Last Updated on November 4, 2025 by mcelik

Did you know that lower back pain affects millions of people worldwide? A lot of this pain comes from herniated disc symptomsA herniated disc occurs when the soft inner gel leaks through a tear in the outer disc. This can irritate nearby nerves and cause symptoms. Learn about main Herniated Disc Symptoms, including pain, numbness, and tingling in the spine.
It’s important to know the signs and sciatica symptoms of a herniated disc. This helps you know when to get medical help. We’ll look at the common signs of a herniated disc, so you can understand when to seek help.
The spine has many parts, including spinal discs. These discs act as cushions between the vertebrae. They support the spine and help it move.
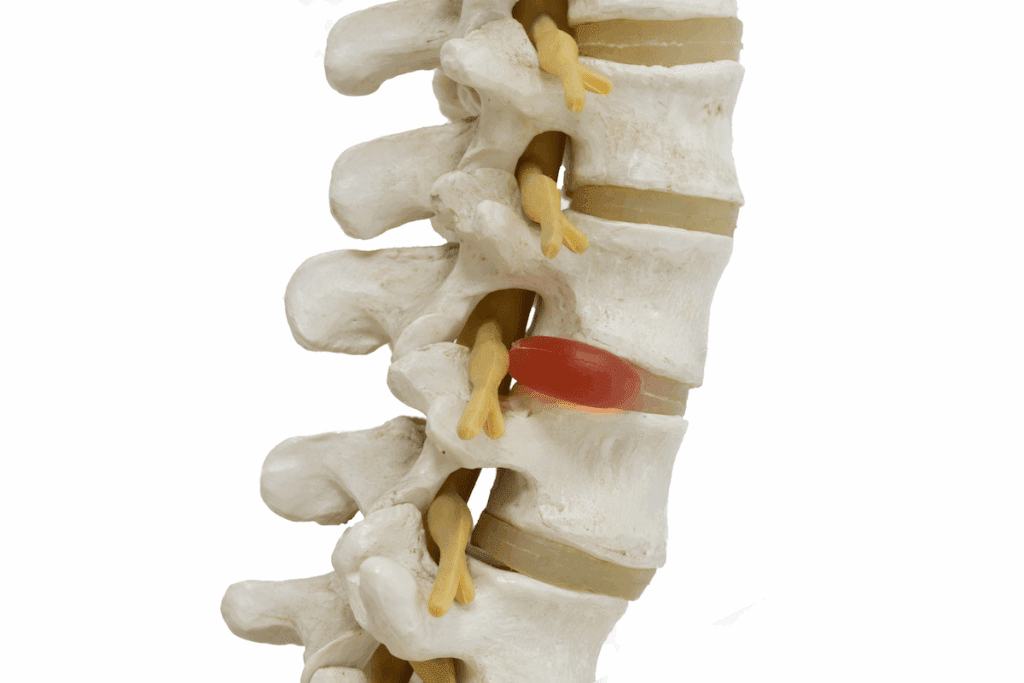
A spinal disc has two main parts: the nucleus pulposus and the annulus fibrosus. The nucleus pulposus is soft and gel-like, absorbing shock. The annulus fibrosus is tougher and outer, holding the nucleus. They work together to spread pressure evenly.
Spinal discs are key for flexibility and absorbing shock. But, they can get damaged and degenerate. This can happen due to age-related degeneration, postural strain, and repetitive lifting injuries.
Disc herniation happens when the outer layer (annulus fibrosus) tears or cracks. This lets the soft inner gel (nucleus pulposus) leak out. This can press on nerves, causing pain, numbness, and weakness. Many things can cause disc herniation, like wear and tear, injury, or strain.
Knowing how disc herniation happens is key for preventing and treating it. Keeping the spine healthy through good posture, exercise, and avoiding strain can lower the risk of a herniated disc.
Knowing the signs of a herniated disc is key for quick diagnosis and treatment. A herniated disc can press on or irritate nearby nerves. This can cause different symptoms in people, based on the herniation’s size and location, and the person’s health.
Pain is a common symptom of a herniated disc. This pain can be in the herniation area or spread along the nerve path. For example, a lumbar herniation can cause radiating pain down the leg, known as sciatica.
The pain’s intensity can vary and may worsen with certain movements or positions.
Numbness and tingling are also common symptoms. When a nerve is compressed or irritated, it can disrupt normal nerve function. This can cause numbness or tingling in the affected limb.
For example, a cervical spine herniation can lead to numbness or tingling in the arm or hand. These feelings can be uncomfortable and may affect daily activities.
Muscle weakness is another significant symptom of a herniated disc. When a nerve controlling muscle movement is compressed, it can cause muscle weakness. This weakness can make everyday tasks harder and, if not treated, may lead to more problems.
