Last Updated on November 20, 2025 by Ugurkan Demir
Hemolytic anemia is a condition where red blood cells are destroyed too fast. This leads to symptoms like fatigue, shortness of breath, and jaundice. At Liv Hospital, we know how complex this condition can be. We provide detailed care for it.Find out: does anemia cause fever? Learn the crucial link to hemolytic anemia, jaundice, and other serious symptoms explained.
When red blood cells are destroyed quickly than they can be made, it causes jaundice anemia. This is when the skin and eyes turn yellow. This happens because of the buildup of bilirubin, a byproduct of red blood cell breakdown.
It’s important to understand the causes and effects of hemolytic anemia for effective treatment. Our team at Liv Hospital is committed to patient-centered care. We use advanced medical knowledge and an ethical approach.
When red blood cells are destroyed faster than they can be made, hemolytic anemia happens. This condition is when red blood cells are destroyed early. It can cause many health problems.
Hemolytic anemia occurs when red blood cells are destroyed too quickly. This can happen inside or outside the blood vessels, like in the spleen or liver. Medical studies show it’s a complex process involving many cellular and biochemical actions.
Symptoms of hemolytic anemia vary. They can include feeling very tired, shortness of breath, and jaundice. Jaundice makes the skin and eyes turn yellow. In severe cases, it can cause heart problems or infections.
Hemolytic anemia is different from other anemias. Unlike iron-deficiency or vitamin deficiency anemia, it’s caused by red blood cell destruction. Knowing the differences is key to correct diagnosis and treatment.
Dealing with hemolytic anemia needs a detailed approach. By understanding its causes and mechanisms, doctors can find better treatments. This helps manage symptoms and improve patient health.

Grasping hemolysis is key to understanding hemolytic anemia’s impact. Hemolysis is the breakdown of red blood cells (RBCs), leading to health issues.
When RBCs are destroyed, they spill their contents, including hemoglobin, into the blood. Hemoglobin is vital for carrying oxygen to the body’s tissues.
Erythrocyte hemolysis is the breakdown of red blood cells. The cell membrane ruptures, releasing hemoglobin into the plasma. This can happen due to autoimmune disorders, infections, or mechanical damage.
The body then processes the released hemoglobin. The liver plays a key role in handling bilirubin from hemoglobin breakdown. High bilirubin levels can cause jaundice, marked by yellow skin and eyes.
Hemoglobin is essential for RBCs to function properly. It picks up oxygen in the lungs and carries it to tissues. When RBCs are destroyed, less oxygen is delivered, causing fatigue and shortness of breath.
The loss of RBCs disrupts oxygen transport. This can lead to tissues not getting enough oxygen, causing complications.
The immediate effect of RBC destruction is the release of hemoglobin into the blood. This can cause jaundice, fatigue, and, in severe cases, kidney damage from too much hemoglobin.
The body tries to replace lost RBCs by producing new ones. But if destruction outpaces production, anemia can occur. Anemia is marked by low red blood cell count or hemoglobin levels.
Understanding hemolysis and its effects is vital for managing hemolytic anemia. Recognizing symptoms allows healthcare providers to treat them effectively.
It’s important to know how anemia and fever are connected. Fever can be a sign of different types of anemia, like hemolytic anemia. We’ll look into why this happens.
Hemoglobin fever happens when the body breaks down red blood cells. This breakdown releases hemoglobin and other stuff into the blood. It can start an inflammatory response.
This response is caused by cytokines and can make your body temperature go up. The exact reasons are complex and involve many steps.
When red blood cells break down, they release hemoglobin and other substances into the blood. This can make the body’s immune system react. It’s like the body’s way of fighting off injury or infection.
This reaction gets immune cells working and releases cytokines. These molecules help with the inflammation. This can cause fever and other symptoms.
Fever with anemia can be a sign of something serious. It might mean an infection or a big hemolytic episode. It’s key to watch the fever and get help if it doesn’t go away or gets worse.
