
At Liv Hospital, we know how hard it is to diagnose aplastic anemia. It’s a rare but serious condition where the bone marrow doesn’t make enough blood cells. This results in pancytopenia, which means fewer red blood cells, white blood cells, and platelets.Learn 7 key aplastic anemia blood test results and laboratory findings you should know. Understand the serious implications.
It’s important to understand the lab findings for this condition. We offer full care for aplastic anemia patients. We use blood tests to find key signs. These signs often show pancytopenia on a complete blood count (CBC) and other important signs.
Key Takeaways
- Pancytopenia is a key sign of aplastic anemia.
- A complete blood count (CBC) is key to checking blood cell production.
- The reticulocyte count helps check bone marrow work.
- Lab results help decide on treatment.
- Comprehensive care tackles related health issues.
- Getting the right diagnosis is key to good treatment.
What Is Aplastic Anemia and Why Blood Tests Matter
Aplastic anemia is a serious condition that affects how the bone marrow makes blood cells. It’s important to understand its definition, how it works, and the role of blood tests in diagnosing it. This condition makes it hard for the bone marrow to produce blood cells.
Definition and Pathophysiology of Aplastic Anemia
Aplastic anemia happens when hematopoietic stem cells in the bone marrow fail. This leads to a big drop in blood cell production. It affects red blood cells, white blood cells, and platelets.
This condition is caused by the immune system attacking the bone marrow. It can be triggered by toxins, certain medicines, viruses, and autoimmune diseases.
The Critical Role of Laboratory Testing
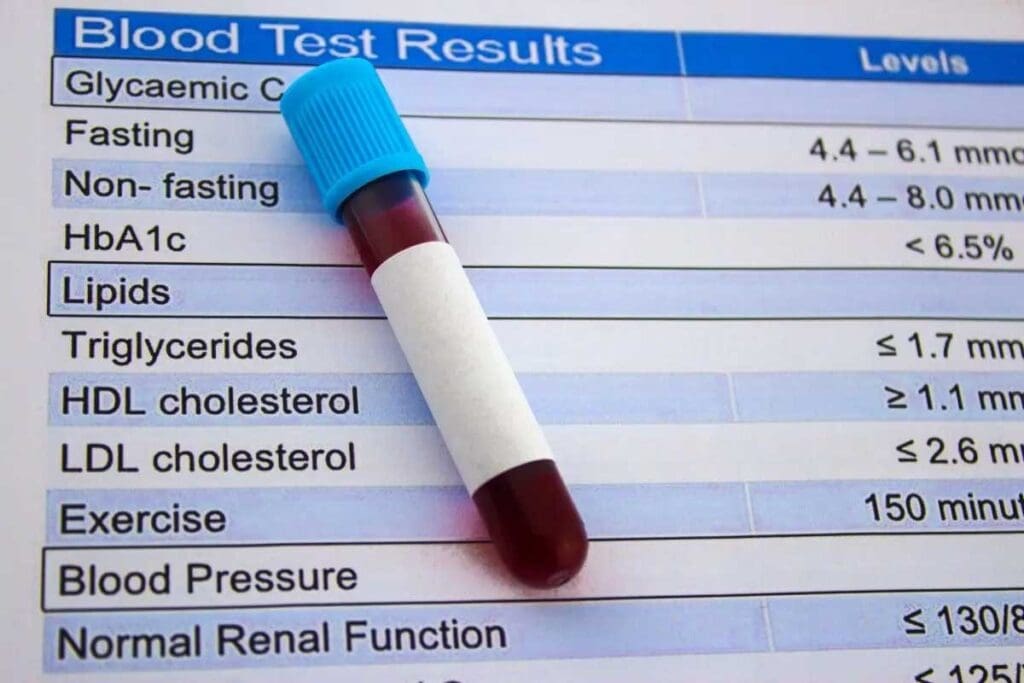
Laboratory tests are key in diagnosing aplastic anemia. The first step is a Complete Blood Count (CBC). It shows if there’s a lack of blood cells.
