Last Updated on October 21, 2025 by mcelik
Graft versus host disease (GVHD) of the lungs is a serious issue after an allogeneic hematopoietic stem cell transplant. If you’re feeling short of breath or coughing after such a procedure, it’s understandable to be worried.
At Liv Hospital, we have a team with international expertise in managing GVHD lung complications. We focus on you, ensuring you get the support and guidance you need during treatment.
Pulmonary GVHD affects nearly 9% of transplant patients. This makes it a big concern for those going through this procedure. We’ll cover the essential facts about GVHD lungs, including symptoms, diagnosis, and treatment. Our goal is to give you the information and support you need.
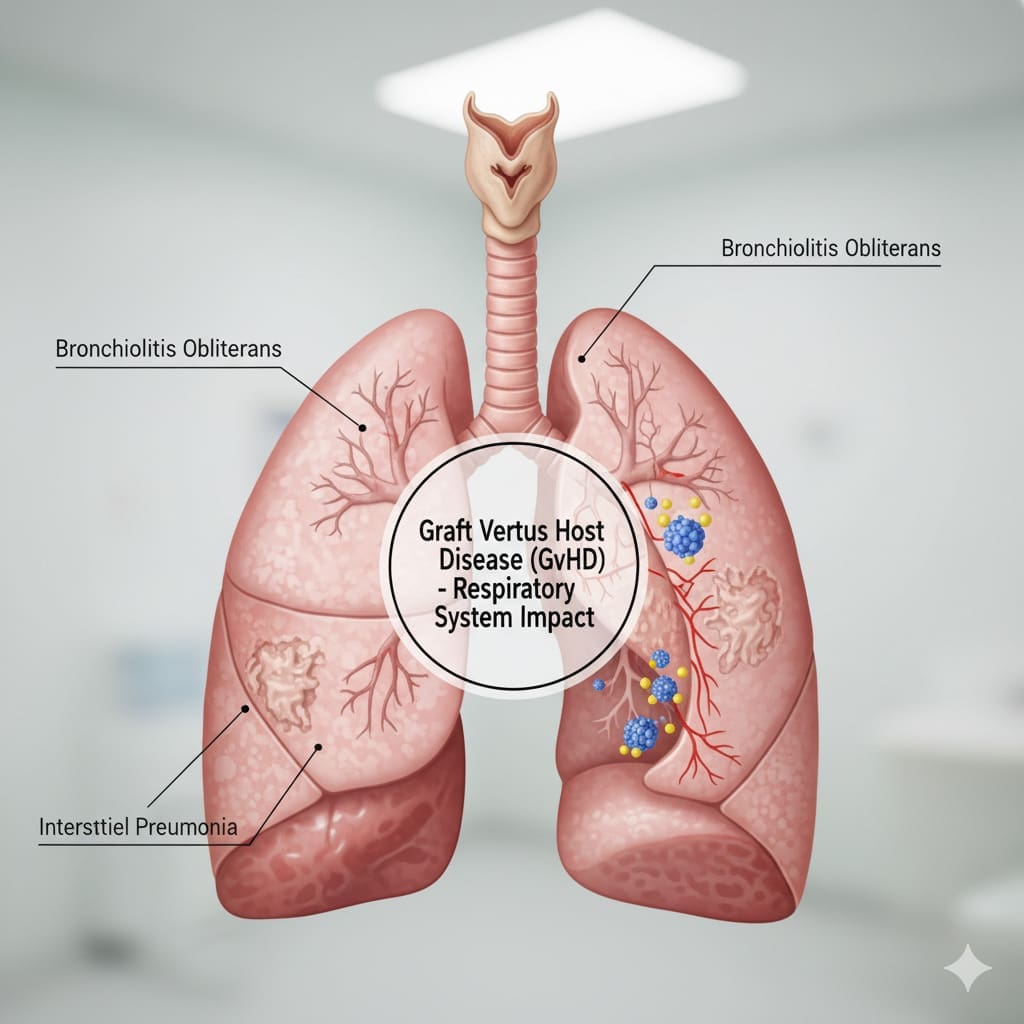
Graft Versus Host Disease (GVHD) happens when a donor’s immune cells see the recipient’s body as foreign. This can cause serious problems, like GVHD lung disease in the lungs.