Knowing when fever is a big deal is important. The table below shows when to worry:
| Symptom | Possible Indication | Action Required |
| Fever above 101°F (38.3°C) | Possible infection or severe hemolysis | Seek immediate medical attention |
| Fever accompanied by chills or sweating | Infection or significant inflammatory response | Consult a healthcare provider |
| Fever with severe anemia symptoms | Significant hemolytic episode | Urgent medical evaluation |
Knowing how anemia and fever are linked helps people see when they need more medical help.
Jaundice and anemia are linked through hemolysis, where red blood cells break down faster. This leads to jaundice, a yellowish skin and eye discoloration. Understanding hemolysis and its effect on bilirubin levels is key.
When red blood cells are destroyed, hemoglobin is released into the blood. This hemoglobin turns into bilirubin, a yellow pigment. As more red blood cells are broken down, more bilirubin is produced. This results in elevated bilirubin levels.
The liver is vital in handling bilirubin from broken-down red blood cells. It makes bilirubin water-soluble so it can be excreted. But if hemolysis is too fast, the liver can’t keep up. This leads to high levels of unconjugated bilirubin in the blood.
Jaundice happens in hemolytic anemia because the liver can’t handle all the bilirubin. This causes bilirubin to build up, turning the skin and eyes yellow. It shows the body’s fight against the fast breakdown of red blood cells.
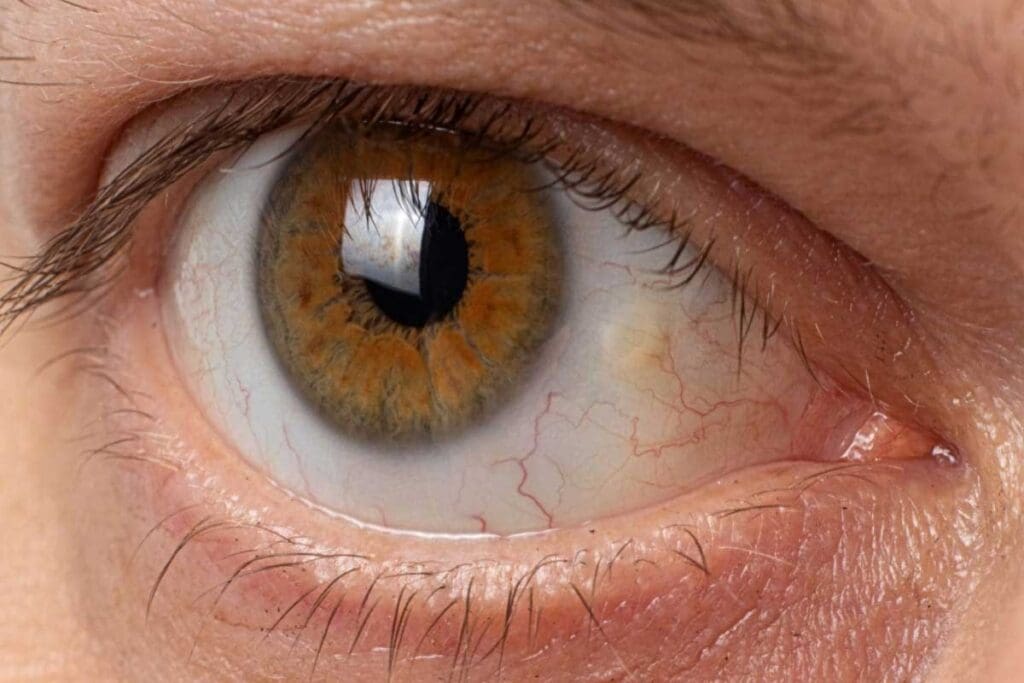
The yellowing of the eyes, known as scleral icterus, is a key sign of hemolytic anemia. It happens when the body breaks down red blood cells too fast. The liver can’t keep up, leading to a buildup of bilirubin.
Scleral icterus makes the white part of the eye turn yellow. This is because bilirubin loves to stick to the elastic tissues in the sclera. Seeing yellow eyes can be an early sign of hemolytic anemia.
In severe cases, the yellowing of the eyes can be very noticeable. This is often seen with jaundice, feeling tired, and shortness of breath. If you notice yellow eyes, it’s important to see a doctor right away.