More tests, like bone marrow aspiration and biopsy, are needed. They help confirm the diagnosis and see how severe it is.
| Laboratory Test | Purpose |
| Complete Blood Count (CBC) | To identify pancytopenia and assess the severity of blood cell reduction. |
| Bone Marrow Aspiration and Biopsy | To evaluate the bone marrow’s cellularity and confirm the diagnosis of aplastic anemia. |
| Reticulocyte Count | To assess the bone marrow’s ability to produce new red blood cells. |
These tests are vital for diagnosing aplastic anemia. They help figure out how severe it is and guide treatment.
Overview of Aplastic Anemia Blood Test Results
Diagnosing aplastic anemia requires a detailed look at blood test results. We will discuss the steps and tests involved in this process.
The Diagnostic Approach to Suspected Aplastic Anemia
When we think aplastic anemia might be present, we follow a specific plan. First, we run a Complete Blood Count (CBC). Then, we do more detailed tests, like a bone marrow biopsy.
“The diagnosis of aplastic anemia is based on a combination of clinical findings and laboratory tests.” – A statement that highlights the need for a detailed approach.
The CBC is our first step. It often shows pancytopenia. Then, we do more tests to confirm the diagnosis.
Primary vs. Secondary Laboratory Investigations
Primary tests include the CBC and reticulocyte count. These tests give us our first hints about aplastic anemia.
| Laboratory Test | Purpose |
| CBC | To assess the overall blood cell count |
| Reticulocyte Count | To evaluate bone marrow function |
Secondary tests are more detailed, like the bone marrow biopsy. This test is key to confirming the diagnosis by showing hypocellularity.
Our method is thorough, making sure we look at every part of the patient’s condition.
Key Finding #1: Pancytopenia on Complete Blood Count
Pancytopenia is when all three types of blood cells – red, white, and platelets – drop. This is a key sign of aplastic anemia. It shows the bone marrow can’t make enough blood cells.
Understanding CBC Parameters in Aplastic Anemia
A Complete Blood Count (CBC) is vital for checking blood cell levels. In aplastic anemia, CBCs show a drop in all blood cell types. Knowing these CBC details is key to diagnosing aplastic anemia. A CBC looks at:
- Hemoglobin (Hb) and Hematocrit (Hct) for red blood cells
- White Blood Cell Count (WBC) for white blood cells
- Platelet Count for platelets
These parts of the CBC tell us how bad the pancytopenia is. They show how much the bone marrow is failing.
The Significance of Simultaneous Decrease in All Blood Cell Lines
A drop in all blood cell lines points to a bone marrow problem. This pancytopenia is not just one cell line issue; it’s a full failure of the bone marrow. The level of pancytopenia can vary. But its presence is a big clue that needs more checking, like for aplastic anemia.
By looking at CBC results and understanding pancytopenia, we move closer to diagnosing aplastic anemia. This is a big step towards starting the right treatment.
Key Finding #2: Decreased Red Blood Cell Parameters
Aplastic anemia shows a decrease in red blood cell parameters. This reflects the condition’s impact on bone marrow. We will explore how aplastic anemia affects red blood cell production and the key lab findings.
Hemoglobin and Hematocrit Values in Aplastic Anemia
In aplastic anemia, hemoglobin (Hb) and hematocrit (Hct) values are typically decreased. Hemoglobin is a protein in red blood cells that carries oxygen. Hematocrit is the proportion of red blood cells in the blood. A decrease in these values indicates anemia, a common feature of aplastic anemia.
Anemia’s severity can vary. It often depends on the degree of bone marrow failure. We see that:
- Low hemoglobin levels can lead to symptoms such as fatigue, weakness, and shortness of breath.
- Hematocrit values provide insight into the proportion of red blood cells, helping to assess the severity of anemia.