GVHD starts when the donor’s immune cells attack the recipient’s body. This can harm organs like the lungs. Symptoms include coughing and feeling short of breath. For more info, check out our resource page on Graft Versus Host.
GVHD develops when donor immune cells and recipient tissues interact. The key factors contributing to GVHD are:
Knowing these factors helps find patients at risk of GVHD. It also helps take steps to prevent it.
The lungs are very sensitive to GVHD. It often shows up as bronchiolitis obliterans syndrome (BOS). BOS causes inflammation and scarring in small airways, leading to symptoms like:
Spotting GVHD lung disease early is hard because its symptoms are not clear. That’s why regular lung function tests, like FEV1, are important to check how well the lungs are working.
It’s key to understand how common GVHD lungs are and who might get them. GVHD of the lungs is a serious issue that can happen after a certain type of transplant. We’ll look at how often it occurs and why it’s important to spot those at risk early.
About 9% of transplant patients get GVHD lungs. Research shows GVHD can affect many parts of the body, including the lungs. This number shows we need to watch for GVHD lungs closely to help patients do better.
Finding out who’s most likely to get GVHD lungs is a big deal. Things like the transplant type, how well the donor and recipient match, and the patient’s health can play a part. Knowing these factors helps doctors come up with plans to lower the risk of GVHD lungs and make transplants more successful.
GVHD lungs can really hurt a transplant patient’s quality of life. So, it’s important to find a balance between preventing GVHD and the risks of treatments that stop it.
It’s important to spot the early signs of pulmonary GVHD to act quickly. Symptoms like cough and shortness of breath can signal GVHD lung disease.
The first signs of GVHD lungs can be tricky to spot. They might include:
These signs can look like other lung problems. So, doctors need to be extra careful with transplant patients.
Even though they’re important, GVHD lung symptoms are often missed. This is because of:
| Factor | Description |
|---|---|
| Non-specific presentation | The symptoms can be similar to those of other respiratory conditions, making diagnosis challenging. |
| Lack of awareness | Patients and healthcare providers may not be fully aware of the risks and symptoms of GVHD lungs. |
| Variability in symptom severity | The severity of symptoms can vary widely among patients, making it difficult to diagnose based on symptoms alone. |
Knowing these reasons helps us improve early detection and treatment. By understanding these symptoms and challenges, doctors can better manage GVHD lungs.
In GVHD lungs, the FEV1 marker is key for checking lung function and predicting results. FEV1, or Forced Expiratory Volume in one second, is a vital test. It shows how much air you can breathe out in one second, helping to see how bad lung damage is.
Lung function tests, like FEV1, are very important for diagnosing and treating GVHD patients’ breathing problems. FEV1 is very important because it shows how blocked the airways are. By watching FEV1 changes, doctors can see how lung disease is getting worse or better and if treatments are working.
A drop in FEV1 is a big warning sign of lung function getting worse. Studies have found that a ≥10% decline in FEV1 after a transplant means a higher risk of death and less chance of getting better. This number is a warning to doctors to change treatment plans and try harder to stop things from getting worse.
Knowing about FEV1 changes helps doctors make treatment plans that fit each patient’s needs. This can lead to better care and health for GVHD lungs. By watching FEV1 closely and acting on big changes, we can help patients breathe better and live healthier lives.
Diagnosing GVHD lungs is a big challenge after a transplant. The symptoms can be hard to spot because they are not specific. This makes it tough to tell if it’s GVHD or something else.
To figure out GVHD lungs, doctors use a few methods. Pulmonary function testing (PFT) is a key first step. It shows how well the lungs are working and if there are any problems.