For instance, leg weakness can affect mobility and increase the risk of falls.
It’s important to recognize these three main signs—pain, numbness and tingling, and muscle weakness—to seek medical help. Early diagnosis and treatment can greatly improve outcomes for those with herniated discs.
The pain from herniated discs is complex and varies among people. Knowing these pain patterns is key for diagnosis and treatment.
The spot of the herniated disc affects the pain. For example, a lumbar herniation can cause lower back pain that spreads to the legs. This is often called sciatica.
A cervical herniation, on the other hand, can lead to neck pain. This pain can move to the arms, shoulders, and upper back.
Moving can make herniated disc pain worse. Bending, twisting, or lifting heavy things puts more pressure on the disc. This increases the pain, known as pain aggravated by movement.
Resting can help, but how much relief it brings depends on the herniation’s severity and the person’s tolerance.
Many people with herniated discs face chronic back pain. Knowing what activities or positions make pain worse is important. By avoiding these, patients can find pain relief with rest and other treatments.
It’s important to understand the neurological symptoms of a herniated disc. This is key for the right diagnosis and treatment. When a disc herniates, it can press on or irritate nearby nerves. This leads to various neurological problems.
Radiculopathy happens when a nerve root gets compressed or damaged. This causes pain, numbness, tingling, and weakness in the areas the nerve serves. Cervical radiculopathy affects the neck and arm. Lumbar radiculopathyimpacts the lower back and legs.
Nerve root compression happens when the herniated disc material presses on the nerve root. This disrupts its function. Symptoms include pain that spreads along the nerve’s path, numbness or tingling, and muscle weakness.
| Condition | Symptoms | Affected Areas |
| Cervical Radiculopathy | Pain, Numbness, Tingling, Weakness | Neck, Arm, Hand |
| Lumbar Radiculopathy | Pain, Numbness, Tingling, Weakness | Lower Back, Leg, Foot |
The neck is a common spot for herniated discs. This can lead to symptoms that affect daily life. A herniated disc in the neck can press on nerves, causing various symptoms.
Cervical herniated discs often cause pain in the neck and arm. This pain can feel sharp or dull. It helps doctors figure out where and how bad the herniation is.
A disc at C6-C7 might make pain go down to the arm and hand. This is just one example.
Moving your head or lifting heavy things can make this pain worse. Knowing how pain moves can help doctors find and treat the problem.
| Symptom | Description | Common Causes |
| Neck Pain | Dull or sharp pain in the neck | Herniated disc, muscle strain |
| Arm Pain | Radiating pain down the arm | Nerve compression, disc herniation |
| Upper Extremity Weakness | Weakness or tingling in the arm or hand | Nerve root compression |
People with cervical herniated discs might also feel weakness and tingling in their arms. This happens when nerves get compressed or irritated. The nerves affected decide where the weakness and tingling show up.
For instance, a C7 nerve root issue can cause triceps and wrist extensor weakness. It can also make the middle finger tingle. Spotting these patterns helps doctors diagnose cervical radiculopathy and other issues.
Lumbar disc herniation shows clear symptoms that need attention. When a disc in the lower back herniates, it can bother nearby nerves. This leads to various symptoms.
Lower back pain is a main symptom of a lumbar herniated disc. This pain can spread to the legs. It can feel different in strength and might be joined by leg pain, numbness, or tingling.
Pain that goes down the leg, following the sciatic nerve, is a common sign. This usually means there’s a lumbar herniated disc.
Sciatica is a key sign of a lumbar herniated disc. It causes pain, numbness, or weakness that goes down the sciatic nerve. This usually affects one leg.
Sciatica symptoms, like sciatica symptoms of pain, numbness, or tingling in the leg, point to a lumbar herniated disc. We’ll explore how lumbar herniated discs and sciatica are linked. This is why getting the right diagnosis and treatment is so important.
Herniated disc symptoms can really change someone’s daily life. They can affect how well you move, sleep, and feel overall. How much they impact you depends on how bad the herniation is and your health.
A herniated disc can cause a lot of pain and discomfort. This pain can make it hard to do simple things like bend, lift, or even walk. The pain can be so bad that it limits how much you can move, making everyday tasks hard.
It’s important for people with a herniated disc to stay independent. So, finding ways to manage symptoms is key.
People with a herniated disc often have trouble sleeping. The pain and discomfort make it hard to find a comfy sleeping spot. This can lower their energy and affect their quality of life.
We know that managing sleep and quality of life is vital for those with a herniated disc. Understanding how symptoms affect daily life helps us see the need for care that covers physical and emotional well-being.
Diagnosing herniated discs right means knowing how to tell them apart from muscle strain and arthritis. We need to look closely at the symptoms to treat them well.
Muscle strain and disc herniation can seem similar, with pain and less mobility. But, the pain’s feel and other symptoms can tell them apart.
