Last Updated on November 17, 2025 by Ugurkan Demir
At Liv Hospital, we know how vital our bodies are, and how essential blood cells are to our survival. Many people often ask, where are blood cells formed and how this process keeps us healthy.
Blood cells are mainly made in the bone marrow — a process called hematopoiesis. The bone marrow, found inside bones like the hips and thighbones, produces all types of blood cells.
Red blood cells, for example, are created in the bone marrow and last about 100–120 days in our bodies. Understanding where blood cells are formed helps us appreciate how the bone marrow supports life and ensures our body functions properly.
At Liv Hospital, we emphasize the importance of knowing which organ makes blood cells in adults. The bone marrow truly is key to our health, producing the blood cells we need every single day.
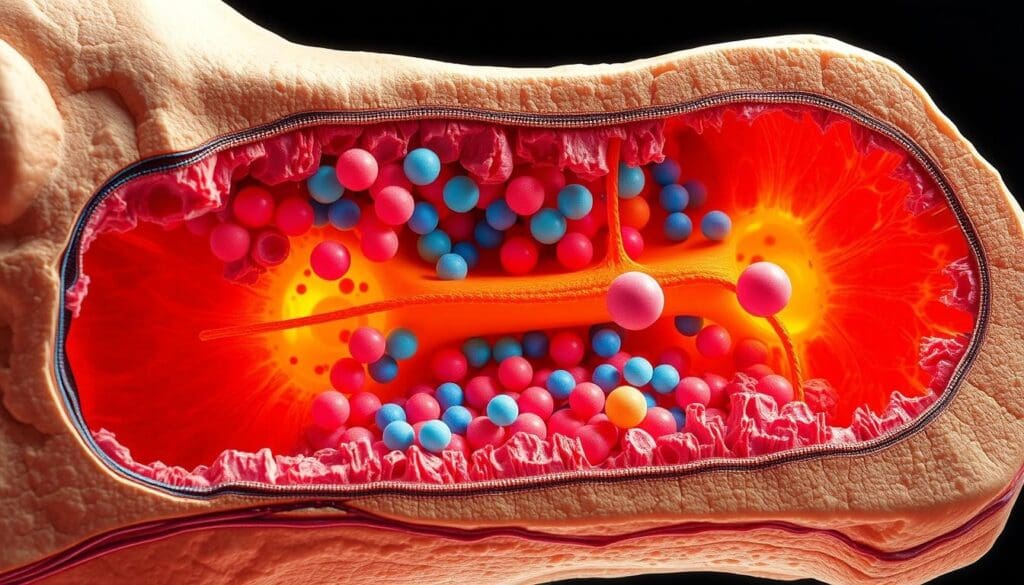
Blood is a complex fluid that keeps us alive. It carries vital substances all over the body. It’s a multifaceted tissue that does many important jobs to keep us healthy.
Blood has several key parts, each with its own role. It has red blood cells that carry oxygen. White blood cells fight infections and support our immune system. Platelets help stop bleeding when a vessel is injured.
These cells float in plasma, the liquid part of blood. Plasma also carries proteins, nutrients, and hormones.
The mix of blood components is amazing. It shows how different parts work together to keep us balanced. Knowing about blood helps us understand how our bodies work and react to health issues.
Blood does many important jobs in our bodies. It carries oxygen from the lungs to our tissues and carbon dioxide back to the lungs. It also brings nutrients from our digestive system to our cells and takes waste to organs like the kidneys and liver for removal.
Blood is also key in fighting infections. White blood cells protect us from germs and invaders. It helps keep our body’s acid-base balance and controls our body temperature.
Blood clotting is another vital function. It stops bleeding when a blood vessel is damaged. This process involves platelets and clotting factors in plasma, showing the complex ways blood works.
Hematopoiesis is how our bodies make blood cells. It’s key to keeping us alive. It starts with hematopoietic stem cells in the bone marrow.
Hematopoiesis means making all blood cell types from stem cells. It keeps our blood flowing with red, white cells, and platelets. It’s a series of steps where stem cells grow and change into different blood cells.
It starts with stem cells that can grow and change into any blood cell. They go through stages, guided by growth factors and cytokines, to become specific cells.
The blood cells’ take is complex and controlled. Stem cells first split into myeloid or lymphoid cells. Myeloid cells make red blood cells, platelets, and more. Lymphoid cells turn into T cells, B cells, and natural killer cells.
