Last Updated on November 4, 2025 by mcelik

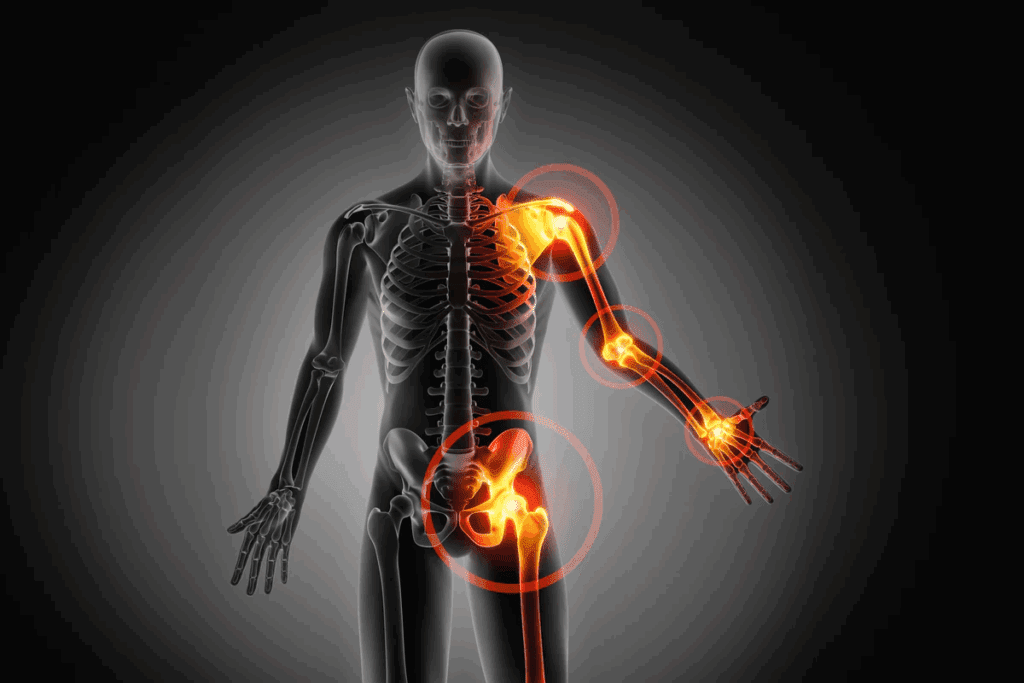
Did you know over 10 million Americans have osteoporosis? This condition weakens bones, making them more likely to break. Finding the right way to manage it is very important.Find the best thing to take if you have osteoporosis and explore the most effective treatment for osteoporosis.
Managing osteoporosis well means making lifestyle changes and using medical treatments. It’s key to understand the condition and its effects on bones to choose the best treatment.
Osteoporosis means “porous bones.” It makes bones weak and more likely to break. This happens when the body doesn’t make enough new bone or when too much old bone is lost.
Osteoporosis weakens bones, making them more likely to break. Normal bone is constantly being remodeled through a process involving the breakdown and formation of bone tissue. In osteoporosis, this balance is disrupted, with more bone being broken down than formed. The condition often progresses without symptoms until a fracture occurs, highlighting the importance of preventive measures and early diagnosis.
Bone loss in osteoporosis can be caused by hormonal changes, nutritional deficiencies, and lifestyle factors. Hormonal changes, such as those experienced during menopause, can accelerate bone loss due to decreased estrogen levels. Also, not enough calcium and vitamin D is bad for bones. Lifestyle factors, like not moving enough, smoking, and drinking too much alcohol, also raise the risk of osteoporosis.
Some groups are more likely to get osteoporosis. These include older adults, postmenopausal women, people with a family history of osteoporosis, and those with certain medical conditions or taking specific medications. Risk assessment helps figure out who might get osteoporosis and break bones. Key risk factors include:
Osteoporosis diagnosis focuses on bone density and health. Accurate diagnosis is key for the right treatment.
Bone Mineral Density (BMD) testing is vital for diagnosing osteoporosis. It checks the minerals in bones, showing strength and fracture risk. Dual-Energy X-ray Absorptiometry (DXA) is the main BMD test.