Arthritis and disc issues can look alike, making it key to tell them apart.
| Characteristics | Arthritis | Disc Herniation |
| Pain Location | Usually in joints, causing pain all over | Pain spreads along nerves |
| Associated Symptoms | May include stiff joints, swelling, and less movement | Often numbness, tingling, and weak muscles |
| Triggers | Worse with movement, better with rest | Worsened by certain actions or positions |
Knowing these differences helps doctors make better diagnoses and treatment plans.
Knowing the signs of a herniated disc is key to getting help fast. Some symptoms mean you need to see a doctor right away. This can stop problems from getting worse.
Cauda equina syndrome is a serious issue. It happens when nerves in the lower back get squished. This can cause permanent damage if not treated quickly.
Key symptoms of cauda equina syndrome include:
A medical expert says, “Cauda equina syndrome is a medical emergency. It needs quick attention to avoid permanent damage.”
“Prompt surgical intervention is often necessary to relieve compression on the nerves and restore function.”
Progressive neurological deficits mean symptoms get worse over time. This can be muscle weakness, numbness, or tingling. It shows nerve damage is getting worse.
| Symptom | Description | Implication |
| Muscle Weakness | Gradual loss of strength in muscles | Potential for significant impairment |
| Numbness or Tingling | Abnormal sensations in limbs | Nerve compression or damage |
| Loss of Reflexes | Diminished or absent reflexes | Neurological damage |
If you notice these signs, get medical help right away. Waiting can cause permanent harm. This can really affect your life.
It’s hard to spot these signs, but knowing them is the first step. If you see any, talk to a doctor without delay.
Doctors use many methods to find out if a herniated disc is present. It’s key to get a correct diagnosis for the right treatment.
The first step is a physical check-up. We look at muscle strength, reflexes, and how you feel to see if nerves are hurt. Tests like the straight leg raise can tell if a herniated disc is causing sciatica.
Imaging tests are vital to confirm a herniated disc. MRI (Magnetic Resonance Imaging) is best because it shows soft tissues clearly. It helps us see where and how big the herniated disc is, guiding our treatment. CT scans are used when MRI isn’t possible.
Sometimes, a CT myelogram is done. It involves dye in the spinal canal to see the spinal cord and nerves better.
Neurological tests are also key. They include EMG and NCS to check nerve function and damage. These tests help us understand how much nerve damage there is and what treatment to use.
By using physical exams, imaging, and neurological tests together, we can accurately diagnose a herniated disc. Then, we can create a treatment plan that fits your needs.
Knowing why disc herniation happens is key to stopping it and treating it well. It comes from many things that harm the spine’s health and strength.
As we get older, our spinal discs change naturally. They lose water, becoming less flexible and more likely to tear. Age-related degeneration makes discs less able to absorb shock and stay in shape.
Degenerative disc disease happens when discs wear down over time. This makes herniation more likely. It can be sped up by genes, lifestyle, and past injuries.
Big accidents, like falls or car crashes, can put a lot of stress on spinal discs. Traumatic injuries can hurt the disc right away, making it bulge or burst.
Doing the same thing over and over can also hurt discs. Repetitive lifting injuries and postural strain can weaken discs. This makes them more likely to herniate. People who work hard physically are at higher risk, showing why safety and right body mechanics are so important.
By knowing these causes, we can act early to stop disc herniation and handle its symptoms better. We can keep our spine healthy with the right exercise, posture, and lifting ways.
People with herniated discs can find relief through self-care. Simple strategies can help manage symptoms and improve life quality.
Resting your back is key when you have a herniated disc. Rest means avoiding activities that make it worse. Changing your daily activities to ease spine strain can help a lot.
For example, taking breaks when lifting or bending is good. Also, making your workspace comfortable can help your posture.
Heat and cold therapy can help with herniated disc pain. Cold packs reduce inflammation, while heat relaxes muscles and boosts blood flow.
OTC pain relievers can help with herniated disc symptoms. Ibuprofen and acetaminophen reduce pain and inflammation.
Always follow the dosage and talk to a doctor before starting any new medication.
For those with ongoing or severe herniated disc symptoms, professional help is key. Healthcare experts offer various solutions to ease pain, boost function, and improve life quality. This is vital when home remedies don’t work.
Physical therapy is essential for herniated discs. Our physical therapists create custom workout plans. These plans aim to strengthen muscles, enhance flexibility, and correct posture.
They use several techniques, such as:
Benefits of Physical Therapy:
| Therapy Type | Benefits |
| Manual Therapy | Reduces pain and inflammation, improves mobility |
| Strengthening Exercises | Enhances spinal stability, reduces risk of future injury |
| Stretching and Flexibility Exercises | Improves range of motion, reduces stiffness |
Sometimes, prescription drugs are needed to manage herniated disc symptoms. These can include:
It’s critical to consult with a healthcare provider to find the right medication and dosage.
