Last Updated on November 4, 2025 by mcelik
Back pain is a big problem worldwide, affecting millions. Many cases are due to herniated discs. A herniated disc can cause a lot of pain and discomfort, making people wonder about the best treatments. Learn about Hernia Disc Surgery Benefits and when it’s the best option for lasting relief.
Deciding if herniated disc surgery is needed depends on how bad the condition is. The decision to have surgery often depends on how much the herniated disc affects your life.
Key Takeaways
- Herniated discs are a common cause of back pain.
- Surgery is considered when the condition severely impacts daily life.
- Understanding the benefits of herniated disc surgery is key.
- The decision to undergo surgery depends on the condition’s severity.
- Exploring treatment options is essential for effective management.
Understanding Herniated Discs: Causes, Symptoms, and Impact on Quality of Life
Knowing the causes and symptoms of herniated discs is key to finding the right treatment. A herniated disc affects the spine, causing pain and changing daily life.
What Exactly Is a Herniated Disc?
A herniated disc happens when the soft center of a spinal disc bulges or leaks. This can press on nerves, causing symptoms.
Common Causes of Disc Herniation
Disc herniation can come from aging, injury, or strain. Heavy lifting, bending, or twisting can also raise the risk.
Recognizing Herniated Disc Symptoms
Symptoms include sharp pain, numbness, tingling, or muscle weakness. The severity and type depend on the disc’s location and the nerves involved.
Herniated discs can greatly affect a person’s life, making daily tasks hard and physical activities less enjoyable. Knowing about the condition is the first step to better treatment and outcomes.
Diagnosing a Herniated Disc: From Physical Examination to Advanced Imaging
To accurately diagnose a herniated disc, doctors use a mix of initial checks and advanced imaging. This detailed approach helps ensure patients get the right diagnosis. This is key to finding the best treatment.
Initial Clinical Assessment
The first step in diagnosing a herniated disc is a thorough clinical check. A healthcare professional will do a physical examination to assess the patient’s condition. This check may include:
- Looking at the patient’s medical history to find any conditions that might be causing symptoms.
- Checking the patient’s range of motion and flexibility to see if there are any pain points.
- Doing neurological tests to see if there’s nerve damage or compression.
Imaging Technologies Used for Diagnosis
While a physical exam gives valuable insights, imaging technologies are key in confirming a herniated disc diagnosis. The most used imaging methods are:
- Magnetic Resonance Imaging (MRI): MRI is the top choice for diagnosing herniated discs. It shows detailed images of the spine, helping doctors see the disc and how severe the herniation is.
- Computed Tomography (CT) scans: CT scans can also diagnose herniated discs, mainly when an MRI is not available or not suitable.
- X-rays: X-rays can help rule out other back pain causes like fractures or degenerative changes, even though they’re not as detailed as MRI or CT scans.
Determining the Severity of Disc Herniation
After diagnosing a herniated disc, figuring out how severe it is is key to treatment planning. The severity is based on the herniation size, location, and nerve compression level. This info helps doctors:
- Choose between non-surgical treatments and surgery.
- Create a treatment plan that fits the patient’s needs.
- Keep track of the condition’s progress and adjust the treatment as needed.
Knowing the diagnosis and severity of a herniated disc is vital for patients. It helps them decide if herniated disc surgery is effective for their case.
Conservative Treatment Approaches for Herniated Discs

Treatment for herniated discs often starts with non-surgical methods. These include rest, physical therapy, and medication. They aim to ease pain and improve life quality. These steps are usually the first choice, trying to avoid surgery.
Rest and Activity Modification
One key step is to change activities so as not to make the problem worse. This means cutting down on heavy lifting, bending, or twisting. Also, taking breaks to rest is important. Rest helps reduce swelling and pain.
Physical Therapy and Exercise Programs
Physical therapy is vital for herniated disc care. It includes exercises to strengthen the muscles around the spine. These exercises also improve flexibility and posture. You might do stretching, core exercises, and low-impact aerobics.