The test results are shown as T-scores. These scores compare your bone density to a healthy young adult of the same sex. A T-score of -2.5 or lower means you have osteoporosis. Scores between -1 and -2.5 suggest osteopenia, a condition before osteoporosis.
BMD testing is the top choice for osteoporosis diagnosis. But, other tools offer extra info. These include:
These tools, along with medical history and physical exams, help doctors assess osteoporosis risk. They guide treatment choices.
The main goal of treating osteoporosis is to stop fractures. This keeps bones strong and improves overall health. Treatment plans include many steps to reduce fracture risk and boost bone health and life quality.
Stopping fractures is key in treating osteoporosis. This is done through lifestyle changes, better nutrition, and medicines. By lowering fracture risk, people with osteoporosis can live better and stay independent.
Keeping or growing bone density is another big goal. This is done with exercises, enough calcium and vitamin D, and certain medicines. Regular checks and treatment plan changes are vital to reach this goal.
Osteoporosis can make life hard, causing pain and limiting movement. Treatments aim to ease pain and boost how well you can move. This includes physical therapy, pain meds, and other support.
| Treatment Goals | Strategies | Benefits |
| Preventing Fractures | Lifestyle changes, nutritional supplements, medications | Reduced fracture risk, improved quality of life |
| Maintaining/Improving Bone Density | Exercise, calcium/Vitamin D intake, bone-enhancing medications | Enhanced bone health, reduced risk of osteoporosis progression |
| Reducing Pain/Enhancing Quality of Life | Physical therapy, pain management, supportive measures | Alleviated pain, improved mobility and functional capacity |
Bisphosphonates are often the first choice for treating osteoporosis. They help increase bone density. This makes them effective in lowering the risk of fractures in people with osteoporosis.

Bisphosphonates stop bone resorption by osteoclasts. This leads to more bone mass and less fracture risk. They keep bones strong by reducing bone loss.
There are several oral bisphosphonates like alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva). These are taken weekly or monthly. They are good at preventing vertebral and non-vertebral fractures.
Zoledronic acid (Reclast) is for those who can’t take oral bisphosphonates. It’s an intravenous infusion given once a year. It significantly lowers fracture risk in postmenopausal women with osteoporosis.
Bisphosphonates are effective in lowering fracture risk and are usually well-tolerated. But, they can have side effects and long-term use needs careful thought. Despite this, they are key in treating osteoporosis because they strengthen bones and prevent fractures.
SERMs are used in osteoporosis treatment. They mimic estrogen’s good effects on bones without its risks. These medications work on estrogen receptors and help keep or boost bone density.
Raloxifene, known as Evista, helps prevent vertebral fractures in postmenopausal women with osteoporosis. It binds to estrogen receptors, mimicking estrogen’s positive effects on bones. This helps keep bones healthy and lowers the chance of vertebral fractures.
Choosing raloxifene depends on the patient’s risk for osteoporosis and fractures. It’s best for postmenopausal women at high risk of vertebral fractures but low risk of other fractures. But, the benefits must be balanced against the risks, like a higher chance of blood clots.
| Characteristics | Raloxifene (Evista) |
| Mechanism of Action | Acts on estrogen receptors to maintain bone density |
| Primary Benefit | Reduces risk of vertebral fractures |
| Ideal Candidates | Postmenopausal women at high risk of vertebral fractures |
Anabolic agents are a new hope for those with osteoporosis. They help build new bone. This is different from treatments that just stop bone loss.
Teriparatide, or Forteo, and abaloparatide, or Tymlos, are two promising treatments. They are given by injection. They work like parathyroid hormone to grow new bone. Key benefits include:
Teriparatide is used for up to 2 years. Abaloparatide is used for up to 18 months. Both help lower fracture risk in postmenopausal women with osteoporosis.
Romosozumab, or Evenity, is a new agent with a unique action. It builds bone and stops bone loss. Clinical trials have shown:
Romosozumab is given monthly for 12 months. Its unique action and effectiveness make it a key option for those at high fracture risk.
Denosumab, known as Prolia, is a big step forward in treating osteoporosis. It’s a monoclonal antibody that targets RANKL. This protein is key in breaking down bone.
Denosumab doesn’t work like bisphosphonates. Instead, it targets RANKL to stop bone breakdown. This targeted approach leads to less bone loss.
Denosumab’s unique mechanism makes it a good choice for those who can’t take bisphosphonates.