People with hemolytic anemia might also see their skin and mucous membranes look pale. In some cases, the retina can change due to anemia or related issues.
| Visual Symptom | Description | Association with Hemolytic Anemia |
| Scleral Icterus | Yellowing of the whites of the eyes | Directly related to bilirubin buildup from hemolysis |
| Pallor | Pale skin and mucous membranes | Result of reduced red blood cell count |
| Retinal Changes | Alterations in the retina | May occur in association with anemia or related conditions |
Inherited hemolytic anemia is a group of disorders in which red blood cells are destroyed early. This happens because of genetic mutations. These conditions are passed down from parents to their children and can greatly affect their lives if not managed well.
We will look at three main inherited hemolytic anemia types: Sickle Cell Anemia, Thalassemia, and Enzyme Deficiencies Leading to Hemolytic Anemia. Knowing about these conditions is key to early diagnosis and treatment.
Sickle Cell Anemia is a genetic disorder that affects hemoglobin in red blood cells. It makes red blood cells sickle-shaped, leading to their early destruction. This shape can cause them to get stuck in small blood vessels, making the condition worse.
Key complications of Sickle Cell Anemia include:
Thalassemia is another inherited hemolytic anemia caused by mutations in genes responsible for hemoglobin production. It results in reduced or absent globin chains, leading to anemia and other issues.
There are two main types of Thalassemia: Alpha-Thalassemia and Beta-Thalassemia. Each type has different levels of severity based on the number of genes affected.
Certain enzyme deficiencies, like Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency, can cause hemolytic anemia. G6PD deficiency makes red blood cells more likely to be destroyed under certain conditions, such as infection or specific medications.
Understanding the triggers and managing these conditions properly can greatly improve life quality for those with enzyme deficiency-related hemolytic anemia.
Acquired hemolytic anemia comes from many factors that destroy red blood cells too much. It’s different from inherited forms because it happens over a person’s life. It’s caused by things outside the body or secondary to other conditions.
Autoimmune hemolytic anemia (AIHA) happens when the immune system sees red blood cells as enemies. It attacks them. This can be because of other diseases like lupus or infections. Treatments often involve immunosuppressive drugs to dampen the immune system’s attack on red blood cells.
Some medicines can make red blood cells break down. This happens when the immune system reacts to the cells or when the cells get damaged. Common offenders include antibiotics like penicillin and anti-inflammatory drugs. Stopping the offending medication is usually the first step in managing this condition.
Infections can lead to hemolytic anemia in several ways. They can directly harm red blood cells or release toxins that damage them. Malaria is a well-known example where parasites infect and destroy red blood cells.
Red blood cells can get damaged by artificial heart valves or vascular grafts. These devices can cause red blood cells to break as they pass through. It’s key to watch patients with these devices for signs of hemolysis.
Knowing about these causes of hemolytic anemia is key to treatment. Each cause needs a different plan, from changing medicines to treating infections or autoimmune diseases.
To find out if someone has hemolytic anemia, doctors use several important tools. They look at blood tests to see how bad the anemia is and what might be causing it.
Blood tests are key in spotting hemolytic anemia. Here are some important ones:
The reticulocyte count is very important for diagnosing hemolytic anemia. Reticulocytes are young red blood cells. If there are more of them, it means the bone marrow is making more red blood cells because of hemolysis. This test shows how severe the anemia is and how well the bone marrow is responding.
The Direct Antiglobulin Test (DAT), or Coombs test, finds antibodies or proteins attached to red blood cells. These can mark red blood cells for destruction, causing hemolytic anemia. The DAT is key for diagnosing autoimmune hemolytic anemia.
Other ways to diagnose hemolytic anemia include:
Treating hemolytic anemia involves several steps. It depends on the cause of the condition. We need to find and fix the root problem, using different treatments.
First, we tackle the main cause of hemolytic anemia. For infections, we use antibiotics. For autoimmune issues, immunosuppressive therapies help stop the immune system from attacking red blood cells.