Each type of cell goes through steps to become what it is. For example, red blood cells lose their nucleus and get more hemoglobin. Platelets come from megakaryocytes breaking apart.
Knowing how these paths work helps us understand how our bodies keep blood cells in balance. This balance is key to health and fighting off diseases.
Blood cell formation, or hematopoiesis, mainly happens in the bone marrow of adults. This complex process is key to making the different blood cells our body needs to work properly
The bone marrow is a spongy tissue inside bones like the hips and thighbones. It makes blood cells. It’s the main place for blood cell production, making red blood cells, white blood cells, and platelets.
The bone marrow has stem cells, which turn into different blood cells.
“The bone marrow is the main place for blood cell making in adults, making billions of blood cells every day,” say hematology experts. This is key to keeping the right balance of blood cells in our body.
In adults, the pelvis, spine, ribs, and sternum are key to blood cell making. These bones have red bone marrow, which is where blood cells are made. The pelvis is very important, making a lot of our blood cells.
Bone marrow can be red or yellow, depending on its role. Red bone marrow is where blood cells are made, with blood vessels and stem cells. Yellow bone marrow is mostly fat and doesn’t make blood cells.
| Characteristics | Red Bone Marrow | Yellow Bone Marrow |
| Main Function | Hematopoiesis (blood cell production) | Fat storage |
| Cell Composition | Stem cells, blood vessels | Fat cells |
In summary, the bone marrow, mainly in the pelvis, spine, ribs, and sternum, is where blood cells are made in adults. Knowing about red and yellow bone marrow helps us understand how our body makes blood cells.
Hematopoietic stem cells are at the center of blood production. They can turn into different blood cell types. These cells are key to making blood cells throughout our lives.
Hematopoietic stem cells have special traits for blood production. They can self-renew, keeping a steady supply of stem cells. They can also differentiate into all blood cell types, like red and white blood cells, and platelets.
One important trait is their ability to stay dormant until needed. This lets them quickly respond to the body’s blood cell needs. For example, during hard exercise or at high altitudes, more red blood cells are needed for oxygen.
The self-renewal of hematopoietic stem cells keeps their numbers steady in the bone marrow. This ensures a ready supply of stem cells to turn into different blood cells as needed.
Differentiation is when stem cells become specific blood cells. This involves many changes that lead to mature blood cells. The process is controlled by growth factors and signals in the bone marrow.
The bone marrow has a special area called the stem cell niche. It supports the survival and function of hematopoietic stem cells. This niche includes various cells that help regulate stem cell behavior.
The stem cell niche is vital for balancing self-renewal and differentiation. It provides the signals and growth factors needed for stem cell development. Knowing about the stem cell niche is key to therapies to improve blood cell production in blood disorders.
In summary, hematopoietic stem cells are vital for blood production in humans. Their unique traits and the supportive bone marrow environment allow for constant blood cell production. This complex process is essential for keeping the body balanced and responding to blood cell needs.
Red blood cell production, or erythropoiesis, is a complex process. It starts with hematopoietic stem cells in the bone marrow. These cells turn into mature erythrocytes, which are vital for oxygen delivery in the body.
Erythropoiesis begins with hematopoietic stem cells in the bone marrow. They differentiate into erythrocyte progenitor cells. These cells go through several stages of maturation.
During these stages, cells undergo significant changes. They lose their nucleus and most organelles. This is to optimize their function in oxygen delivery.
Erythropoietin (EPO) is a hormone made mainly by the kidneys. It’s produced when oxygen levels are low. EPO helps erythrocyte progenitor cells survive, grow, and differentiate.
Erythropoietin’s key functions include:
The body’s oxygen levels control red blood cell production. When oxygen is low, the kidneys make more EPO. This stimulates erythropoiesis.
As red blood cells increase, oxygen delivery gets better. EPO production then goes down. This creates a negative feedback loop that keeps the body in balance.
This complex regulation ensures the body has the right number of red blood cells. It adapts to changes in altitude, physical activity, and other factors that affect oxygen demand.
White blood cells are key to our immune system, fighting off infections. They are also known as leukocytes. These cells protect us from bacteria, viruses, and other harmful substances. Making white blood cells is a complex process involving many cell types and regulatory mechanisms.
There are five main types of white blood cells, each with its own role. These include:
Together, these cells offer a strong immune defense.
White blood cells start with hematopoietic stem cells in the bone marrow. These stem cells turn into different progenitor cells. Then, these cells mature into the various white blood cell types. The maturation process involves growth, differentiation, and becoming fully functional.
