Last Updated on November 17, 2025 by Ugurkan Demir
Getting a stem cell transplant can feel overwhelming. Before it, patients go through a preparative regimen called stem cell conditioning. This step is key to removing sick cells and making room for new ones.What chemo is used before stem cell transplant? Get the crucial and powerful guide to stem cell conditioning protocols now.
At Liv Hospital, we know how vital the right conditioning chemotherapy is. We focus on each patient, using the latest and best treatments. This guide will look at the chemotherapies used before a transplant. We’ll cover myeloablative and reduced-intensity conditioning.

Stem cell transplantation is a key treatment for many diseases. It involves moving stem cells into a patient’s body to replace bad bone marrow. We’ll look at the basics of stem cell transplantation, its role in treatment, and the different types.
Stem cell transplants are vital for treating serious diseases. They can cure some types of leukemia and lymphoma. By replacing bad bone marrow with healthy stem cells, SCT treatment can save lives.
The process starts with conditioning therapy to get the patient ready. Then, stem cells are infused. These cells go to the bone marrow and start making healthy blood cells.
There are two main types of stem cell transplants: autologous and allogeneic. Autologous transplants use the patient’s own stem cells. These are collected, stored, and then given back after treatment. This is often for patients with lymphoma or multiple myeloma.
Allogeneic transplants use stem cells from a donor. This is usually for patients with leukemia. Allogeneic transplants also have a graft-versus-tumor effect. This means the donor’s immune cells can fight cancer cells.
| Transplant Type | Stem Cell Source | Common Uses |
| Autologous | Patient’s own stem cells | Lymphoma, Multiple Myeloma |
| Allogeneic | Donor stem cells | Leukemia, Other Hematological Disorders |
Conditioning, or the preparative regimen, is key in stem cell transplantation. It prepares the body for new stem cells, aiming for a successful transplant.
The main goal is to create space in the bone marrow for new stem cells. This is vital when the bone marrow is full of diseased cells.
The conditioning regimen eradicates existing cells. This makes room for the new stem cells to grow and produce healthy blood cells.
Another key goal is to eliminate diseased cells in the body. High-dose chemotherapy and/or radiation therapy are used to target and destroy cancer cells.
The preparative regimen also aims to suppress the patient’s immune system. This is to prevent it from rejecting the new stem cells. This is most important in allogeneic transplants, where the donor cells are seen as foreign.
By weakening the immune system, the conditioning regimen helps the new stem cells to engraft and work well. This reduces the chance of graft rejection and other issues.
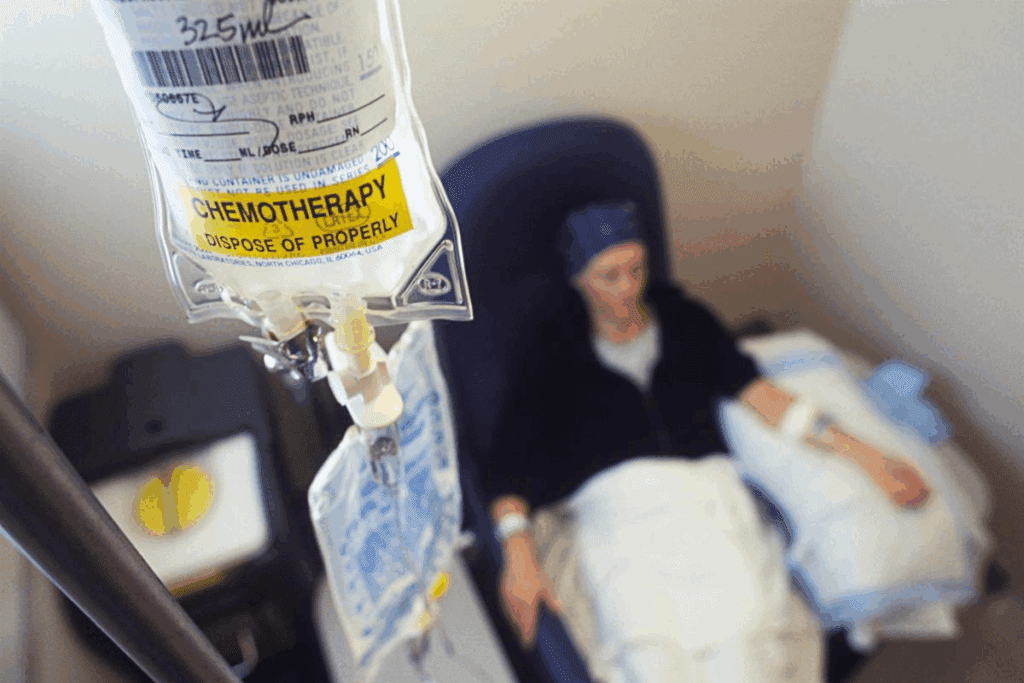
Chemotherapy is key before a stem cell transplant. It kills diseased cells and makes room for new ones. The choice of chemo and how intense it is depends on the disease, the patient’s health, and the transplant type.
