Last Updated on November 20, 2025 by Ugurkan Demir

Find out: does anaemia cause fever? Learn about the crucial link to hemolytic anemia, jaundice, and other serious symptoms.
When anemia also brings fever and yellow eyes, it might mean there’s a bigger issue. It’s important to understand these signs to diagnose and treat the problem correctly.
We’ll look into how hemolytic anemia can show these symptoms. Knowing this helps us give the right care to our patients.
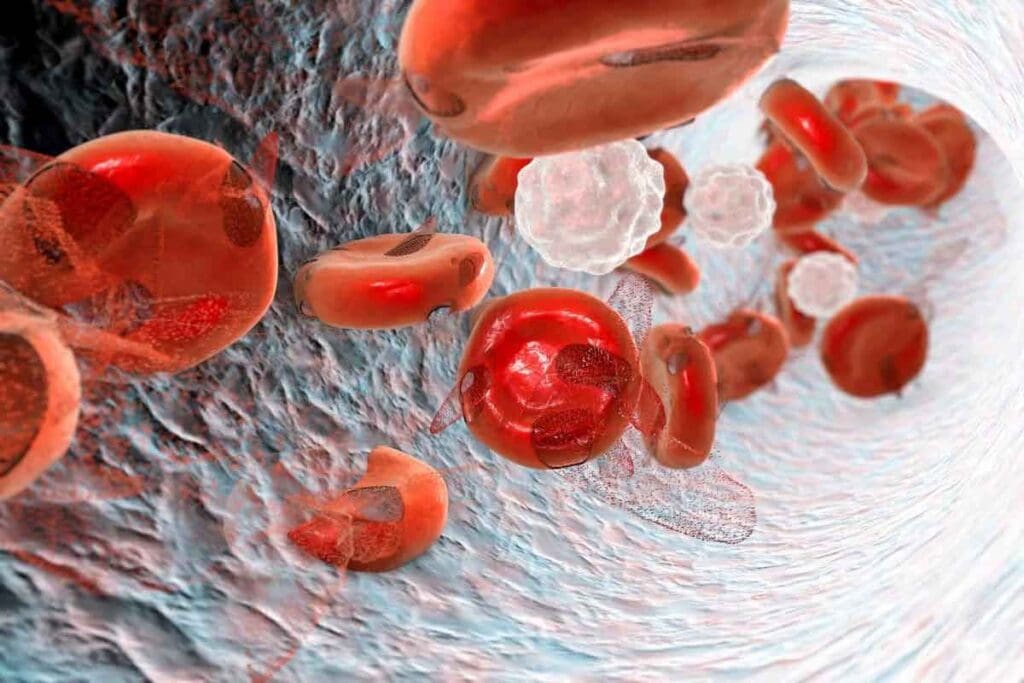
Anemia is more than just a simple condition. It has several types, including hemolytic anemia. This type is marked by the fast destruction of red blood cells. Knowing about anemia’s types and how they affect the body is key.
Anemia happens when there are not enough red blood cells or hemoglobin in the blood. Hemoglobin carries oxygen to the body’s parts. Without enough oxygen, tissues don’t get enough oxygen, causing fatigue, weakness, and shortness of breath.
Anemia affects a big part of the world’s population. It’s a major health issue that needs to be understood and managed well.
There are many types of anemia, each with its own reasons and signs. Some common ones are:
| Type of Anemia | Cause | Key Characteristics |
| Iron-deficiency anemia | Lack of iron | Low hemoglobin levels, fatigue |
| Vitamin deficiency anemia | Deficiency in vitamin B12 or folate | Neurological symptoms, weakness |
| Hemolytic anemia | Premature destruction of red blood cells | Jaundice, fatigue, shortness of breath |
Hemolytic anemia occurs when red blood cells are destroyed too quickly. This can happen inside or outside the blood, mainly in the spleen. It can be inherited or caused by other factors, like sickle cell disease.
“Hemolytic anemia represents a complex interplay of genetic, environmental, and immune system factors, requiring a nuanced approach to diagnosis and treatment.” – Hematologist.
Knowing the specific type of anemia is key to good treatment. By understanding each type’s characteristics and causes, doctors can give better care.

Hemolysis is when red blood cells break down too early. This can cause hemolytic anemia. It messes up the normal life cycle of red blood cells, leading to health problems.
