new problems and change your treatment if needed. It’s also a chance to talk about any worries or symptoms you have.
Tests are important for managing DVT and PE long-term. They include blood tests and imaging to check for clots. These tests help find any new issues early.
It’s important to understand your test results. Blood tests show if your medicine is working. Imaging studies check if clots are getting better.
| Test Type | Purpose | Frequency |
| Blood Work | Monitor Anticoagulation Therapy | Regularly, as advised by healthcare provider |
| Imaging Studies (e.g., Ultrasound, CT Scan) | Assess Clot Resolution | Initially and as necessary based on patient condition |
| D-dimer Test | Assess for Clot Presence | May be done periodically, specially if symptoms recur |
Some people may face ongoing issues after DVT or PE. These can include post-thrombotic syndrome (PTS) or chronic thromboembolic pulmonary hypertension (CTEPH). Handling these problems needs a detailed plan that might include medicine and lifestyle changes.
For example, people with PTS might wear compression stockings and do exercises. Those with CTEPH might need special drugs to manage their condition.
When to switch from a specialist to a primary care doctor depends on several things. It’s about how stable your condition is and if you can handle your care on your own. Usually, if you’ve had a simple case of DVT or PE and are on stable treatment, you can switch to primary care.
But, if you have a complex case or big complications, you might need to keep seeing specialists. It’s important to work with your healthcare team to figure out the best care plan for you.
Working with a hematologist or blood clot specialist is key for managing blood clots well. Together, patients get care that fits their needs perfectly.
A good partnership with a specialist helps patients understand their condition better. They learn about treatments and how to prevent blood clots. This teamwork leads to better health choices and outcomes.
When looking for a specialist, think about their skills, experience, and how they communicate. A specialist who listens and answers questions creates a supportive partnership. This helps patients manage their condition better.
Having a partnership with a blood clot specialist makes managing blood clots easier. It’s vital for the best health results and lowering the chance of future clotting problems.
A hematologist is usually the go-to doctor for blood clots. They specialize in blood disorders and clotting conditions.
Ask your hematologist about the cause of your blood clots. Find out if you have an underlying condition. Also, ask about your risk for future clots and tests for family members.
Doctors use several methods to diagnose clotting disorders. They start with initial assessments and physical exams. Then, they run coagulation panels and blood tests.
Imaging studies like ultrasound, CT scans, and MRIs are also used. Genetic screening helps identify hereditary clotting disorders.
Treatment options include anticoagulant medications and thrombolytic therapy for severe clots. Surgery may also be needed. Preventive measures help avoid future clots.
Treatment length varies based on your case, the type of clot, and its cause. Your doctor will guide you on the treatment duration.
Risk factors include genetic predisposition and recent surgery. Prolonged immobility, cancer, and certain medical conditions also increase your risk.
No, managing blood clots needs medical supervision. This includes monitoring tests and managing medication side effects. Lifestyle changes are also necessary.
Seek a specialist if you have severe symptoms or if your doctor recommends it. You may need complex care.
Follow-up appointment frequency depends on your condition and treatment. Your doctor will tell you how often to come back.
Lifestyle changes may include diet and exercise adjustments. Quitting smoking and other habits are also important. Your doctor will give you personalized advice.
Sometimes, your primary care physician can treat blood clots. But for complex or severe cases, a specialist like a hematologist may be needed.
Warning signs include sudden swelling, pain, or discoloration in a limb. Difficulty breathing or chest pain are also signs. Seek immediate medical attention if you experience these symptoms.
Medical News Today. Deep Vein Thrombosis: Diagnosis and Treatment.
https://www.medicalnewstoday.com/articles/deep-vein-thrombosis
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!