Many chemotherapy agents are used before a stem cell transplant. These include:
These agents are picked for their ability to kill cancer cells. They also help in allogeneic transplants by suppressing the immune system to prevent rejection.
Radiation therapy is also used in conditioning, often in myeloablative conditioning. Total Body Irradiation (TBI) gives a uniform dose of radiation to the whole body. It is used to:
TBI is often combined with chemo to boost its effectiveness.
The timing and administration of conditioning therapy are carefully planned. It is given over several days before the stem cell transplant. The exact schedule depends on the chemo agents and if radiation is used.
In a typical myeloablative regimen, chemo is given over 4 to 7 days. TBI is given in fractions over 1 to 4 days. The stem cell transplant happens within 24 to 48 hours after conditioning is finished.
Myeloablative conditioning (MAC) has been around for decades. It prepares patients for stem cell transplants. This method uses high-dose chemotherapy to kill diseased cells and make room for new stem cells.
MAC destroys the patient’s bone marrow completely. This gets rid of any cancer cells. It works by using high-dose chemotherapy that targets fast-growing cells, like cancer and bone marrow cells.
Busulfan is a key chemotherapy drug in MAC. It’s often paired with cyclophosphamide for a strong regimen. These regimens are effective against cancers like leukemia and lymphoma.
Cyclophosphamide is another important drug in MAC. It’s often mixed with total body irradiation (TBI) or busulfan. This mix is effective against many blood cancers.
Using different chemotherapy drugs together is common in MAC. Mixing agents like busulfan and cyclophosphamide makes the regimen stronger. This targets more cancer cells and can lower the chance of cancer coming back.
Total body irradiation (TBI) is a key part of myeloablative conditioning before stem cell transplants. It delivers radiation to the whole body. This kills cancer cells and weakens the immune system. It’s vital for some patients.
TBI is for patients with blood cancers like leukemia or lymphoma. It’s used when the disease is widespread or could affect the brain. Doctors decide based on the disease type, stage, patient’s age, and health.
TBI is often paired with chemotherapy. This combo is more effective in killing cancer cells and weakening the immune system. It lowers the chance of cancer coming back after the transplant. Chemotherapy agents like cyclophosphamide and etoposide are commonly used.
| Chemotherapy Agent | Role in Conditioning | Common Side Effects |
| Cyclophosphamide | Eradicates malignant cells and suppresses the immune system | Nausea, vomiting, hair loss |
| Etoposide | Targets malignant cells, enhances immunosuppression | Hair loss, mucositis, fatigue |
TBI can cause side effects like nausea, vomiting, and organ damage. Patients get support care to manage these. This includes antiemetic meds, hydration, and nutrition. Long-term issues like cataracts and secondary cancers also need watching.
Understanding TBI’s role helps patients grasp their treatment. It shows the efforts made to make their stem cell transplant successful.
Reduced-intensity conditioning (RIC) is a gentler way to prepare for stem cell transplants. It uses lower doses of chemotherapy. This is good for older patients or those with health issues who can’t handle strong treatments.
RIC uses lower chemotherapy doses than traditional methods. It aims to weaken the immune system enough for donor stem cells to take hold. At the same time, it tries to keep side effects down. This makes RIC a better option for many patients who were once too old or frail for traditional treatments.
Fludarabine is a key part of many RIC plans. It’s often mixed with other drugs like busulfan or melphalan. Fludarabine-based regimens are chosen for their balance of effectiveness and safety, making them a favorite for RIC.