Hemolysis, or erythrocyte hemolysis, is when red blood cells break down. Normally, these cells last about 120 days. But with hemolysis, they get destroyed much sooner.
This early destruction can happen for many reasons. It might be due to genetic disorders, infections, or autoimmune diseases. Knowing what hemolytic meaning is helps doctors diagnose and treat these issues.
Red blood cells are made in the bone marrow and usually last 120 days. They carry oxygen to all parts of the body.
But with hemolysis, these cells don’t last long. This can cause a lack of red blood cells, leading to anemia.
| Characteristics | Normal RBC Lifecycle | Hemolysis |
| Lifespan | Approximately 120 days | Significantly reduced |
| Destruction Location | Primarily spleen | It can occur in the spleen, liver, or bloodstream |
| Causes | Apoptosis or normal wear | Genetic, autoimmune, or infectious factors |
Erythrocyte hemolysis is when red blood cells are destroyed. The reasons can be inherited or acquired.
Inherited causes include sickle cell anemia and thalassemia. Acquired causes include autoimmune diseases, infections, and some medicines.
It’s important to know these causes and how they work. This helps doctors find the best treatments for hemolytic anemia.
Anemia and fever have a complex relationship, mainly in hemolytic anemia. This is when red blood cells break down too early. We must explore how fever happens in this condition and when it’s a worry.
Hemolytic anemia causes the body to fight off the breakdown of red blood cells. This fight releases substances like hemoglobin into the blood. The immune system sees these as invaders, leading to inflammation and fever.
This inflammation is a natural defense. But in hemolytic anemia, it can cause fever. This fever shows the body is fighting the loss of red blood cells.
Fever in hemolytic anemia, known as “hemoglobin fever,” happens when hemoglobin is released into the blood. This can start an inflammatory response, raising the body’s temperature.
The exact reasons for hemoglobin fever involve many factors. These include the release of pro-inflammatory cytokines and other substances. These changes can affect how the body regulates temperature, causing fever.
Fever can be a sign of hemolytic anemia, but knowing when it’s serious is key. A long-lasting or high fever might mean an infection or a severe crisis.
People with hemolytic anemia should watch their body temperature. If they have fever, jaundice, fatigue, or trouble breathing, they should see a doctor. It’s important to catch and treat fever early to avoid problems.
The link between jaundice and anemia comes from how our bodies deal with bilirubin. This is a byproduct of breaking down red blood cells. When red blood cells break down, as in hemolytic anemia, bilirubin levels go up. This leads to the yellow color seen in jaundice.
Jaundice is more than just a sign; it shows what’s happening inside. Knowing this helps doctors diagnose and treat hemolytic anemia better.
When red blood cells break down too much, it makes more bilirubin. Normally, the liver breaks down bilirubin and gets rid of it. But if too much is made, the liver can’t keep up.
This buildup causes the skin and eyes to turn yellow, known as jaundice. How yellow they get depends on how many red blood cells are breaking down and how well the liver can handle bilirubin.
Yes, anemia can make eyes turn yellow because of high bilirubin levels. Yellow eyes, or scleral icterus, show that bilirubin levels are too high.
Seeing yellow eyes is a key sign for doctors. It tells them to look deeper into what’s causing it, like hemolytic anemia.
Jaundice and anemia together mean there’s a problem with breaking down red blood cells. Seeing both symptoms means it’s time to really check what’s going on and how to fix it.
Spotting jaundice and anemia together is key to quick and right treatment. It needs a full check-up, tests, and sometimes more to figure out and fix the problem.
Hemolytic anemia has symptoms that can really affect a person’s life. These signs come from the fast breakdown of red blood cells and the body’s efforts to make up for it.
The symptoms of hemolytic anemia mainly come from the breakdown of red blood cells. This leads to more bilirubin, causing jaundice. Jaundice makes the skin and eyes look yellow because the liver can’t handle all the bilirubin.
Fatigue is another symptom, caused by fewer red blood cells to carry oxygen. People might also feel short of breath and have pale skin because of less oxygen getting to the tissues.
Hemolytic anemia also has symptoms that affect the whole body. Some people might get a fever. This could be because of the cause of hemolysis or the body’s fight against the red blood cell destruction.