For GVHD lungs, PFTs check things like Forced Expiratory Volume in 1 second (FEV1) and Forced Vital Capacity (FVC). These tests help see how bad the lung damage is and if it’s getting worse.
| PFT Parameter | Description | Significance in GVHD Lungs |
|---|---|---|
| FEV1 | Volume exhaled in the first second | A decline indicates obstructive lung disease |
| FVC | Total volume exhaled | Reductions suggest restrictive lung disease |
| FEV1/FVC Ratio | Ratio of FEV1 to FVC | A low ratio indicates airway obstruction |
If PFTs don’t give clear answers, doctors might use lung biopsy. This involves looking at lung tissue for GVHD signs like lymphocytic infiltration and fibrosis.
Handling GVHD in the lungs needs a detailed plan. This includes using medicines to suppress the immune system and special treatments for the lungs. Using advanced tests is key to making the right treatment choices and helping patients get better.
It’s important to know the difference between acute and chronic GVHD lungs. Graft-versus-host disease (GVHD) can affect the lungs in two ways. Each type has its own signs and treatment needs.
Acute GVHD happens early, usually within 100 days after a transplant. It shows up quickly with symptoms like trouble breathing and coughing. Chronic GVHD, on the other hand, starts later and its symptoms come on slowly.
Knowing when GVHD starts is key to treating it right. Acute GVHD might need quick action with medicines. Chronic GVHD needs a careful plan to manage symptoms and avoid lung damage.
Chronic GVHD of the lungs often leads to bronchiolitis obliterans syndrome (BOS). BOS causes inflammation and scarring in the airways. It’s a serious problem because it can lead to permanent lung damage.
BOS is a big deal in chronic GVHD lungs. Doctors diagnose it by looking at symptoms, lung function tests, and scans. Finding BOS means the lung GVHD is severe and might not get better.
The table below shows the main differences between acute and chronic GVHD lungs. It covers when they happen, how they start, and what they look like.
| Characteristics | Acute GVHD Lungs | Chronic GVHD Lungs |
|---|---|---|
| Timeframe | Within 100 days post-transplant | Beyond 100 days post-transplant |
| Presentation | Sudden onset of respiratory symptoms | Insidious onset of symptoms |
| Characteristic Features | Diffuse alveolar damage | Bronchiolitis obliterans syndrome (BOS) |
It’s vital for doctors to understand these differences. Patients need to know about their condition and how to manage it.
Treating GVHD in the lungs needs a two-part plan. This plan includes both general treatments and specific lung-focused treatments. The goal is to calm down the immune system and protect the lungs from more damage.
Systemic treatments are key in fighting GVHD in the lungs. These treatments include:
Targeted lung treatments are also vital in managing GVHD in the lungs. These treatments include:
By using both systemic treatments and lung-focused treatments, we can manage GVHD in the lungs well. It’s important to keep an eye on how the patient is doing. We need to adjust the treatment plan as needed for the best results.
When first treatments fail, patients with GVHD lungs need new, aggressive treatments. Advanced therapies offer hope for managing GVHD lungs better. They aim to improve patient outcomes and quality of life.
For those not helped by initial treatments, second-line options are key. Infliximab, a monoclonal antibody, targets immune pathways in GVHD. It has shown to reduce inflammation and improve lung function in some patients.
Other second-line treatments include:
| Treatment | Mechanism | Potential Benefits |
|---|---|---|
| Infliximab | Monoclonal antibody against TNF-alpha | Reduces inflammation, improves lung function |
| ECP | Modifies immune cells outside the body | Modulates immune response, potentially reducing GVHD severity |
| Rituximab | Targets B cells | Decreases immune system’s attack on lung tissues |
Researchers are also exploring new therapies for GVHD lungs. These include:
These new approaches could greatly help patients with GVHD lungs, including those needing lung transplant due to GVHD. Ongoing research and trials are vital to check their safety and effectiveness.
As research advances, we might see better ways to manage GVHD lungs, including chronic lung GVHD. This could greatly improve the lives of those affected.
For those with severe GVHD lungs, lung transplantation might be a lifesaver. This complex surgery is for those with lung damage that can’t be fixed by other means.
