Last Updated on November 4, 2025 by mcelik

Compare which is worse—osteoarthritis or osteoporosis—and understand the key differences in osteoporosis vs osteoarthritis.
Nearly 53 million adults in the United States have arthritis, with osteoarthritis being very common. Osteoporosis affects about 10 million Americans, making it a big health issue. Both conditions affect the musculoskeletal system but in different ways.
Osteoarthritis mainly affects the joints, causing pain and stiffness. On the other hand, osteoporosis weakens bones, making them more likely to break.
It’s important to know the differences between these two conditions for the right treatment. This article will look at the unique features of osteoarthritis and osteoporosis. We’ll compare how they affect health and quality of life.
Bone and joint health are key to our ability to move and live well. As we get older, our bones and joints change. These changes can make them weaker and less functional.
Healthy bones are strong and dense, giving our bodies shape. Joints, where bones meet, are flexible and let us move. The health of bones and joints depends on each other, needing a balance of body processes.
“The skeletal system is a complex framework that not only provides support but also facilitates movement through its intricacy,” says a leading orthopedic specialist. This shows why keeping bones and joints healthy is so important.
Aging has a big impact on bone and joint health. Older bones are less dense and more likely to break. Joints may wear out, making it harder to move and raising the risk of osteoarthritis.
There are many wrong ideas about bone and joint health. For example, many think osteoarthritis and osteoporosis are just part of aging. They believe nothing can be done to stop or manage them.
But, changing your lifestyle and getting medical help can really help manage these conditions. Knowing the truth is key to taking care of our bones and joints.
“Prevention and early intervention are key to managing bone and joint health. By understanding the risks and taking proactive measures, individuals can significantly reduce their likelihood of developing severe bone and joint conditions.”

Osteoarthritis, also known as wear-and-tear arthritis, is a common joint condition. It happens when cartilage breaks down, causing joint inflammation and pain.
Osteoarthritis is a degenerative joint disease. It occurs when cartilage and bone break down. It’s a common arthritis type, affecting over 32.5 million adults in the U.S. It gets more common with age, affecting the elderly a lot.
Osteoarthritis damages cartilage, causing bones to rub against each other. This leads to pain, stiffness, and less mobility. It can also cause bone spurs and cysts in the joint.
The inflammation in joints can cause swelling and redness. As the disease gets worse, simple tasks become hard because of pain and stiffness.
Osteoarthritis can hit any joint, but it often affects the hands, knees, hips, and spine. Weight-bearing joints like the knees and hips are more at risk. They bear a lot of stress and strain.
Osteoporosis is a major health issue affecting millions globally. It makes bones weaker and more likely to break.
Osteoporosis is a bone disease that weakens bones. This makes them fragile and prone to fractures. The National Osteoporosis Foundation says about 10 million Americans have it.
Another 44 million have low bone density, which raises their risk. The condition gets more common with age, hitting many seniors hard.
It’s estimated that half of women and a quarter of men over 50 will break a bone due to osteoporosis.
Osteoporosis lowers bone density, making bones weak. This makes them break easily, even with small injuries. It often affects hips, spine, and wrists.
A DEXA scan measures bone density. It compares your bones to those of a healthy young adult. This gives a T-score that shows how healthy your bones are.
Hips, spine, and wrists are most at risk for osteoporotic fractures. Hip fractures can lead to disability and even death. Vertebral fractures cause back pain and loss of height.
Wrist fractures, though less severe, can also lower quality of life. Knowing which areas are most at risk helps prevent fractures.
Changing your lifestyle and getting medical help can reduce fracture risk.
Both osteoporosis and osteoarthritis affect bone health but in different ways. It’s important to know how they differ.
Osteoarthritis happens when cartilage in joints breaks down. This leads to bone-on-bone contact, causing pain and stiffness. Osteoporosis, on the other hand, makes bones weaker and more likely to break.