Table: White Blood Cell Development Stages
| Cell Type | Progenitor Cell | Maturation Site |
| Neutrophils | Myeloblast | Bone Marrow |
| Lymphocytes | Lymphoblast | Lymphoid Organs |
| Monocytes | Monoblast | Bone Marrow |
| Eosinophils | Myeloblast | Bone Marrow |
| Basophils | Myeloblast | Bone Marrow |
Many factors can trigger the production of white blood cells. This includes infections, inflammation, and immune responses. When the body finds pathogens, it sends out cytokines and other signals. These signals help make more white blood cells to fight the infection and get us healthy again.
In the bone marrow, a fascinating process unfolds as megakaryocytes mature and release platelets into the bloodstream. This complex process is vital for our body’s ability to form blood clots and prevent excessive bleeding.
Megakaryocytes are giant cells in the bone marrow that produce platelets. They go through maturation steps, becoming polyploid. This means they have multiple sets of chromosomes, allowing them to produce a large number of platelets.
“The process of megakaryocyte maturation is tightly regulated and involves the coordinated action of various growth factors and cytokines,” as noted by hematologists studying blood cell formation.
As megakaryocytes mature, they extend long, thin processes called proplatelets into the bone marrow sinusoids. These proplatelets are then fragmented into individual platelets, which are released into the circulation. This process is remarkable for its efficiency, producing billions of platelets daily.
The release of platelets is a critical step in maintaining the body’s hemostatic balance. Any disruption in this process can lead to bleeding disorders or thrombotic complications.
The production of platelets is regulated by a complex interplay of factors, including thrombopoietin, a hormone produced by the liver and kidneys. Thrombopoietin stimulates the proliferation and maturation of megakaryocytes, ensuring that platelet production meets the body’s needs.
In conclusion, platelet formation is a vital process that ensures our body’s ability to clot blood effectively. Understanding this process provides insights into the complex mechanisms that maintain our health.
Blood cell maturation doesn’t stop in the bone marrow. Other organs take over at different stages. The thymus, spleen, and lymph nodes are key in this process.
The thymus is vital for T lymphocytes (T cells) maturation. It’s behind the sternum and is most active in kids and teens. After puberty, it shrinks and works less.
“The thymus is responsible for the education of T cells, ensuring they can distinguish between self and non-self antigens.”
T cells in the thymus go through selection. This means they learn not to attack the body’s own cells. This helps prevent diseases like autoimmune ones.
The spleen is in the upper left of the abdomen. It filters blood, getting rid of old or damaged red blood cells. It also recycles iron.
The spleen is a storage place for immune cells. It releases them when needed. It also makes antibodies to fight infections.
| Organ | Function in Blood Cell Maturation |
| Thymus | T cell maturation and selection |
| Spleen | Blood filtration, lymphocyte development, and antibody production |
| Lymph Nodes | B cell maturation and antibody production |
Lymph nodes are all over the body. They’re key for B lymphocytes (B cells) maturation. Inside, B cells become activated, grow, and turn into antibody-making plasma cells.
This process involves many cells and signals. It leads to the creation of antibodies that fight specific pathogens.
In conclusion, the thymus, spleen, and lymph nodes are vital for blood cell maturation. Each plays a unique role in the development and function of immune cells.
We make about 100 billion blood cells every day. This shows how complex and efficient our body’s hematopoietic system is. It’s not just a number; it’s proof of our body’s ability to stay balanced and adapt.
The creation of blood cells is carefully managed. It balances making new cells with getting rid of old or damaged ones. This balance keeps the number of blood cells steady, even with constant turnover.
A key part of this balance is controlling hematopoiesis, the making of blood cells. Hematopoiesis happens mainly in the bone marrow. It’s influenced by growth factors and cytokines.
“The hematopoietic system has an incredible capacity for regeneration and adaptation, allowing it to respond to a wide range of physiological demands and pathological insults.”
Blood cells live for different lengths of time, from hours to years. Knowing these lifespans helps us understand how blood cell production works.
| Blood Cell Type | Average Lifespan |
| Red Blood Cells | Approximately 120 days |
| Platelets | 8-12 days |
| White Blood Cells | Varies (e.g., neutrophils: 5-6 days, lymphocytes: months to years) |
Keeping blood cell production in balance is complex. It involves feedback mechanisms and regulatory pathways. The body checks the levels of different blood cells and adjusts production as needed.