Medication Options for Pain Management
There are many ways to manage pain from herniated discs. Over-the-counter options like ibuprofen or acetaminophen are common. For more severe pain, doctors might prescribe muscle relaxants or oral steroids.
Combining rest, physical therapy, and the right medication can help a lot. Many people find relief without needing surgery.
When Does a Herniated Disc Require Surgical Intervention?
Knowing when a herniated disc needs surgical intervention is key. Most first try conservative treatments first. But sometimes surgery is needed.
Red Flags That Indicate Surgery May Be Necessary
Some symptoms and conditions are red flags for surgery. These include:
- Severe pain that doesn’t get better or gets worse
- Numbness or tingling in the hands or feet
- Muscle weakness that makes daily tasks hard
- Loss of bladder or bowel control
These signs point to neurological deficits needing quick medical help. If you see these symptoms, see a doctor fast.
Failed Conservative Treatment Scenarios
If conservative treatments don’t help, surgery might be next. This includes when:
- Physical therapy and exercise don’t improve things
- Pain meds don’t work
- Changing your lifestyle doesn’t help symptoms
Then, surgery could be a better way to fix the herniated disc and symptoms.
Neurological Deficits Requiring Immediate Attention

Neurological deficits from a herniated disc are serious. Signs like getting weaker, numbness, or tingling in limbs, or losing reflexes, mean nerve damage. In bad cases, cauda equina syndrome can cause paralysis and loss of bladder and bowel control. Quick surgery is often needed to avoid lasting harm.
In short, not all herniated discs need surgery. But some red flags and failed treatments mean it’s time for surgical intervention. Always talk to a healthcare professional to figure out the best treatment for you.
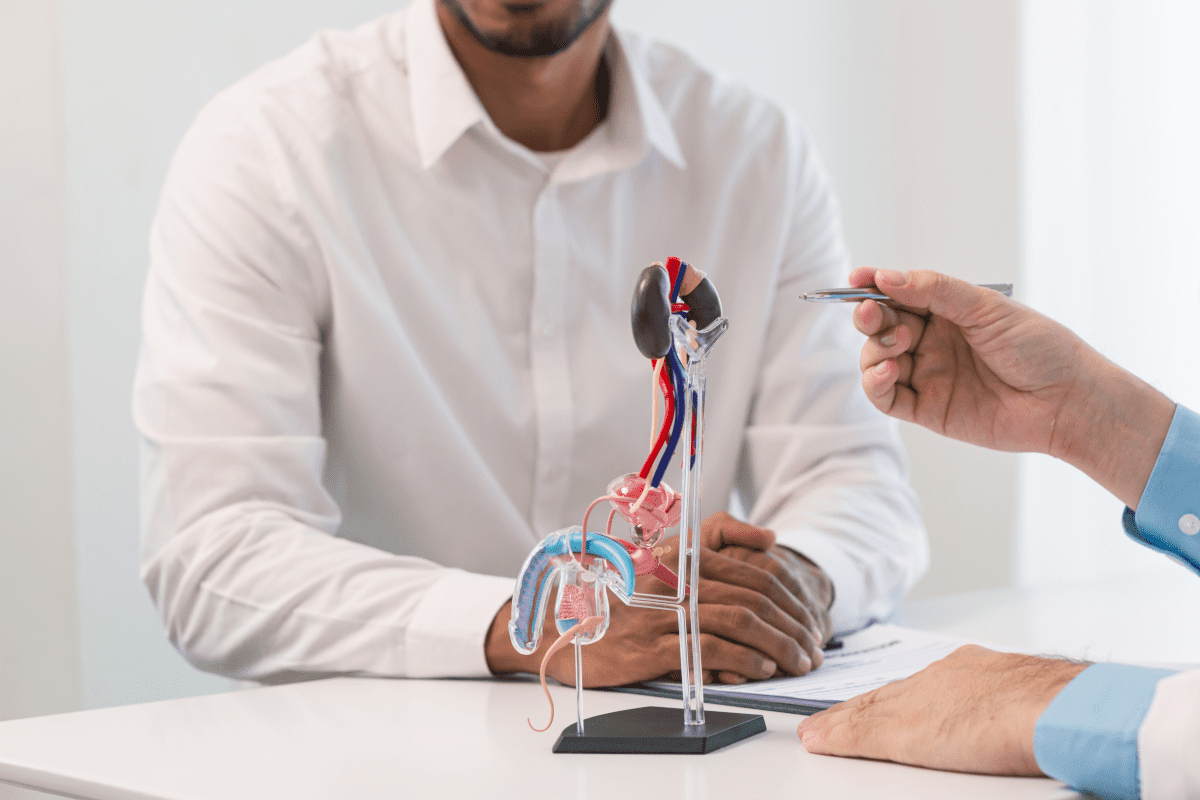
Types of Surgical Procedures for Herniated Discs
For those with herniated discs, several surgical options exist. These depend on the herniation’s severity and location. These procedures are chosen after other treatments have not worked well enough.
Microdiscectomy: The Gold Standard
Microdiscectomy is the top choice for herniated disc surgery. It’s a minimally invasive method. It removes the herniated disc part that’s pressing on a nerve.
The surgery is done under a microscope or with loupe magnification. This allows for precise removal of the disc material. It keeps the surrounding tissue safe.
Laminectomy and Laminotomy
Laminectomy and laminotomy involve removing part of the vertebra. A laminectomy removes a larger part of the lamina. Laminotomy removes a smaller part, often just a piece of the lamina.