Osteoarthritis is caused by joint cartilage wear and tear. Osteoporosis is due to an imbalance in bone remodeling, where bone loss is greater than bone growth.
Osteoarthritis mainly affects joints, including cartilage, synovium, and subchondral bone. Osteoporosis, by contrast, weakens bones overall, making them more likely to fracture.
Both conditions get worse with age but affect different groups. Osteoarthritis is common in older adults due to wear and tear. Osteoporosis also worsens with age and is more common in postmenopausal women due to hormonal changes.
Key demographic differences include:
Yes, it’s possible to have both osteoporosis and osteoarthritis, often in older adults. This can make diagnosis and treatment more complex.
“The presence of comorbid conditions like osteoporosis and osteoarthritis requires a holistic treatment plan that addresses both conditions.”
Understanding the differences between osteoporosis and osteoarthritis is key to effective treatment, even when both conditions occur together.
Osteoarthritis develops from a mix of factors that harm joints over time. Knowing these causes is key for preventing and managing the condition.
Age is a major risk factor for osteoarthritis. As we age, the cartilage in our joints wears down. This can lead to osteoarthritis. Age-related wear and tear is a natural process, but its speed can be affected by other factors.
Genetics also play a big role in osteoarthritis. People with a family history of osteoarthritis are more likely to get it. Scientists are studying genetic predispositions to find markers for risk.
Being overweight is a big risk factor, mainly for joints like the knees and hips. Extra weight puts more stress on these joints, speeding up wear and tear. Keeping a healthy weight through diet and exercise can help lower this risk.
Joint injuries, like fractures or sprains, can raise the risk of osteoarthritis. Jobs that put a lot of strain on joints also increase this risk. For example, jobs that involve kneeling or heavy lifting can harm the knees or hips.
| Risk Factor | Description | Impact on Osteoarthritis Risk |
| Age | Natural wear and tear over time | High |
| Genetics | Family history of osteoarthritis | Moderate to High |
| Obesity | Excess weight on weight-bearing joints | High |
| Previous Injuries | Joint injuries or trauma | Moderate |
Knowing these risk factors helps people take steps to prevent osteoarthritis. By tackling risks like obesity and job-related hazards, people can lower their chances of getting osteoarthritis.
Many factors can increase the risk of osteoporosis. These include hormonal changes, lifestyle choices, and nutritional deficiencies. Knowing these risk factors is key to preventing and managing osteoporosis.
Hormonal changes, like the drop in estrogen during menopause, are big contributors to osteoporosis. Estrogen helps keep bones strong. When estrogen levels fall, bones can weaken fast. Menopause is a critical time for bone health. Women are more likely to get osteoporosis then because of the big drop in estrogen.
Not getting enough calcium and vitamin D is a big risk for osteoporosis. Calcium is key for strong bones, and vitamin D helps the body use calcium. Eating foods rich in these nutrients or taking supplements is important to prevent osteoporosis.
Our lifestyle choices also affect our bone health. Smoking and drinking too much alcohol can harm bones. Being inactive can also make bones weaker. Regular exercise, like weight-bearing activities, helps keep bones strong. Quitting smoking and drinking less can also lower the risk of osteoporosis.
Some medical conditions and medicines can raise the risk of osteoporosis. Conditions like hyperthyroidism and rheumatoid arthritis can hurt bone health. Long-term use of corticosteroids and some medicines can also cause bone loss. Knowing these risks helps manage and reduce their impact on bones.
| Risk Factor | Description | Impact on Bone Health |
| Hormonal Changes | Decrease in estrogen during menopause | Rapid loss of bone mass |
| Nutritional Deficiencies | Lack of calcium and vitamin D | Increased risk of osteoporosis |
| Lifestyle Factors | Smoking, excessive alcohol, inactivity | Weaker bones, increased risk |
| Medical Conditions | Hyperthyroidism, rheumatoid arthritis | Affects bone density and health |
Knowing the symptoms of osteoarthritis is key for early diagnosis and treatment. This degenerative joint disease shows through various symptoms that can affect one’s life quality.