For example, red blood cell production is controlled by erythropoietin. This hormone is made by the kidneys when oxygen levels are low. Platelet and white blood cell production are also influenced by growth factors and cytokines.
This complex interaction helps the body keep the right number of blood cells. This ensures it can respond quickly to any challenge or demand.
Many disorders can mess up how blood cells are made, causing health problems. Making blood cells is a complex job that needs many cell types and growth factors working together. If this process goes wrong, it can lead to different disorders.
The bone marrow is key in making blood cells. Problems with the bone marrow can really affect how blood cells are produced.
Bone marrow failure syndromes happen when the bone marrow can’t make enough blood cells. This can cause anemia, infections, and bleeding problems. Aplastic anemia is when the bone marrow can’t make new blood cells. This leads to feeling tired, weak, and more likely to get infections.
There are many reasons for bone marrow failure, like toxins, some medicines, and viruses. Treatment might include fixing the cause or using immunosuppressive therapy or a bone marrow transplant.
Blood cancers, like leukemia, lymphoma, and myeloma, happen when genes that control blood cell production get messed up. This can cause abnormal blood cells to grow too much. Leukemia is when white blood cells grow too much, leading to infections, anemia, and bleeding.
Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. MDS can turn into acute myeloid leukemia (AML) in some cases. Knowing the exact type of blood cancer or dysplasia is key to the right treatment.
Modern medicine has made big strides in treating blood cell formation disorders. Now, we have targeted therapies, immunotherapies, and stem cell transplants. For example, bone marrow transplantation can save lives for people with bone marrow failure syndromes or certain blood cancers.
Gene therapy is also being explored for genetic disorders affecting blood cell production. The field is always growing, giving new hope to those with these complex conditions.
| Disorder | Characteristics | Treatment Options |
| Aplastic Anemia | Failure of the bone marrow to produce blood cells | Immunosuppressive therapy, bone marrow transplantation |
| Leukemia | Abnormal proliferation of white blood cells | Chemotherapy, targeted therapy, and stem cell transplantation |
| Myelodysplastic Syndromes (MDS) | Poorly formed or dysfunctional blood cells | Supportive care, immunosuppressive therapy, and stem cell transplantation |
It’s important to understand the disorders that affect blood cell formation to find good treatments. Research is always finding new things about these disorders, leading to new therapies.
We’ve looked into how blood cells are made, focusing on where they are created and which organ makes blood in adults. The bone marrow is key, producing about 2-3 million red blood cells every second. This process turns hematopoietic stem cells into red, white blood cells, and platelets.
The making of blood cells is tightly controlled, with many factors affecting how fast it happens. For example, erythropoietin from the kidneys is vital for red blood cell creation. Knowing how blood is made in our bodies helps us understand how we stay healthy.
In summary, the blood-making system is amazing and vital for our lives. We’ve seen how the bone marrow creates blood cells and how different factors influence this. By understanding where blood cells are made in adults, we can appreciate the complexity of our bodies.
In adults, the bone marrow is where blood cells are made. It produces all blood cell types, like red and white blood cells, and platelets.
Blood cells are made in the bone marrow. It’s found in the pelvis, spine, ribs, and sternum. The bone marrow has stem cells that turn into different blood cells.
Hematopoiesis is how stem cells turn into blood cells. It makes red, white blood cells, and platelets. These cells are key to staying healthy.
Erythropoietin is a hormone from the kidneys. It helps make red blood cells when the body needs more oxygen.
White blood cells come from leukopoiesis. It’s when stem cells turn into different white blood cells. These cells fight infections and diseases.
The thymus helps T cells mature. It’s important for T cell education. This ensures T cells can fight off pathogens.
Platelets are made through thrombopoiesis. It’s when megakaryocytes in the bone marrow release platelets. Platelets help with blood clotting.
Different blood cells live for different times. Red blood cells last about 120 days. White blood cells and platelets have shorter lifespans.
The body keeps blood cell production balanced through feedback mechanisms. These ensure blood cell counts stay normal, even when the body changes.
Disorders like bone marrow failure and blood cancers can affect blood cell production. These can be serious for health.
Blood cancers and dysplasias are treated with chemotherapy, radiation, and bone marrow transplants. These aim to fix blood cell production and manage the condition.
London Health Sciences Centre. Blood and bone marrow health.
PubMed Central. Structural organization of bone marrow and hematopoiesis.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!