These procedures are for those with severe nerve compression or spinal stenosis.
Minimally Invasive Techniques
Minimally invasive herniated disc surgery is becoming more popular. It’s known for less tissue damage, reduced bleeding, and quicker recovery times. These surgeries use smaller incisions and special tools to remove the herniated disc or decompress the nerve.
Spinal Fusion: When and Why It’s Considered
Spinal fusion is a more complex procedure. It joins two or more vertebrae together to stabilize the spine. It’s for those with severe disc degeneration, instability, or when other surgeries have failed.
The decision to undergo spinal fusion is made on a case-by-case basis. It considers the patient’s health, the extent of their condition, and the procedure’s benefits and risks.
In conclusion, the right surgery for a herniated disc depends on several factors. These include the herniation’s severity, the patient’s health, and the surgeon’s judgment. Knowing the different options helps patients make better decisions about their care.
Hernia Disc Surgery Benefits: What Improvement Can You Expect?
Many patients consider herniated disc surgery with the expectation of significant improvements in both pain relief and overall quality of life. Many turn to surgery after trying other treatments without success.
Immediate Pain Relief Outcomes
Immediate pain relief is a key benefit of hernia disc surgery. By taking out the herniated disc part that’s pressing on a nerve, surgery can quickly ease pain. This can greatly improve a patient’s daily life.
Research shows most patients see a big drop in pain after surgery. This quick relief can change their lives, letting them do things they couldn’t before because of pain.
Restoration of Neurological Function
Surgery can also bring back neurological function. A herniated disc can cause numbness, tingling, and weakness. By fixing this, surgery can help nerves work right again.
Patients often notice better feelings and strength after surgery. This makes it easier to do everyday tasks and enjoy physical activities.
Quality of Life Enhancements Post-Surgery
The mix of pain relief and restored function greatly improves quality of life. Patients can go back to work, hobbies, and social events without pain.
Being able to move more also leads to a healthier lifestyle. Many feel more confident and mentally better after surgery.
In summary, hernia disc surgery brings many benefits. These include quick pain relief, better nerve function, and a better life. These changes can greatly improve a patient’s life, letting them enjoy activities they couldn’t before.
