When a blood clot Does Blood Work Show Cancer?forms in a vein or artery, it can cause serious problems. At Liv Hospital, we know how important quick treatment is to get blood flow back to normal. We use medications that dissolve clots fast, called thrombolytics or fibrinolytics. These are given quickly in emergencies.

We use the drug that dissolves blood clots called thrombolytics to quickly restore blood flow. In this article, we’ll cover the top 7 clot-dissolving medications and their emergency use. Thrombolytics like tissue plasminogen activator (tPA), tenecteplase, and reteplase are common. They’re used in emergencies such as heart attacks, strokes, and pulmonary embolisms. These drugs break down clots by activating the body’s natural fibrinolytic system, helping to prevent organ damage and improve survival. Administration is typically via IV or catheter directly to the clot site for rapid effect.
Key Takeaways
- Thrombolytic medications are used to dissolve clots and restore blood flow.
- Timely treatment is key in emergencies.
- Liv Hospital offers patient-focused care for blood clot issues.
- The top 7 medications will be discussed, along with their mechanisms and uses.
- Knowing about these treatments helps people make better choices.
Understanding Blood Clots and Their Treatment
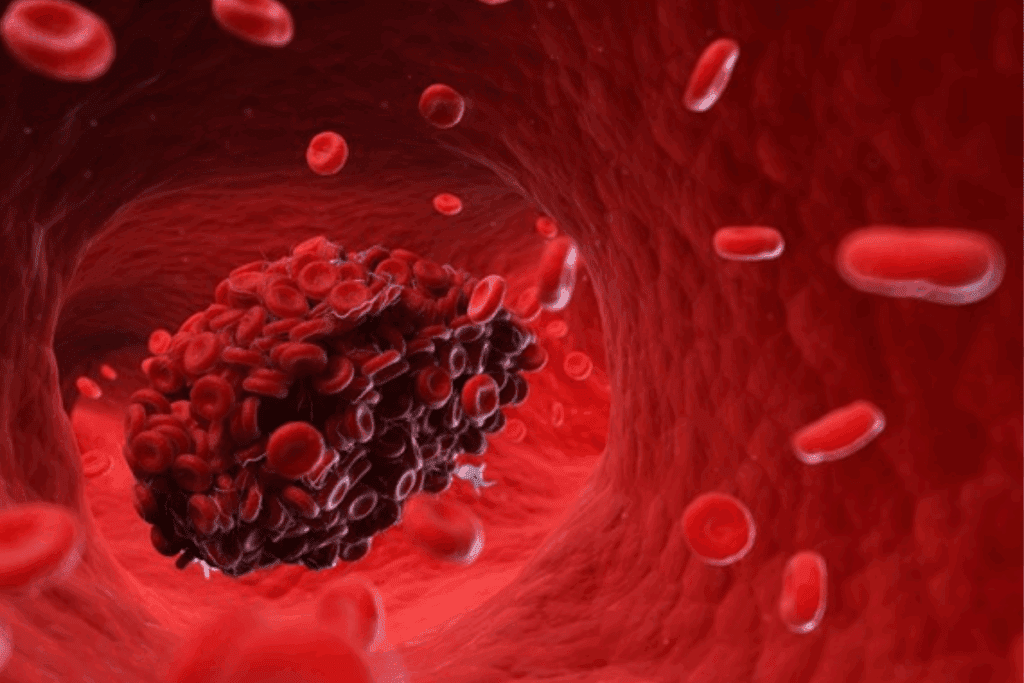
It’s important for both patients and doctors to know about blood clots and how to treat them. Blood clots can happen in different parts of the body. This includes the legs, lungs, and brain. They can cause serious problems like deep vein thrombosis (DVT), pulmonary embolism (PE), and ischemic stroke.
How Dangerous Blood Clots Form
Blood clots become dangerous when the body’s clotting system gets out of balance. This can happen for many reasons. These include staying in one place for too long, having a family history of clotting, or having certain health conditions. When a clot forms, it can block blood flow. This can damage tissues or even cause organ failure if not treated right away.