Morphological Features of RBCs
While aplastic anemia mainly affects red blood cell production, the morphological features of RBCs are also important. Typically, the red blood cells in aplastic anemia are normocytic and normochromic, meaning they are of normal size and hemoglobin content.
Some variations may be observed, and understanding these can help in differential diagnosis. Key points to note include:
- The presence of normocytic, normochromic anemia is consistent with the diagnosis of aplastic anemia.
- Occasionally, macrocytosis (larger than normal red blood cells) may be seen if there is an associated folate or vitamin B12 deficiency.
In summary, decreased red blood cell parameters, including low hemoglobin and hematocrit values, are critical findings in aplastic anemia. Understanding these changes, along with the morphological features of RBCs, is essential for diagnosing and managing the condition effectively.
Key Finding #3: Low White Blood Cell Count
One key finding in aplastic anemia is a low white blood cell count. White blood cells help fight infections. In aplastic anemia, the bone marrow can’t make enough blood cells. This makes patients more likely to get sick.
Neutropenia: The Most Significant WBC Finding
Neutropenia, or a low neutrophil count, is a big problem in aplastic anemia. Neutrophils fight bacterial infections. Without enough neutrophils, the body can’t fight off infections well. This puts patients at risk for serious infections.
Absolute Neutrophil Count Calculation and Interpretation
The Absolute Neutrophil Count (ANC) is very important. It shows how many neutrophils are in the blood. To find ANC, we multiply the white blood cell count by the percentage of neutrophils. A low ANC means a higher risk of getting sick.
Here’s how to understand ANC:
| ANC Value | Interpretation |
| > 1,500 cells/µL | Normal |
| 1,000-1,500 cells/µL | Mild neutropenia |
| 500-1,000 cells/µL | Moderate neutropenia |
| Severe neutropenia |
Knowing about ANC is key to managing aplastic anemia. It helps decide how to protect against infections. It also tells if G-CSF therapy is needed to help make more neutrophils.
Key Finding #4: Reduced Platelet Count
Thrombocytopenia, or low platelet count, is common in aplastic anemia. It raises the risk of bleeding, making it key to managing the disease.
Typical Platelet Values in Aplastic Anemia
In aplastic anemia, the bone marrow fails, leading to low platelet counts. Normal counts are 150,000 to 450,000 platelets per microliter. But aplastic anemia patients often have counts below 50,000/μL, sometimes even below 20,000/μL.
The severity of thrombocytopenia varies among patients. But it’s a common finding in all stages of the disease. Below is a comparison of platelet counts in aplastic anemia patients and normal values.
| Category | Normal Range | Aplastic Anemia |
| Platelet Count (/μL) | 150,000 – 450,000 | Often |
Correlation Between Platelet Count and Bleeding Risk
The risk of bleeding in aplastic anemia patients is tied to their platelet count. As platelet counts drop, so does the risk of bleeding. Severe thrombocytopenia (low platelet count) increases this risk.
But, he link between platelet count and bleeding risk isn’t straightforward. Other factors, like platelet function and coagulation disorders, also play a role. Yet, keeping platelet counts up is vital in managing aplastic anemia.
In summary, a low platelet count is a big deal in aplastic anemia, raising the risk of bleeding. Knowing the usual platelet values and how they relate to bleeding risk is key to managing the disease well.
Key Finding #5: Characteristically Low Reticulocyte Count
Reticulocytopenia, or a low reticulocyte count, is a key sign of aplastic anemia. It shows that the bone marrow can’t make new blood cells. This finding is important for diagnosing the condition and telling it apart from other blood disorders.
To grasp the importance of reticulocytopenia in diagnosing aplastic anemia, we must look at the details of reticulocyte counts and what they mean.
Understanding Reticulocyte Percentage and Absolute Count
Reticulocytes are young red blood cells in the blood. The reticulocyte count shows how many of these cells are in the blood. It’s usually given as a percentage or an absolute number.