Potential Risks and Complications of Herniated Disc Surgery
Herniated disc surgery has its own set of risks and complications. While it’s generally safe, knowing these risks is key for patients. This helps them make informed decisions about their treatment.
Common Surgical Complications
Surgical complications can happen during or after the surgery. These might include reactions to anesthesia, bleeding, or infection. Sometimes, the surgery might not fully fix the herniated disc, or it could come back.
| Complication | Description | Frequency |
| Infection | Bacterial infection at the surgical site | Rare |
| Bleeding | Excessive bleeding during or after surgery | Uncommon |
| Nerve Damage | Damage to the nerves surrounding the disc | Uncommon |
Infection and Bleeding Risks
Infection is a risk with any surgery, including herniated disc surgery. Signs of infection include fever, redness, and swelling at the surgical site. Bleeding can range from mild to severe. To reduce these risks, antibiotics and careful surgical techniques are used.
“The risk of infection after spine surgery is a significant concern, and measures such as antibiotic prophylaxis are critical in minimizing this risk.” –
Nerve Damage Concerns
Nerve damage is a possible complication of herniated disc surgery. This can cause numbness, weakness, or pain in the affected limb. Careful surgical planning and technique are essential in minimizing this risk. In some cases, nerve damage may be temporary, while in others, it can be permanent.
Anesthesia-Related Risks
Anesthesia is used during herniated disc surgery to ensure patient comfort. But anesthesia carries its own risks, including allergic reactions, respiratory complications, and, in rare cases, death. Anesthesiologists take precautions to minimize these risks, including thorough patient evaluation before surgery.
Understanding these risks and complications is vital for patients considering herniated disc surgery. By being informed, patients can better navigate their treatment options and make decisions that are right for them.
The Recovery Process After Herniated Disc Surgery
Herniated disc surgery is just the start. A full recovery is key to getting back to normal. This journey includes several stages, from right after surgery to physical therapy and getting back to daily life.
Immediate Post-Operative Period
The first part of recovery is all about rest and managing pain. Doctors tell patients to stay away from heavy lifting and bending. Pain medication helps with the discomfort. It’s important to follow the doctor’s advice to avoid problems.
Physical Therapy and Rehabilitation
Once the initial recovery is over, physical therapy becomes critical. A custom rehab plan helps regain strength and flexibility. Physical therapists teach exercises that aid in healing and prevent future issues.
Return to Work and Daily Activities Timeline
When to go back to work varies a lot. It depends on the surgery type, health, and job demands. Usually, people can start with light tasks in 4-6 weeks. But, harder activities might take 8-12 weeks. Always listen to your doctor and physical therapist for a safe comeback.
Success Rates and Outcomes of Herniated Disc Surgery
Patients need to know the success rates of herniated disc surgery. The surgery’s success can depend on several things. These include the type of surgery, the patient’s health, and how severe the herniation is.
Statistical Success Rates by Procedure Type
Different surgeries for herniated discs have different success rates. For example, microdiscectomy, a less invasive procedure, often works well. It can relieve pain and improve function in 80% to 95% of cases.
| Surgical Procedure | Success Rate | Complication Rate |
| Microdiscectomy | 80-95% | 1-5% |
| Laminectomy | 70-90% | 5-10% |
| Spinal Fusion | 60-85% | 10-20% |
Factors That Influence Surgical Outcomes
Many things can affect how well herniated disc surgery works. These include the patient’s age, health, how severe the herniation is, and any other health issues. Choosing the right patients before surgery is key to a good outcome.
Choosing the right patients means looking at how long symptoms have lasted, if there are any nerve problems, and if other treatments have helped.
Measuring “Success” in Spine Surgery
Success in spine surgery can be measured in several ways. These include how much pain is relieved, if the patient can move better, and if they’re happy with the results. Doctors use special questionnaires and tests to check these things.