Studies show that acting fast when blood clots happen is key. Doctors use tools like ultrasound, venography, MRI, or CT scans to find and treat clots accurately.

The Critical Difference Between Clot Dissolvers and Blood Thinners
It’s important to know the difference between clot dissolvers and blood thinners. Blood thinners stop new clots from forming and keep existing ones from growing. Clot dissolvers, on the other hand, break down clots that have already formed. This is very important in emergencies where quick action is needed.
| Treatment Type | Function | Examples |
| Clot Dissolvers (Thrombolytics) | Break down existing clots | tPA, Alteplase, Tenecteplase |
| Blood Thinners (Anticoagulants) | Prevent new clots and stop existing clots from growing | Heparin, Warfarin, Rivaroxaban |
Emergency Treatment Timeline for Best Outcomes
How quickly treatment starts is very important for patients with blood clots. Studies show that using clot dissolvers works best if started within two hours of the clot forming. Quick treatment not only saves lives but also lowers the chance of lasting damage.
Knowing the emergency treatment timeline helps doctors make fast, informed decisions. The goal is always to get blood flowing again as quickly as possible to reduce harm.
Tissue Plasminogen Activator (tPA): The Gold Standard Drug That Dissolves Blood Clots
tPA is the top choice for treating blood clots in patients with ischemic stroke and pulmonary embolism. It quickly opens up blocked blood vessels. This helps restore blood flow to areas that need it most.
Activating Plasminogen to Break Down Clots
tPA turns plasminogen into plasmin, an enzyme that breaks down fibrin in blood clots. This is key to dissolving clots and keeping blood vessels open. It’s a lifesaver in emergencies.
tPA is very precise in its action. It targets fibrin in clots without causing widespread bleeding. This makes tPA a top choice for treating blood clots.
Administration Methods and Timing Requirements
tPA is given through an IV. How quickly it’s given is very important. For stroke, it works best within 4.5 hours of symptoms starting. The exact dose and how it’s given can change based on the condition.
Quick action with tPA is key to good results. Doctors must act fast to give tPA. They check each patient to see if tPA is right for them.
Effectiveness for Stroke, Pulmonary Embolism, and DVT
tPA is very good at treating different blood clot problems. It quickly breaks down clots in the brain, lungs, and veins. This has greatly improved patient outcomes in these serious conditions.
- In ischemic stroke, tPA helps restore blood flow to the brain, reducing the risk of long-term disability.
- For pulmonary embolism, tPA can dissolve clots that obstruct blood flow to the lungs, improving hemodynamics and reducing mortality.
- In deep vein thrombosis, tPA can be used to dissolve clots in the deep veins, reducing the risk of post-thrombotic syndrome.
tPA’s ability to dissolve blood clots makes it a key treatment for many conditions. It’s a vital drug for treating blood clots.
Alteplase: Versatile First-Line Treatment for Multiple Clot Types
Alteplase is a key medication for dissolving blood clots in serious cases. It works by starting the body’s natural clot-breaking process. This makes it a top choice for medication to dissolve blood clots in emergencies.
Alteplase is known for its wide use in treating blood clot-related issues. It’s effective in treating strokes, pulmonary embolism, and deep vein thrombosis. This makes it a vital medication that dissolves blood clots well.
Applications in Ischemic Stroke Treatment
In treating ischemic stroke, Alteplase is given through an IV to quickly get blood flowing to the brain. Given quickly, usually within hours of a stroke, it greatly improves patient outcomes. As a medication to dissolve blood clots, it helps reduce brain damage.
Protocol for Pulmonary Embolism Management
For pulmonary embolism, Alteplase breaks up the clot blocking the blood flow. The treatment is carefully chosen and monitored due to its risks. Alteplase is a key medication to dissolve blood clots in the lungs, improving blood flow.
Treatment Approach for Deep Vein Thrombosis
In deep vein thrombosis, Alteplase is used when there’s a high risk of clot growth or limb ischemia. The choice to use Alteplase weighs the benefits against risks like bleeding. As a medication that dissolves blood clots, it’s a good option for DVT.
Alteplase is a versatile and effective clot-busting agent used in many serious cases. Its use in treating strokes, pulmonary embolism, and deep vein thrombosis highlights its role as a medication to dissolve blood clots quickly and effectively.