Denosumab is given as a subcutaneous injection every six months. It’s easy for patients to take. Studies show it boosts bone density and lowers fracture risk.
But, it’s important to watch out for side effects like hypocalcemia and dermatological reactions. Patients on denosumab need to be checked for these issues.
Denosumab is a great option for osteoporosis treatment. It offers a targeted and effective way to reduce fracture risk.
Hormone replacement therapy (HRT) is a common treatment for osteoporosis, mainly in postmenopausal women. It involves giving the body hormones it no longer makes after menopause, mainly estrogen.
HRT helps keep or boost bone density in postmenopausal women. This reduces the chance of fractures linked to osteoporosis.
Estrogen therapy, a type of HRT, is good for bones. It offers several benefits:
HRT has its benefits for bones, but it also comes with risks. These include a higher chance of breast cancer, blood clots, and stroke. So, it’s important to think carefully before starting HRT.
The pros and cons of HRT depend on several things. These include the patient’s health history, age, and the type of therapy. Talking to a healthcare provider is key to decide if HRT is right for you.
Osteoporosis medications can have side effects, from mild to severe. It’s important for patients and doctors to know about these issues. This way, they can manage them well.
Oral bisphosphonates, a common type of osteoporosis medication, can cause stomach problems. These include esophagitis, gastritis, and dyspepsia. To lessen these risks, patients should take the medicine with a full glass of water. They should also stay upright for at least 30 minutes after.
Osteonecrosis of the jaw (ONJ) is a rare but serious issue linked to some osteoporosis drugs, like bisphosphonates and denosumab. ONJ causes jawbone tissue death, leading to pain, swelling, and exposed bone. To prevent it, keep good oral hygiene, avoid major dental work, and tell your dentist about your medication.
| Risk Factors for ONJ | Preventive Measures |
| Use of bisphosphonates or denosumab | Good oral hygiene practices |
| Invasive dental procedures | Avoiding invasive dental work |
| Poor oral health | Regular dental check-ups |
Atypical femur fractures (AFFs) are rare but serious problems linked to long-term bisphosphonate use. AFFs are fractures in the thigh bone with little or no trauma. Other rare issues include atrial fibrillation and severe muscle pain. Patients on long-term medication should be closely watched for these risks.
Knowing the side effects and complications of osteoporosis medications helps patients and doctors. They can then work together to reduce risks and get the most from treatment.
Making lifestyle changes is key to managing osteoporosis and keeping bones strong. By adding natural methods to your daily routine, you can greatly boost your bone health.
Eating a balanced diet is essential for bone health. Calcium and Vitamin D are critical because they help build bone density. Vitamin K aids in bone mineralization, and Magnesium helps the body absorb calcium.
Focus on foods high in these nutrients. Dairy products are full of calcium, and fatty fish are a vitamin D powerhouse. Spinach and kale are great for magnesium and vitamin K.
| Nutrient | Food Sources | Benefits |
| Calcium | Dairy products, leafy greens, fortified foods | Builds and maintains bone density |
| Vitamin D | Fatty fish, fortified dairy products, sunlight exposure | Enhances calcium absorption |
| Vitamin K | Leafy greens, fermented foods | Supports bone mineralization |
| Magnesium | Nuts, seeds, whole grains, leafy greens | Aids in calcium absorption and bone health |
Exercise is vital for bone health. Weight-bearing and resistance exercises are best for strengthening bones. Activities like walking, running, and weightlifting help bones grow and get denser.
A study in the Journal of Bone and Mineral Research showed that resistance training boosts bone density in older adults.
“Resistance exercise is a potent stimulus for bone growth and can be an effective adjunct to traditional treatments for osteoporosis.”
Here are some effective exercises:
Along with diet and exercise, some alternative therapies and supplements can help bone health. Acupuncture and yoga can improve balance and lower fall risks. Supplements like calcium and vitamin D are good for those who can’t get enough from food.
Always talk to a healthcare provider before trying new supplements or therapies. This ensures they’re safe and right for you.
Osteoporosis treatment options vary, and understanding the differences is key to making an informed decision. Several medications and lifestyle changes are available. Comparing their effectiveness, convenience, and cost helps individuals and healthcare providers create a personalized plan.