It can also cause gallstones because of the extra bilirubin. The spleen might get bigger, too, as it tries to remove damaged red blood cells.
The symptoms of hemolytic anemia can be very different for each person. They depend on the cause, how fast red blood cells are destroyed, and how well the body can adjust. Some people might only notice mild symptoms, while others face severe fatigue, frequent jaundice, and other serious problems.
It’s important to know about all these symptoms to treat hemolytic anemia well. By understanding the range of symptoms, doctors can give better care and help patients feel better.
Red blood cells can be destroyed early, a condition known as hemolysis. This can happen due to inherited or acquired conditions. Hemolytic anemia, which leads to the early destruction of red blood cells, can greatly affect a person’s life. It’s important to know the causes to manage and treat them effectively.
Inherited conditions are a big factor in hemolytic anemia. These conditions come from genetic mutations that affect red blood cells’ structure or function.
As a medical expert says, “Genetic counseling is often recommended for families with a history of inherited hemolytic anemia. It helps them understand the risks and management options.”
Acquired hemolytic anemia comes from external or environmental factors, not genetics. These include:
Knowing if hemolytic anemia is inherited or acquired is key to finding the right treatment. As research goes on, treatments are becoming more specific to each person’s condition.
“The key to managing hemolytic anemia lies in identifying and addressing the underlying cause, whether it’s genetic or acquired.” –
Hematology Expert
Hemolytic anemia causes red blood cells to break down over time. This can lead to serious health problems. Patients often face ongoing symptoms and complications that affect their daily lives.
Chronic hemolysis causes anemia and jaundice symptoms that last forever. Patients feel tired, weak, and short of breath. The yellow skin and eyes from jaundice can also hurt their self-esteem.
Managing these symptoms is key. Regular check-ups and treatment changes are important. A full care plan helps reduce these symptoms.
Long-term hemolysis can harm organs. High bilirubin levels can cause gallstones and kidney damage. The heart also works harder, leading to heart problems.
It’s vital to watch for these problems early. This way, we can treat them quickly.
Chronic hemolysis greatly affects a patient’s life. Ongoing symptoms and organ risks limit daily activities. It also impacts mental health.
Supportive care is essential. This includes counseling and lifestyle changes. By managing symptoms and preventing complications, we help patients live better lives.
Diagnosing hemolytic anemia involves several steps. We look at clinical evaluation, lab tests, and sometimes advanced tests. This guide will help you understand how it’s done.
The first step is a detailed clinical evaluation. We check the patient’s history for signs of hemolysis, like jaundice and fatigue. A physical exam is also key, looking for signs like pallor and jaundice.
We also look at the patient’s family history. Some causes of hemolytic anemia run in families. Knowing the patient’s history helps us decide what tests to run next.
Laboratory tests are critical in diagnosing hemolytic anemia. We start with a complete blood count (CBC) to check hemoglobin and red blood cell count. A reticulocyte count shows if the bone marrow is making more red blood cells.
Other important tests include:
These tests, along with clinical findings, help confirm hemolytic anemia and find the cause.
In some cases, we need advanced tests to find the cause of hemolytic anemia. These include:
These tests help us understand the cause of hemolytic anemia. They guide us in choosing the right treatment.
Many conditions can look like hemolytic anemia. This makes differential diagnosis very important. Getting the right diagnosis is key to treating the condition properly.
It’s important to think about other health issues that might seem like hemolytic anemia. These include things that cause jaundice or fever in anemia.
Jaundice is a sign of hemolytic anemia, but it can also mean other things. For example:
To tell these apart from hemolytic anemia, we use lab tests and the doctor’s checks.
Fever can happen in people with anemia, but it’s not just from hemolytic anemia. Other reasons for fever in anemic patients include:
It’s important to do a detailed test to find out why anemic patients have a fever.
Hemophilia anemia is often mixed up with hemolytic anemia because of their similar names. But hemophilia is a problem with blood clotting, while hemolytic anemia is about red blood cells breaking down.
It’s very important to know the difference between these two conditions to treat them correctly.
Hemolytic anemia treatment focuses on the cause and severity of the condition. It aims to reduce red blood cell destruction. Management often combines strategies to address the cause, alleviate symptoms, and prevent complications.
The first step is identifying and treating the cause. This might mean stopping certain medications or treating infections. For inherited conditions like sickle cell disease, specific therapies help manage symptoms and prevent complications.