Tenecteplase (TNK-tPA): Advanced Single-Dose Thrombolytic
Tenecteplase is a big step forward in treating blood clots. It’s a single-dose treatment. This makes it a next-generation thrombolytic agent, designed to overcome earlier drug limitations.
Enhanced Fibrin Specificity and Longer Half-Life
Tenecteplase targets blood clots better because of its enhanced fibrin specificity. This reduces the risk of bleeding. It also has a longer half-life than traditional tPA, making dosing easier.
Studies show tenecteplase is effective for the treatment of blood clots in the leg and other conditions. It’s noted for better efficacy and fewer side effects.
Single-Bolus Administration Advantage in Emergency Settings
Its single-bolus administration is a big plus in emergencies. It’s quick and easy, allowing doctors to focus on other care needs.
In emergencies, tenecteplase’s single-dose advantage can greatly improve patient results. It’s said to be a major improvement in treating acute ischemic stroke.
Comparative Effectiveness Against Traditional tPA
Studies show tenecteplase works as well as, or better than, traditional tPA. Its ability to target clots and longer action time make it more effective.
Tenecteplase is a leading choice for treating blood clots. Its innovative features make it a valuable tool for doctors treating thrombotic events.
Reteplase: Dual-Bolus Thrombolytic for Rapid Intervention
Reteplase is a key drug in treating blood clots. It works fast and effectively for heart attacks and other clot-related issues.
Unique Structural Properties and Mechanism
Reteplase is a special kind of clot-dissolving medicine. It lasts longer in the body than others, making it easier to use in emergencies. A study on PubMed Central shows it’s good at breaking down clots.
“Reteplase has made treating clots simpler,” say recent guidelines. It lets doctors give quick and effective treatment.
Two-Bolus Administration Protocol
Reteplase is given in two doses, 30 minutes apart. This method works well for fast clot dissolving. It’s simple, which is great for emergencies
This two-dose method is a big plus. It avoids the need for constant infusion and cuts down on mistakes. This makes reteplase a good choice for heart attacks and possibly other clotting issues.
Primary Use in Myocardial Infarction and Expanding Applications
Reteplase is mainly for heart attacks. It’s proven to be effective and is a top choice. Researchers are also looking into using it for other clot problems, like in the lungs or legs.
As we learn more about how it works, reteplase might be used more often. Its special features make it a strong candidate for treating different clot-related issues.
Streptokinase: Time-Tested Thrombolytic Agent
Streptokinase has been a key part of treating blood clots for many years. It works by breaking down fibrin, which is a major component of clots. This makes it a vital tool in managing acute thrombotic events.
Fibrinolysis Mechanism
Streptokinase turns plasminogen into plasmin, which then breaks down fibrin clots. This non-selective mechanism is effective but can affect the whole fibrinolytic system. It’s important to use it carefully.
The process starts with the formation of a streptokinase-plasminogen complex. This complex then converts other plasminogens into plasmin. This chain reaction is key to the drug’s ability to dissolve clots.
Cost-Effectiveness in Healthcare
Streptokinase is also cost-effective in healthcare. It’s cheaper than many other clot-dissolving drugs. This makes it more accessible to more patients.
| Treatment | Cost | Efficacy |
| Streptokinase | Lower | High |
| tPA | Higher | High |
| Tenecteplase | Highest | Very High |
This cost-effectiveness is very important in places where money is tight. It helps ensure more people can get the treatment they need.
Immunogenicity and Contraindications
Butt, streptokinase has immunogenicity concerns. It comes from beta-hemolytic streptococci. This can lead to the body making antibodies against it. This can make it less effective over time and cause allergic reactions.
There are also certain situations where streptokinase should not be used. These include recent streptococcal infections, known allergies to the drug, and previous exposure that led to significant antibody formation. It’s important to know a patient’s medical history before using streptokinase.
In summary, streptokinase is a valuable tool in fighting blood clots. Its ability to break down fibrin, cost-effectiveness, and the need to consider its side effects make it a complex but useful treatment.