Melphalan is used in RIC, mainly for patients with certain cancers like multiple myeloma. In RIC, melphalan is given in lower doses. This reduces the risk of serious side effects while keeping the disease under control.
There are other RIC plans being tested and used, too. These might include different chemotherapy mixes, targeted therapies, or new ideas. The right RIC plan depends on the patient’s disease, health, and who the donor is.
BEAM conditioning is a key part of treating lymphoma with stem cell transplants. It kills cancer cells and gets the body ready for the transplant. We’ll look at what the BEAM protocol includes, how well it works, and its side effects.
The BEAM protocol uses four main drugs:
Together, these drugs help get rid of lymphoma cells.
BEAM conditioning works well for many lymphoma types, like Hodgkin and non-Hodgkin lymphoma. It helps achieve complete remission and improves survival rates, making it a good treatment choice.
BEAM conditioning is effective but has serious side effects, including:
Myeloablative conditioning (MAC) and reduced-intensity conditioning (RIC) are two ways to prepare for stem cell transplants. Each has its own benefits and risks. The right choice depends on the patient’s age, health, and the type of disease.
Relapse is a big worry in stem cell transplants. MAC is linked to lower relapse rates in younger patients with some leukemias. But long-term survival also depends on the disease and the patient’s health.
A study on acute myeloid leukemia showed MAC had lower relapse rates. Yet, overall survival was similar because MAC had higher treatment-related deaths.
Treatment-related mortality (TRM) is key when picking between MAC and RIC. MAC has a higher TRM because it’s more intense. This can cause more side effects and problems. RIC, being less toxic, has lower TRM, making it better for older patients or those with health issues.
Quality of life (QoL) is important when looking at MAC vs. RIC. MAC might control the disease better but its high toxicity can harm QoL. RIC, being less intense, might improve QoL in the short term but raises concerns about relapse.
In the end, choosing between MAC and RIC should match the patient’s specific needs. This includes their health, disease, and personal wishes.
Choosing the right conditioning regimen is complex. It depends on several key factors. Healthcare providers look at many elements to pick the best regimen for each patient.
A patient’s age and health are key in choosing a conditioning regimen. Older patients or those with health issues might need a gentler approach. This reduces the risk of side effects.
We use special tools to check a patient’s health and function. This helps us make the regimen fit the patient’s needs. We aim to control the disease while keeping risks low.
The disease type and status also play a big role. For some diseases, a stronger regimen is needed. But for others, a gentler approach might be better.
We look at the disease stage, past treatments, and how well the patient has responded. This tailored approach helps improve outcomes and lower the chance of the disease coming back.
In allogeneic stem cell transplants, the donor matters a lot. We consider HLA matching, donor age, and health when choosing the regimen.
| Donor Characteristic | Impact on Conditioning Regimen |
| HLA Matching | Influences the risk of graft-versus-host disease (GVHD) and may affect the intensity of conditioning required. |
| Donor Age | Older donors may be associated with increased risk of GVHD or other complications. |
| Donor Health Status | Affects the quality of the stem cells and the donor’s ability to donate. |
We tailor conditioning regimens to each patient’s unique needs. This might mean combining different treatments or using new therapies. It aims to make the regimen more effective.
Our goal is to find the safest and most effective regimen for each patient. This approach improves treatment results and enhances care quality for those undergoing stem cell transplants.
Recent studies have greatly improved our understanding of conditioning before stem cell transplantation. We now know more about how different approaches affect patient outcomes. This knowledge is helping us make better choices for our patients.
Myeloablative Conditioning (MAC) works best for young, fit patients. It helps them survive longer and reduces the chance of cancer coming back. This is because MAC is strong enough to kill off cancer cells effectively.
A study in a top medical journal showed MAC’s success. Young patients who got MAC had fewer cancer relapses than those who got reduced-intensity conditioning (RIC). This makes MAC a good choice for eligible patients.
Reduced-Intensity Conditioning (RIC) is better for older patients or those with health issues. It’s less harsh than MAC but can also prepare the body for a transplant. This makes RIC a safer option for those who can’t handle MAC.