- Pain relief
- Improved mobility
- Return to normal activities
- Patient satisfaction
Recurrence Rates and Secondary Surgeries
Some patients may need surgery again, with rates up to 20%. The need for a second surgery depends on the first surgery and whether there’s any leftover disc material.
The success of herniated disc surgery depends on many things. These include the surgery type and the patient’s health. Knowing these factors helps doctors and patients set realistic goals and improve results.
Surgery vs. Non-Surgical Treatment: A Comparative Analysis
Choosing between surgery and non-surgical treatment for a herniated disc is a big decision. You need to know about their effectiveness, risks, and outcomes. This helps you pick the best option for your health and needs.
Effectiveness for Pain Relief
Surgery is often seen as a quick fix for pain. Microdiscectomy, a common surgery for herniated discs, can greatly reduce pain in the short term. But non-surgical treatments like physical therapy and medication can also work well for many people. They might just take longer to show results.
How well non-surgical treatments work can vary a lot. It depends on how bad the herniation is, your overall health, and how well you follow the treatment plan. It’s important to think about the quick relief surgery offers versus the slower but possible non-surgical methods.
Recovery Time Comparisons
Recovery times are very different for surgery and non-surgical treatments. Surgery can take weeks to months to recover from, based on the surgery and how fast you heal. Non-surgical treatments take longer but are safer.
- Surgical recovery means rest and then rehab.
- Non-surgical recovery is about getting better slowly through therapy and lifestyle changes.
Long-term Outcome Differences
Looking at long-term results, both surgery and non-surgical treatments have their benefits. Surgery can give lasting relief for some, making symptoms less likely to come back. But non-surgical treatments can also lead to long-term improvement, with some people getting rid of their symptoms completely.
Choosing between these options depends on many factors. These include how bad your symptoms are, your overall health, and what you prefer. Talking to healthcare professionals is key to finding the right treatment for you.
Financial Considerations: Cost, Insurance, and Economic Impact
When thinking about herniated disc surgery, knowing the financial side is key. The surgery’s cost can change a lot. This depends on the procedure type, the surgeon’s fees, and where the surgery happens.
Average Costs of Different Surgical Procedures
In the U.S., herniated disc surgery can cost between $15,000 and $30,000 or more. A simple procedure like microdiscectomy might cost between $15,000 and $25,000. But, more complex surgeries like spinal fusion can cost $30,000 to $50,000 or more.
Costs include:
- Surgeon’s fees
- Hospital or surgical facility charges
- Anesthesia fees
- Pre-operative and post-operative care
- Imaging and diagnostic tests
Insurance Coverage for Spine Surgery
Insurance for herniated disc surgery varies by provider and policy. Most plans cover some costs, but how much can vary a lot. It’s important to check your insurance before surgery.
A study found that:
“Most patients with private insurance have coverage for spine surgery, but out-of-pocket costs vary widely.”
Hidden Costs of Recovery and Rehabilitation
There are also hidden costs for recovery and rehab. These include physical therapy, pain meds, and lost income from time off work.
Economic Comparison to Ongoing Conservative Treatment
The initial surgery cost might seem high. But it’s often cheaper than ongoing conservative treatment. Chronic pain management, physical therapy, and doctor visits can add up over time. Surgery might be more cost-effective in the long run.
In conclusion, understanding the financial side of herniated disc surgery is essential. By looking at costs, insurance, and hidden costs and comparing them to ongoing treatment, patients can make better financial decisions.
Special Considerations for Different Patient Populations
Choosing herniated disc surgery is a big decision. It needs to fit the individual, considering their unique needs. Different groups have special needs that affect surgery results and recovery.
Age-Related Factors in Surgical Decision-Making
Age is key in herniated disc surgery. Older patients face more risks due to health issues. Older adults need detailed checks before surgery to understand their health risks. Younger patients might heal faster because of better health.