Urokinase: Targeted Clot Dissolution Therapy
Urokinase is a strong thrombolytic agent for dissolving blood clots. It’s used in certain medical cases where its special properties help patients the most.
Direct Activation of Plasminogen at Clot Sites
Urokinase’s main benefit is activating plasminogen right at the clot. This targeted approach makes the treatment more precise. It reduces the chance of side effects happening all over the body.
Activating plasminogen directly is key for:
- Improving how well clots dissolve
- Lowering the risk of bleeding
- Having better control over the treatment
Catheter-Directed Thrombolysis Applications
Urokinase works great in catheter-directed thrombolysis (CDT). CDT uses a catheter to send the drug straight to the clot. This method is very effective for treating:
- Acute limb ischemia
- Deep vein thrombosis (DVT)
- Other peripheral arterial occlusions
Using urokinase in CDT quickly gets blood flowing again. It also helps avoid long-term damage to blood vessels.
Use in Peripheral Vascular Occlusions
Urokinase is also good for treating blockages in arteries and veins. Its ability to activate plasminogen makes it perfect for:
- Getting blood flow back to ischemic limbs
- Making symptoms of vascular blockages less severe
- Improving patient results
Healthcare providers use urokinase’s targeted action to treat complex vascular problems. This helps patients get better faster.
Conclusion: Choosing the Right Thrombolytic and Understanding Treatment Timing
We’ve looked at many drugs to break up clots, like tPA, alteplase, and tenecteplase. Each has its own use and how it’s given.
Choosing the right clot-dissolving drug depends on several things. These include the type of clot, when treatment starts, and the patient’s health. Knowing about these drugs and their uses is key to good treatment.
Getting the right treatment quickly is very important. For example, blood thinners can help with leg clotsbut the treatment must fit the patient’s needs.
Healthcare providers must consider each drug’s unique features and the patient’s situation. This way, they can make the best choices for treatment. Understanding all the options is essential for effective care.
FAQ
What are the most common medications used to dissolve blood clots?
Common medications for dissolving blood clots include tPA, alteplase, tenecteplase, reteplase, streptokinase, and urokinase. They are used for conditions like ischemic stroke and deep vein thrombosis.
How do clot dissolvers differ from blood thinners?
Clot dissolvers, or thrombolytics, break down blood clots. Blood thinners, or anticoagulants, stop new clots from forming and prevent existing ones from growing. Both are important in treating blood clots.
What is the role of tPA in thrombolytic therapy?
tPA is the top choice for breaking down clots. It’s used for conditions like ischemic stroke and is given quickly because time is critical.
What are the benefits of using alteplase in treating thrombotic events?
Alteplase is a first-line treatment for many clot types. It works fast and is key in emergencies.
How does tenecteplase compare to traditional tPA?
Tenecteplase is more specific to clots and lasts longer. It can be given all at once, which is better in emergencies. Studies show it’s as good as tPA, with some benefits.
What is the unique administration protocol for reteplase?
Reteplase is given in two doses, 30 minutes apart. This method is good for treating heart attacks and is used for other clots too.
What are the concerns associated with streptokinase?
Streptokinase is cheap but has risks. It can cause too much clot dissolving and may not work well if used again because of allergic reactions.
How is urokinase used in catheter-directed thrombolysis?
Urokinase is used to dissolve clots directly. It’s effective for treating blockages in blood vessels.
Can blood thinners dissolve existing blood clots?
No, blood thinners prevent new clots and stop existing ones from growing. To dissolve clots, thrombolytics are needed.
What is the importance of timely treatment in thrombolytic therapy?
Quick treatment is key because clot dissolvers work best when given fast. Early action is vital for the best results.
References
- Bates, S. M., Rajasekhar, A., Middeldorp, S., McLintock, C., Rodger, M. A., James, A. H., & Hunt, B. J. (2022). American Society of Hematology 2020 guidelines for management of venous thromboembolism: Treatment of deep vein thrombosis and pulmonary embolism. Blood Advances, 6(6), 1997-2029. U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8329651/




