Studies have shown RIC works as well as MAC for older or weaker patients. It also lowers the risk of death from treatment. This makes RIC a great choice for patients who can’t handle MAC.
| Conditioning Regimen | Patient Profile | Survival Outcomes |
| MAC | Younger, fit patients | Improved long-term survival, reduced relapse |
| RIC | Older patients or those with comorbidities | Comparable survival to MAC, reduced treatment-related mortality |
The field of stem cell transplantation is seeing new ways to condition patients. These new methods aim to improve survival rates and reduce side effects. They use targeted therapies to kill cancer cells or boost the immune system.
Early trials of these new methods are showing promise. Some studies suggest better survival rates and fewer side effects. As research continues, we can expect even more effective and personalized treatments.
We are committed to keeping up with these advances. We want to give our patients the best care possible.
It’s key to manage side effects of pre-transplant chemotherapy well. This ensures patients can handle the treatment and recover well. Pre-transplant chemotherapy, or conditioning, gets the body ready for a stem cell transplant. It kills off diseased cells and weakens the immune system.
Acute side effects from pre-transplant chemotherapy can be tough and varied. Common ones include nausea, vomiting, fatigue, hair loss, and mucositis. We tackle these side effects with a mix of medicines and supportive care.
For example, we use antiemetic drugs to fight nausea and vomiting. We also have pain management plans for mucositis. Plus, nutritional support is key to keeping patients strong during this tough time.
Long-term issues can also come from pre-transplant chemotherapy. These might include infertility, a higher risk of secondary cancers, and organ damage. We talk to patients about these risks to make sure they know what to expect.
Long-term care is important to watch for and manage these complications. This includes regular health checks, monitoring of organ function, and steps to lower risks.
Supportive care is vital for patients going through pre-transplant chemotherapy. It’s not just about medical help but also emotional and psychological support. We offer counseling, support groups, and nutritional advice to help patients deal with the treatment.
Keeping a close eye on patients during and after pre-transplant chemotherapy is key. Regular checks let us adjust treatments, manage side effects, and quickly tackle any problems.
We also teach patients about sticking to their treatment plan and keeping up with follow-ups. By working together, we aim to improve outcomes and support patients through their recovery.
| Side Effect | Management Strategy |
| Nausea and Vomiting | Antiemetic medications |
| Mucositis | Pain management, oral care |
| Fatigue | Nutritional support, rest |
Stem cell transplant conditioning is changing fast. New methods are being found to make treatments better and safer. We’ve talked about the different ways to prepare for a transplant, like myeloablative and reduced-intensity conditioning.
The future looks bright for stem cell transplant conditioning. Scientists are working hard to make treatments even better. By keeping up with the latest news, patients and doctors can make better choices together. Soon, we’ll see treatments that are more tailored to each person, making life better for those getting transplants.
Stem cell conditioning, or a preparative regimen, gets the body ready for a stem cell transplant. It uses chemotherapy and sometimes radiation to kill off sick cells. This makes room for new stem cells to grow.
The chemotherapy used can change based on the transplant type, disease, and patient health. Common agents include busulfan, cyclophosphamide, fludarabine, and melphalan.
Myeloablative conditioning (MAC) uses strong chemotherapy to clear out sick cells. Reduced-intensity conditioning (RIC) uses lower doses. MAC is for younger, healthier patients, while RIC is for older or sicker patients.
BEAM conditioning is a chemotherapy mix used mainly for lymphoma patients. It includes BCNU, etoposide, cytarabine, and melphalan. It prepares lymphoma patients for a stem cell transplant.
Choosing the right conditioning regimen depends on many factors. These include the patient’s age, health, disease type, and the donor. Healthcare teams tailor a plan to each patient’s needs.
Pre-transplant chemotherapy can cause various side effects. Supportive care, monitoring, and follow-up are key to managing these. Patients should talk to their healthcare team about their specific risks and how to manage them.
Total body irradiation (TBI) is used in some conditioning regimens, often with chemotherapy. It kills off sick cells and weakens the immune system. TBI is mainly used in myeloablative conditioning.
New research shows the benefits and outcomes of different conditioning regimens. Emerging targeted conditioning aims to improve treatment results. Staying updated is important for patients and healthcare providers to work together for better outcomes.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!