In autoimmune hemolytic anemia, immunosuppressive therapy is used to lower antibody production. We’ll explore immunosuppressive therapy further in this section.
Supportive care is key in managing hemolytic anemia. It includes:
Patients should also avoid triggers that can worsen hemolysis. This includes certain medications or extreme temperatures.
Blood transfusions are critical for some patients with severe anemia. They increase healthy red blood cells, improving oxygen delivery.
The decision to transfuse blood depends on anemia severity, symptoms, and cause. Immunosuppressive Therapy Options
Immunosuppressive therapy is used for autoimmune causes. Corticosteroids are often the first choice to reduce antibodies. Other agents may be used in resistant cases or when tapering steroids.
The choice of therapy depends on several factors. These include hemolysis severity, patient health, and medication side effects. We must carefully consider the benefits and risks of immunosuppressive therapy.
Tailoring treatment to each patient’s needs helps manage hemolytic anemia effectively. This improves their quality of life.
Living with hemolytic anemia can be tough, but the right strategies can help. It’s important to tackle both medical and lifestyle aspects. This way, people can live fulfilling lives.
Changing your lifestyle is key to managing hemolytic anemia. These changes can lessen the condition’s effects on your daily life.
Regular check-ups and follow-up care are vital for managing hemolytic anemia. They help catch problems early and adjust treatments as needed.
It’s important to see your healthcare provider regularly. This way, you can track how your condition is doing and if your treatment is working.
“Regular follow-up with a healthcare provider is essential for managing hemolytic anemia and preventing complications.”
NHS Guidelines
Stopping complications is a big part of living with hemolytic anemia. There are steps you can take to lower the risk of problems.
| Complication | Prevention Strategy |
| Infections | Keep up with vaccinations and practice good hygiene. |
| Anemia-Related Fatigue | Eat a balanced diet and think about supplements if needed. |
Dealing with hemolytic anemia can be tough emotionally. Finding support can help a lot.
We suggest looking for support groups, online or in-person. They can connect you with others facing similar issues.
By using these strategies, people with hemolytic anemia can improve their quality and manage their condition better.
Hemolytic anemia is a complex condition that needs quick recognition and treatment. We’ve looked at its causes, symptoms, and how to diagnose it. Knowing its signs, like jaundice and fever, is key.
To tackle hemolytic anemia, we must find the root cause and manage symptoms. We talked about the role of lab tests and advanced diagnostics in diagnosing it.
Healthcare providers can create effective treatment plans by understanding hemolytic anemia’s mechanisms and symptoms. It’s important for patients to get medical help if they notice symptoms like jaundice or fever.
In summary, it’s vital to recognize and treat hemolytic anemia to improve patient outcomes. Timely and proper care can lessen its impact and improve life quality for those affected.
Hemolytic anemia is when red blood cells break down too fast. This leads to a lack of red blood cells. Symptoms can include jaundice, fever, and anemia.
Yes, anemia, like hemolytic anemia, can cause fever. This happens because the body reacts to the loss of red blood cells.
When red blood cells break down, they release bilirubin. If the liver can’t clear this bilirubin fast enough, it builds up. This causes jaundice, which makes the skin and eyes yellow.
Symptoms include jaundice, fatigue, and shortness of breath. You might also have pale skin and a fever. How bad these symptoms are depends on how many red blood cells are being destroyed.
Doctors use a few ways to diagnose it. They look at your blood and bilirubin levels. They might also do a bone marrow biopsy to find the cause.
It can be caused by genes you’re born with, like sickle cell disease. Or it can be caused by things you get later, like infections or certain medicines. Autoimmune disorders can also cause it.
Treatment depends on why you have it. It might include fixing the cause, blood transfusions, and sometimes medicines to stop the red blood cells from breaking down.
Yes, with the right care, many people can manage it. This includes making lifestyle changes and getting regular check-ups.
Hemolytic anemia occurs when red blood cells break down. Hemophilia is a bleeding disorder because of a lack of clotting factors. It makes bleeding more likely.
For many, it’s a long-term condition that needs ongoing care. But how it affects you can vary based on the cause and how well you respond to treatment.
It can cause ongoing symptoms and might harm organs. But with the right care, many people can live well and enjoy their lives.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!