Several factors influence the choice of osteoporosis treatment. These include the severity of the condition, patient health, and personal preferences. For instance, patients with severe osteoporosis may need more aggressive treatment, like bisphosphonates or anabolic agents.
Those with mild osteoporosis might manage it through lifestyle changes and supplements. Other factors include the presence of other health conditions and patient preferences. For example, avoiding certain medications or minimizing injections can influence treatment choices.
When comparing osteoporosis treatments, effectiveness, convenience, and cost are key. For example, bisphosphonates are a common first-line treatment. They can be taken orally or intravenously and are effective in reducing fracture risk. Yet, they can cause gastrointestinal side effects and may need frequent dosing.
Denosumab is a targeted therapy given via injection every six months. It may be more convenient but is more expensive than bisphosphonates.
Creating a personalized treatment plan for osteoporosis requires teamwork between the patient and healthcare provider. Specialists, like rheumatologists or endocrinologists, offer valuable insights. They help patients navigate the complex world of treatment options.
Together, patients and healthcare providers can craft a plan that meets their unique needs and goals. This might include a mix of medications, lifestyle changes, and regular monitoring. This ensures the treatment is effective and safe.
New research is changing how we treat osteoporosis. We’re learning more about bones and how to help them. This leads to new ways to help patients with osteoporosis.
New medicines are being tested to help with osteoporosis. These medicines aim to make bones stronger and lower the chance of breaks. Trials are checking if these treatments are safe and work well.
New ways to monitor and treat osteoporosis are also being developed. Better tools help doctors understand bone health better. This means treatments can be more tailored to each patient.
As research keeps moving forward, the future for osteoporosis treatment looks bright. New discoveries could greatly improve how we care for patients with this condition.
Managing osteoporosis well means making smart choices about treatment and lifestyle. Knowing about different treatments like bisphosphonates and SERMs helps. This way, you can work with your doctor to create a plan that’s just right for you.
It’s important to keep up with new research and guidelines for osteoporosis. New medicines and better ways to monitor and treat the condition are always coming. This means more options for people with osteoporosis.
When choosing a treatment, think about how well it works, how easy it is to use, and the cost. Talking to specialists and staying current with osteoporosis news helps keep your bones strong. It also lowers the chance of breaking a bone.
Osteoporosis makes bones weak, leading to more fractures. It lowers bone density and quality. This increases the risk of breaking bones.
Hormonal changes, age, and lifestyle factors cause bone loss in osteoporosis. An imbalance between bone resorption and formation leads to bone tissue loss.
Postmenopausal women, older adults, and those with a family history are at high risk. Low body weight, smoking, and too much alcohol also increase risk.
Doctors use bone mineral density (BMD) tests, like DXA scans, to diagnose osteoporosis. T-scores help interpret results, with scores below -2.5 indicating osteoporosis.
Treatment aims to prevent fractures, improve bone density, and reduce pain. It aims to enhance quality of life.
Bisphosphonates, like alendronate (Fosamax) and zoledronic acid (Reclast), stop bone resorption. This reduces bone loss and increases density.
SERMs, such as raloxifene, help keep bone density and reduce vertebral fractures. But they may raise blood clot and hot flash risks.
Anabolic agents, like teriparatide (Forteo) and romosozumab (Evenity), boost bone formation. They increase density and lower fracture risk.
Denosumab (Prolia) targets and stops osteoclasts, cells that break down bone. It’s given every six months to treat osteoporosis in those at high fracture risk.
HRT can keep bone density and reduce fractures in postmenopausal women. But it may raise breast cancer and heart disease risks.
Managing side effects involves close monitoring and adjusting treatment as needed. This includes handling stomach issues, jaw problems, and femur fracture risks.
Eating right, with calcium, vitamin D, and magnesium, and exercising regularly are key. Supplements and alternative therapies can also help, but under a doctor’s guidance.
Options can be compared by effectiveness, ease, and cost. A healthcare team can create a plan tailored to your needs and risks.
New meds and trials are emerging. Better diagnostic tools and targeted treatments are also being developed.
PEMF therapy may improve bone density and fracture risk. But more research is needed to confirm its effectiveness.
While there’s no cure, natural methods like diet, exercise, and lifestyle changes can help manage osteoporosis. They can reduce fracture risk.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!