The first signs of osteoarthritis include joint pain and stiffness, mainly after rest. People might also hear a crunching sound when moving a joint, called crepitus.
As osteoarthritis gets worse, symptoms intensify. This can lead to more pain, less mobility, and complications. Advanced stages may cause bone spurs and more cartilage loss.
Common complications include:
Osteoarthritis gets worse over time if not treated properly. The speed of progression varies, depending on age, genetics, and lifestyle.
The progression can be characterized by periods of stability punctuated by exacerbations.
Osteoarthritis symptoms can make daily tasks hard. Even simple actions like walking or climbing stairs can be tough due to pain and stiffness.
Managing these effects includes physical therapy, using aids, and changing daily routines to ease joint strain.
Osteoporosis is often called the “silent disease” because it can go unnoticed until a serious event happens. This event is usually a fracture. People might not know they have osteoporosis until it’s too late.
In the early stages, osteoporosis doesn’t show symptoms. This makes it hard for people to know they have it until they break a bone.
“Osteoporosis is a condition that silently robs you of your bone density, leaving you vulnerable to fractures.” This quote shows how sneaky osteoporosis is. It’s why we need to be aware and take steps to prevent it.
Even though osteoporosis itself doesn’t show symptoms, the risk of breaking bones goes up as bones get weaker. Look out for these signs:
Osteoporosis gets worse as bones lose more mass than they gain. This weakens bones and raises the risk of fractures.
As it gets worse, the risk of fractures can really hurt your quality of life. It can make moving around harder and limit your freedom.
If osteoporosis isn’t treated, it can cause big problems later on. These include:
Getting diagnosed and treated early is key. It helps avoid these problems and keeps your life quality high.
Diagnosing bone and joint conditions like osteoarthritis and osteoporosis needs a mix of clinical checks and tests. Getting the diagnosis right is key to making good treatment plans.
Tests for osteoarthritis help check joint health and find out how much damage there is.
Osteoporosis diagnosis looks at bone density and the risk of fractures.
| Diagnostic Test | Osteoarthritis | Osteoporosis |
| X-rays | Joint space narrowing, bone spurs | Vertebral fractures |
| DXA Scan | Not typically used | Bone mineral density |
| MRI | Soft tissue damage, early joint changes | Not typically used |
It’s hard to tell osteoarthritis apart from osteoporosis because their symptoms can be similar. Sometimes, people have both conditions.
Key challenges include:
Osteoarthritis treatment has grown, giving patients many ways to feel better. The right treatment depends on how bad the condition is, the patient’s health, and what they prefer.
Medicines are key in fighting osteoarthritis symptoms. Over-the-counter pain relievers like acetaminophen and ibuprofen help with pain and swelling. For severe cases, prescription medications like corticosteroids or hyaluronic acid injections might be suggested.
Physical therapy is vital in treating osteoarthritis. It includes exercises made just for you to move your joints better, make the muscles stronger, and lessen pain. Low-impact exercises like swimming, cycling, or tai chi are good choices.