Epidural steroid injections can offer significant relief for severe symptoms. These injections put corticosteroids near the spinal cord. This reduces inflammation and pain.
Key Considerations:
By combining these professional treatments, we can create a care plan that meets each patient’s needs.
When other treatments don’t work, surgery might be needed for herniated discs. This can be scary, but knowing what options are available is key.
Surgery is suggested for those with severe symptoms that really hurt their daily life. This includes ongoing pain, numbness, or weakness that hasn’t gotten better. Cauda Equina Syndrome is a serious condition that needs surgery right away.
Choosing surgery is a big decision. A doctor will look at your symptoms, health, and past treatments to decide.
There are many ways to fix herniated discs, each with its own reasons and benefits.
Each surgery has its own good points and risks. For example, discectomy can help a lot, but there’s a small chance of problems like infection or nerve damage. It’s important to talk about these risks with a doctor before deciding.
“The choice of surgical procedure depends on various factors, including the patient’s overall health, the location and severity of the herniation, and the surgeon’s professional judgment.” –
A spine specialist
It’s important to know about each surgery option to make a good choice. We’re here to help and support you every step of the way.
To manage and prevent herniated discs, a complete approach is needed. This includes strengthening the core, using good ergonomics, and maintaining proper body mechanics. By doing these things every day, people can lower their risk of getting herniated discs. They can also ease symptoms if they already have them.
Core exercises are key in preventing herniated discs. They make the spine stronger and more stable. A strong core spreads out the weight better, which lessens the pressure on discs. Effective core exercises include planks, bridges, and pelvic tilts. These exercises strengthen the muscles around the spine and improve posture, lowering the risk of disc herniation.
A study found that adding core exercises to your routine can greatly reduce back pain. “Regular exercise, mainly core strengthening, is essential for preventing and managing herniated discs,” say health experts.
Good body mechanics are important to avoid putting too much strain on the spine. This means lifting right, bending at the knees, and not twisting too much. Proper lifting involves bending at the knees, keeping the object close, and lifting with leg muscles, not the back.
Ergonomics is also key, but it’s more important at work. Setting up workstations for good posture can help avoid back problems. This means adjusting chair heights, monitor angles, and keyboard positions to reduce back and neck strain.
By combining core exercises with good body mechanics and ergonomic adjustments, people can take a proactive step. This helps prevent herniated discs and keeps the spine healthy in the long run.
Knowing the signs of a herniated disc is key to getting the right treatment. We’ve looked at what causes herniated discs, their symptoms, and how to treat them. This information helps you understand and manage your condition better.
Spotting symptoms like pain, numbness, and weakness is important. These signs tell you when to see a doctor. Getting the right treatment can greatly reduce back pain and improve your life.
Managing herniated discs requires a mix of self-care, professional help, and sometimes surgery. Staying active and using good body mechanics can also help. These steps can lower your risk of getting a herniated disc and keep your spine healthy for longer.
It’s vital to talk to doctors for advice on herniated discs. They can help you find the best way to manage your back pain. By being proactive and well-informed, you can better handle your condition and feel better overall.
Symptoms include pain, numbness, tingling, and muscle weakness. These can happen in the lower back, legs, neck, or arms, depending on where the disc is herniated.
The soft inner gel of the disc leaking out irritates nearby nerves. This leads to pain that can spread or stay in one place and gets worse with movement.
A herniated disc has a torn outer disc and leaking inner gel. A bulging disc has an intact outer disc but bulges outward, possibly pressing on nerves.
Yes, a herniated disc in the lower back can cause sciatica. This is pain, numbness, and tingling that goes down the sciatic nerve, affecting the lower back and legs.
Doctors use physical exams, imaging like MRI or CT scans, and nerve tests to diagnose. These help find the herniated disc and check nerve function.
Treatments include rest, heat and cold therapy, and over-the-counter pain meds. Professional options include physical therapy, prescription meds, and sometimes surgery.
Surgery is considered when other treatments don’t work. It’s also needed for severe nerve problems, cauda equina syndrome, or muscle weakness.
Some risks, like age, can’t be avoided. But, keeping your back healthy with exercises, good posture, and avoiding strain can lower the risk of herniation.
Managing chronic pain involves self-care, professional treatments, and lifestyle changes. This includes regular exercise, stress management, and ongoing medical care.
Cauda equina syndrome is a serious condition caused by nerve compression in the lower spine, often from a herniated disc. It leads to severe pain, numbness, and bladder or bowel problems, needing immediate medical help.
Yes, physical therapy is very effective. It improves mobility, strengthens the back, and reduces pain through specific exercises and manual therapies.
Disk herniation. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK441822/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!