Comorbidities and Their Impact on Surgical Outcomes
Comorbidities can make herniated disc surgery harder and affect recovery. Conditions like diabetes, heart disease, and obesity raise surgery risks. Managing these conditions before, during, and after surgery is vital for a good outcome.
| Comorbidity | Potential Impact on Surgery | Preoperative Consideration |
| Diabetes | Increased risk of infection | Control blood sugar levels |
| Heart Disease | Higher risk of cardiac complications | Cardiac evaluation |
| Obesity | Increased risk of wound complications | Weight management |
Athletes and Physically Demanding Occupations
Athletes and those with demanding jobs need special care with herniated disc surgery. The goal is to ease pain and help them get back to their activities. Rehabilitation programs that meet their needs are key to a good recovery.
Pregnancy and Herniated Disc Management
Pregnancy makes diagnosing and treating herniated discs harder. Conservative management is often preferred, with surgery for severe cases. The health of both the mother and fetus is the top priority.
Healthcare providers must understand these special considerations to give personalized care. By considering the unique factors of different patient groups, they can improve surgery results and patient happiness.
Long-Term Effects of Herniated Disc Surgery
It’s important to know the long-term effects of herniated disc surgery. Surgery can help a lot with the pain, but it’s key to understand how it might affect your spine and health later on.
Adjacent Segment Disease
One big thing to think about after surgery is adjacent segment disease (ASD). ASD is when the discs next to the one fixed in surgery start to break down. “The risk of developing ASD is a critical factor in the long-term management of patients who have undergone herniated disc surgery.” It’s something that needs watching and might need more treatment later.
Spinal Stability and Biomechanics
Surgery can change how your spine works and how stable it is. “Maintaining spinal stability is key to avoiding long-term problems and making sure the surgery works.” Physical therapy helps a lot in getting your spine strong again after surgery.
Long-term Pain Management Needs
Even with surgery, some people might keep feeling pain. “Finding good ways to manage pain long-term is key to a better life for these patients.” This could mean taking medicine, changing your lifestyle, or trying other treatments.
Impact on Future Spinal Health
The surgery’s effects can also affect your spine’s health over time. “Knowing how surgery might affect your spine’s future health is important for making good choices about surgery.” Things like your age, how you live, and other spine problems can change how well surgery works out.
In short, while herniated disc surgery can help a lot, it’s vital to know the long-term effects. By understanding these, patients can set realistic goals and work towards keeping their spines healthy for the long haul.
Making the Decision: Questions to Ask Your Surgeon
Deciding on herniated disc surgery needs a detailed talk with your surgeon. This talk is key to grasping the surgery, its good points, and possible downsides. Asking the right questions helps patients make choices that fit their health goals and hopes.
Evaluating Surgical Necessity
Patients often wonder if surgery is really needed. They should ask their surgeons about their condition and how it affects their lives. Knowing the diagnosis and why surgery is suggested is very important.
Some questions to ask include:
- What symptoms mean surgery is needed?
- Have all non-surgical treatments been tried?
- How will surgery help more than other treatments?
Understanding Your Specific Procedure
It’s important to know about the recommended surgery. This means understanding the type of surgery, the methods used, and what it involves. Patients should also ask about the surgeon’s experience with the procedure and what results to expect.
Key questions to ask your surgeon include:
- What is the surgery’s name, and how is it done?
- What risks and complications could there be?
- Are there other surgeries that could work, and how do they compare?
Discussing Expected Outcomes
Knowing what to expect from surgery is key to setting realistic hopes. Patients should talk about the surgery’s benefits, like pain relief and better movement, and the recovery time. It’s also important to ask about success chances and long-term effects.
Some questions to consider:
- What improvements can I expect from the surgery?
- How long will I need to recover, and what does it involve?
- Are there any long-term risks or complications?
Second Opinion Considerations
Getting a second opinion is a common step that can offer more insights and reassurance. Patients should not be afraid to see another specialist if they have doubts or concerns about the first advice.