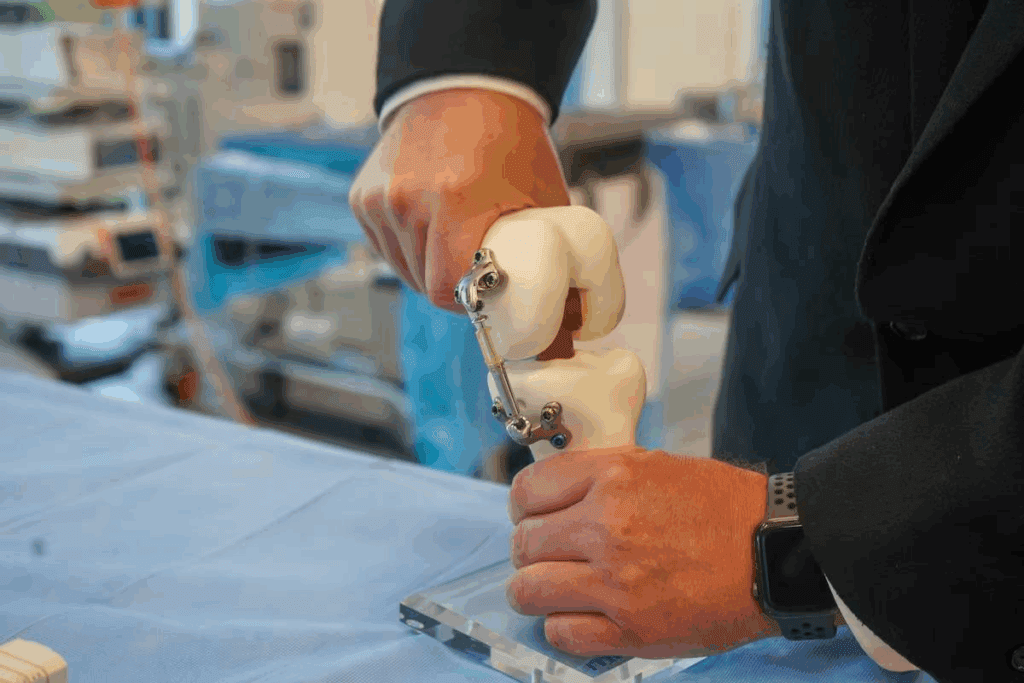
If other treatments don’t work, surgical interventions might be needed. Joint replacement surgery is often done for hips and knees with severe osteoarthritis. Other surgeries include arthroscopy to fix damaged joints or osteotomy to adjust the joint’s alignment.
Many patients also try alternative and complementary therapies. These can be acupuncture, massage, or supplements like glucosamine and chondroitin. While their effectiveness can differ, they might help some people feel better.
It’s important for patients to talk to their doctor to create a treatment plan that fits their needs.
Managing osteoporosis needs a mix of medicine, lifestyle changes, and prevention. The aim is to slow bone loss, lower fracture risk, and keep mobility and quality of life high.
Bisphosphonates are key drugs for osteoporosis. They stop bone loss by blocking bone resorption. This increases bone mass and lowers fracture risk. Alendronate and risedronate are examples. Other options include:
Calcium and vitamin D are key for bone health. Supplements fill nutritional gaps, helping those with dietary needs or increased requirements.
Calcium is vital for bone mineralization. Vitamin D boosts calcium absorption and bone health. It’s essential to keep both nutrients at the right levels for managing osteoporosis.
Weight-bearing exercise, like walking or resistance training, strengthens bones and improves balance. This reduces fall risk. Flexibility and strength exercises are also good.
To prevent falls, remove home hazards, improve lighting, and use assistive devices when needed.
Hormone replacement therapy (HRT) may help some, like postmenopausal women, by reducing bone loss. But, it’s important to weigh its risks and benefits.
Each osteoporosis treatment plan should fit the person, considering their health, risks, and preferences. Regular check-ups and plan adjustments are key for effective management.
Living with osteoarthritis or osteoporosis can really change a person’s life. Each disease brings its own set of challenges. These can affect how you feel and move, both physically and mentally.
Osteoarthritis mainly hurts the joints, causing pain and stiffness. This makes simple tasks hard, like walking or going up stairs. Osteoporosis, on the other hand, often goes unnoticed until a bone breaks. This can suddenly change how you move.
Osteoarthritis makes life tough by causing constant pain and limiting how you can move. It makes doing everyday things hard because of the pain.
Osteoporosis raises the risk of breaking bones, which can be deadly, mainly for older people. These breaks can lead to serious problems and even death. Osteoarthritis, while not deadly, can really hurt your quality of life. It can also lead to other health problems because you can’t move as well.