Corticosteroids are often the first choice to calm down the immune system. Studies show they work well for autoimmune hemolytic anemia (PMC9821124).
Immunosuppressive treatments are key for autoimmune hemolytic anemia. They reduce the immune system’s attack on red blood cells. These treatments include:
Supportive treatments help manage hemolytic anemia symptoms. They improve the quality of life. These include:
In serious cases, blood transfusions are needed. They quickly boost oxygen to tissues. We consider transfusions when hemoglobin levels get too low, risking the patient’s health.
By customizing treatment and watching how the patient responds, we can manage hemolytic anemia well. This improves patient outcomes.
Managing chronic hemolysis needs a full plan. Patients must prevent episodes, watch for complications, and keep their quality of life good.
Managing chronic hemolysis means using medicine and changing lifestyle. Medications like corticosteroids and immunosuppressants help. Sometimes, splenectomy is needed.
Patients need to work with their doctors. They need a treatment plan that fits them. Regular check-ups help adjust treatments and watch for problems.
Stopping hemolytic episodes is key. Avoiding certain medicines or foods helps. Eating well and drinking plenty of water is also important.
Knowing the signs of an episode is vital. Look out for jaundice, fatigue, and shortness of breath. If you see these, get help fast.
Checking for complications regularly is important. Blood tests for anemia and jaundice should be done often. Watch for signs of organ damage too.
| Complication | Monitoring Method | Frequency |
| Anemia | Blood tests (CBC) | Every 3-6 months |
| Jaundice | Bilirubin levels | Every 6-12 months |
| Organ Damage | Imaging studies (e.g., ultrasound) | Annually |
Chronic hemolysis can really affect your life. Fatigue and jaundice can make everyday tasks hard.
To feel better, try supportive care. This includes counseling, nutrition advice, and learning to manage your condition. Joining support groups can also help a lot.
We’ve looked into hemolytic anemia, a condition where red blood cells break down too early. This detailed look has shown us the different reasons, signs, and ways to diagnose it.
Hemolytic anemia is a complex issue that needs a full care plan. Knowing how it works, like the breakdown of red blood cells and jaundice, is key to managing it well.
By spotting the signs of hemolytic anemia early, people can get help fast. This leads to quick diagnosis and treatment. We’ve talked about how a team effort is best for treating this condition, using many approaches to fix the root problems and ease symptoms.
In short, understanding hemolytic anemia fully is essential for the best care. We hope this detailed look has given you useful knowledge. It should help you take a more active part in your health care.
Hemolytic anemia happens when red blood cells break down too fast. This leads to symptoms like tiredness, short breath, and jaundice.
Unlike other anemias, like iron-deficiency anemia, hemolytic anemia is about red blood cells breaking down. It’s not about not making enough.
Yes, fever can be a sign of hemolytic anemia. It’s important to know when to worry about fever with anemia.
Jaundice often shows up in hemolytic anemia. It happens when the liver can’t handle the extra bilirubin from broken-down red blood cells.
Yellow eyes, or scleral icterus, can be a sign of hemolytic anemia. It means there’s a lot of bilirubin from broken-down red blood cells.
Inherited forms include sickle cell anemia and thalassemia. These genetic mutations cause hemolytic anemia.
Acquired causes include autoimmune hemolytic anemia, hemolysis from medicines, and infection-related hemolytic anemia.
Doctors use blood tests like the Direct Antiglobulin Test (DAT) and reticulocyte count. These tests check how fast red blood cells are being destroyed.
Treatment depends on the cause. It might include medicines to stop the immune system from attacking red blood cells, blood transfusions, and treatments to help manage symptoms.
Managing chronic hemolysis means preventing episodes, watching for complications, and focusing on quality of life. Long-term strategies are key.
Erythrocyte hemolysis is when red blood cells are destroyed. It can cause symptoms like jaundice and fatigue.
Hemoglobin is vital for red blood cells. It carries oxygen. When it’s released during hemolysis, it can cause symptoms.
Medical News Today. (2015). Hemolytic anemia: Causes, symptoms and diagnosis. Retrieved from https://www.medicalnewstoday.com/articles/237462
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!