When seeking a second opinion, consider asking:
- Does the second opinion agree with the first on diagnosis and surgery?
- Are there other treatments or surgeries suggested by the second opinion?
- How do the two opinions compare, and what does it mean?
Deciding on herniated disc surgery requires a detailed talk with your surgeon and possibly more opinions. By understanding the surgery’s need, the procedure’s details, and expected results, patients can make a confident choice.
Patient Experiences: Real-World Outcomes and Testimonials
Patients who have had herniated disc surgery share their stories. These stories help others understand what to expect. They can make better choices about their treatment.
Success Stories and Positive Outcomes
Many patients feel much better after surgery.
Challenges and Disappointments
Not everyone has a positive experience. Some face ongoing pain or numbness. It’s important to know that results can vary.
Lessons Learned from Patient Journeys
Testimonials teach us a lot. One key lesson is to have realistic expectations. Being ready for challenges can make recovery better.
Choosing the right surgeon and following care instructions are also important. Sticking to a rehabilitation plan can lead to better results.
What Patients Wish They Had Known Before Surgery
Many patients wish they knew more before surgery. They wish they understood recovery better and the importance of choosing a good surgeon.
Learning from others can help you make better choices. It can guide you through your treatment journey.
Conclusion: Is Herniated Disc Surgery Worth It?
Patients can decide if herniated disc surgery is right for them by looking at the benefits and risks. Surgery can greatly reduce pain and improve quality of life. It also helps restore nerve function.
Choosing surgery depends on understanding your condition and symptoms. You should also know the outcomes of surgery and other treatments. Think about how your condition affects your daily life and the risks.
For those with severe symptoms that haven’t improved with other treatments, surgery might be a good choice. It’s important to talk to a healthcare professional about your situation. They can help decide the best treatment for you.
FAQ
What are the benefits of herniated disc surgery?
Herniated disc surgery can greatly reduce pain and improve your life. It helps alleviate symptoms and can reduce the need for pain medication. It also helps restore your mobility.
Is surgery necessary for a herniated disc?
Not all herniated discs need surgery. Many can be treated with physical therapy, medication, and lifestyle changes. But if these treatments don’t work, or if symptoms are severe, surgery might be needed.
What are the risks and complications associated with herniated disc surgery?
Herniated disc surgery comes with risks like infection, bleeding, and nerve damage. It’s important to understand these risks before deciding on surgery.
How long does it take to recover from herniated disc surgery?
Recovery times vary based on the surgery type and individual factors. Most people can get back to normal in a few weeks to months. Physical therapy is key to a good recovery.
What is the success rate of herniated disc surgery?
Success rates vary by surgery type and patient. Some procedures have a 70% to 90% success rate. But individual results can differ.
How does surgery compare to non-surgical treatment for herniated discs?
Surgery can offer quick pain relief and better function. But it comes with risks. Non-surgical treatments are often tried first. If they fail, surgery might be considered.
What are the financial considerations for herniated disc surgery?
Surgery costs vary by procedure, location, and insurance. It’s important to consider not just the surgery cost but also recovery and rehabilitation expenses.
Are there special considerations for different patient populations undergoing herniated disc surgery?
Yes, different groups like older adults and athletes have unique needs. Age, health, and specific needs should be considered when deciding on surgery.
What are the long-term effects of herniated disc surgery?
Surgery can lead to long-term issues like changes in spinal stability. It’s important to understand these effects to make informed decisions.
What questions should I ask my surgeon before undergoing herniated disc surgery?
Ask your surgeon about the need for surgery, the procedure, expected results, risks, and recovery. Getting a second opinion is also a good idea.
References
- Atlas, S. J., & Deyo, R. A. (2001). Evaluating and managing acute low back pain in the primary care setting. JAMA, 288(21), 2766–2774. National Library of Medicine. https://pubmed.ncbi.nlm.nih.gov/11735705/