The future looks different for people with osteoarthritis. Some have mild symptoms, while others face big challenges. Osteoporosis, if not managed, can cause more breaks and health decline. It’s key to manage both well to improve your future.
| Condition | Primary Impact | Long-term Prognosis |
| Osteoarthritis | Chronic pain and reduced mobility | Variable, potentially significant disability |
| Osteoporosis | Increased risk of fractures | Potential for recurrent fractures and health decline |
Both osteoarthritis and osteoporosis can deeply affect your mind and social life. Chronic pain and not being able to move well can lead to sadness and feeling alone. Osteoporosis can make you anxious about breaking bones, which can also hurt your social life.
It’s important to understand these effects to give full care. This care should help both your body and mind.
Staying healthy and making lifestyle changes can help prevent osteoarthritis and osteoporosis. Knowing how to prevent these conditions can greatly reduce your risk.
Changing your lifestyle can help prevent osteoarthritis and osteoporosis. Regular exercise is key for keeping bones and joints healthy. Walking, swimming, and cycling are good choices.
Acting early is key in managing and preventing osteoarthritis and osteoporosis. Regular health check-ups can spot risk factors early.
| Condition | Early Intervention Strategies |
| Osteoarthritis | Physical therapy, pain management medication |
| Osteoporosis | Bisphosphonates, calcium and vitamin D supplements |
It’s important to know the warning signs of osteoarthritis and osteoporosis. Symptoms like persistent joint pain, decreased mobility, or a sudden fracture mean it’s time to see a doctor.
“Early diagnosis and treatment can significantly improve outcomes for individuals with osteoarthritis or osteoporosis,” says
.
When talking to a healthcare provider about osteoarthritis or osteoporosis, ask the right questions. Ask about the best treatments, lifestyle changes, and what to expect.
It’s important to know the difference between osteoarthritis and osteoporosis. This knowledge helps in managing these conditions better. It also improves your quality of life.
For those with osteoarthritis, managing pain and keeping joints mobile is key. Adopting healthy lifestyle choices is also important. On the other hand, osteoporosis requires focus on bone density. This includes getting enough calcium and vitamin D, exercising, and preventing falls.
Living a healthy lifestyle and getting medical help when needed can help a lot. Regular doctor visits and staying updated on treatments can greatly improve your health.
Being well-informed about bone and joint health is empowering. It helps you manage your condition, avoid complications, and live an active and fulfilling life. This is true even with the challenges of osteoarthritis or osteoporosis.
Osteoarthritis is a disease that affects the cartilage and joints. Osteoporosis is a condition that weakens bones, making them more likely to break.
Yes, it’s possible to have both conditions at once. They share some risk factors.
Symptoms include joint pain, stiffness, and limited mobility. These often affect the hands, hips, knees, and spine.
Osteoporosis might not show symptoms until a bone breaks. Some people may feel back pain, lose height, or have a hunched posture.
Doctors use medical history, physical exams, and imaging tests like X-rays or MRI. They might also check joint fluid.
Doctors use bone density tests, like DXA scans. They might also do vertebral fracture assessments.
Treatments include pain relievers, physical therapy, and lifestyle changes. Sometimes, surgery like joint replacement is needed.
Treatments include medications, supplements, and exercise. Fall prevention and hormone therapy might also be suggested.
Some risk factors can’t be changed. But, staying healthy, exercising, and avoiding joint stress can help prevent it.
Yes, a healthy lifestyle can prevent or delay osteoporosis. This includes a balanced diet, exercise, not smoking, and less alcohol.
Both can cause pain and limit mobility. They increase the risk of complications. The impact varies by individual and condition severity.
A healthy weight, regular exercise, and a balanced diet are key. Avoiding smoking and limiting alcohol also helps.
See a doctor for persistent pain or stiffness, a history of fractures, or concerns about your risk factors.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!