Deciding on lung transplantation is complex. It depends on the patient’s health, lung damage, and chances of success. Key indicators for transplant consideration include:
We look at these factors to see if a patient is a good candidate for lung transplantation.
Results after lung transplantation for GVHD lungs vary. They depend on the patient’s health before the transplant, any other health issues, and the treatment plan after. Studies have shown that survival rates are getting better thanks to new transplant methods and care.
We keep a close eye on how patients do after the transplant. We look at survival rates, how well they’re doing, and managing any problems. Our data show that, in some cases, lung transplantation can greatly improve survival and quality of life for those with severe GVHD lungs.
GVHD lungs bring many challenges that need a complete management plan. This plan includes medical treatment, lifestyle changes, and support care. It’s key to manage GVHD in the lungs to better patient outcomes.
Pulmonary rehab is vital for GVHD lung patients. It helps manage symptoms and boosts lung function. These programs mix exercise, education, and behavior changes.
By joining pulmonary rehab, patients see better exercise tolerance and less breathlessness.
Stopping infections is key in managing GVHD lung symptoms. Patients with GVHD lungs are at high risk of infections. We suggest vaccinations, antimicrobial prophylaxis, and avoiding pathogens.
These steps help lower the risk of pulmonary complications in GVHD.
Quality of life matters a lot for GVHD lung patients. The physical and emotional hurdles of GVHD can affect daily life. We focus on symptom management, psychological support, and lifestyle changes.
This approach aims to boost overall well-being.
In summary, managing GVHD lungs needs a detailed plan. It should include pulmonary rehab, infection prevention, and quality of life focus. This way, we can improve patient outcomes and enhance their life quality.
As we learn more about GVHD lungs, it’s clear we need more research. This is key to better diagnose and treat graft versus host disease lungs. Pulmonary issues in GVHD are a big problem for transplant patients.
New tools like systems biology and artificial intelligence will help us understand GVHD lungs better. These technologies could lead to better ways to manage GVHD. They promise to help patients by spotting problems early and tailoring treatments.
We expect future studies to improve how we diagnose and treat GVHD in the lungs. By exploring new areas in GVHD research, we aim to lessen the impact of GVHD on lungs. This will help improve the lives of those affected by GVHD.
GVHD of the lungs, or pulmonary GVHD, is a serious issue after a stem cell transplant. It happens when the donor’s immune cells see the recipient’s body as foreign. This leads to an immune attack on the lung tissues.
Symptoms of GVHD lungs include coughing, shortness of breath, and wheezing. These signs are often not noticed until the disease is advanced.
GVHD lungs affect nearly 9% of transplant patients. It’s a big concern for those undergoing this procedure.
A drop in FEV1 shows lung function decline. A ≥10% drop after transplant raises mortality risk and reduces recovery chances.
Diagnosing GVHD lungs involves lung function tests and advanced techniques like lung biopsy. Symptoms are often non-specific.
Chronic GVHD, like bronchiolitis obliterans syndrome, has a poor prognosis. It affects lung function more than acute GVHD. It has different presentation and timeframe.
First-line treatments for pulmonary GVHD include immunosuppressive drugs like corticosteroids and calcineurin inhibitors. Targeted pulmonary interventions are also used.
For refractory GVHD lungs, second-line treatments like infliximab are used. Experimental approaches are also explored for those not responding to first-line treatments.
Lung transplantation is considered for severe, irreversible lung damage from GVHD. It involves careful evaluation of indications and post-transplant outcomes.
Patients with GVHD lungs can manage their condition through pulmonary rehabilitation, infection prevention, and quality of life considerations. These help improve symptoms and prevent complications.
Managing chronic lung GVHD requires a multi-faceted approach. This includes immunosuppressive therapies and targeted pulmonary interventions to slow disease progression and improve quality of life.
Lung function tests, like FEV1, help diagnose GVHD lungs by assessing lung function. They detect abnormalities, enabling early intervention and management.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!