- Reticulocyte Percentage: This shows the percentage of red blood cells that are reticulocytes, usually between 0.5% and 2% in healthy people.
- Absolute Reticulocyte Count: This gives the exact number of reticulocytes per microliter of blood. It’s a better way to see how active the bone marrow is.
In aplastic anemia, both the percentage and absolute count of reticulocytes are low. This means the bone marrow isn’t making enough red blood cells.
Why Reticulocytopenia Differentiates Aplastic Anemia
Reticulocytopenia is a key sign that sets aplastic anemia apart from other blood disorders. A low reticulocyte count means the bone marrow isn’t making enough new blood cells. This is a key feature of aplastic anemia.
Other blood disorders, like myelodysplastic syndromes or leukemia, might have different reticulocyte counts. Knowing the reticulocyte count helps doctors tell these conditions apart. It guides them to do more tests to find the right diagnosis.
Doctors look at the reticulocyte count along with other lab results to make a correct diagnosis. This helps them plan the best treatment for patients with suspected aplastic anemia.
Key Finding #6: Bone Marrow Hypocellularity
Diagnosing aplastic anemia requires a detailed look at the bone marrow. We’ll explore how bone marrow aspiration and biopsy results help in making this diagnosis.
Bone Marrow Aspiration and Biopsy Results
Bone marrow biopsy is key in diagnosing aplastic anemia. It involves checking the bone marrow tissue for cell count. In aplastic anemia, the bone marrow is hypocellular, meaning it has fewer cells than usual.
Quantifying Cellularity and Fatty Replacement
The bone marrow’s cell count is measured by comparing hematopoietic cells to fatty tissue. In aplastic anemia, there’s a drop in hematopoietic cells and an increase in fatty tissue. A study on Haematologica shows this change is a key diagnostic sign.
By looking at the bone marrow, doctors can confirm aplastic anemia and rule out other conditions with similar symptoms.
Key Finding #7: Normal Biochemical Parameters
Normal biochemical parameters are a key finding in aplastic anemia. They help tell it apart from other disorders. While blood tests are key for diagnosing aplastic anemia, these parameters offer more insight for managing the patient.
Liver and Kidney Function Tests
Liver and kidney function tests are usually normal in aplastic anemia patients. This is important because it helps rule out other causes of low blood cells. Liver function tests, including ALT, AST, and bilirubin levels, are usually normal, showing the liver is okay. Also, kidney function tests, such as serum creatinine and urea, are usually normal, showing the kidneys are working well.
Serum Iron Studies and Vitamin Levels
Serum iron studies and vitamin levels offer more insights into the patient’s health. In aplastic anemia, serum iron levels may be elevated because of less iron use and blood transfusions. This is important for managing iron levels in patients. Vitamin levels, like vitamin B12 and folate, are usually normal, helping to rule out other anemias.
Understanding these biochemical parameters is key to managing aplastic anemia patients. They may not diagnose the condition, but they help paint a full picture of the patient’s health. This guides treatment decisions.
Diagnostic Criteria for Confirming Aplastic Anemia
To confirm aplastic anemia, we need to understand its diagnostic criteria. The diagnosis involves clinical findings, blood counts, and bone marrow tests.
The International Agranulocytosis and Aplastic Anemia Study says aplastic anemia is diagnosed when certain blood criteria are met. These include a low neutrophil count, low platelet count, and low reticulocyte count. A hypocellular bone marrow is also required.
International Standards for Diagnosis
International standards guide the diagnosis of aplastic anemia. They help distinguish it from other bone marrow failure syndromes. These standards focus on:
- Bone marrow hypocellularity on biopsy
- Peripheral blood cytopenias
- The absence of significant dysplasia or abnormal infiltrates
Marsh et al. (2003) note, “The diagnosis of aplastic anemia is one of exclusion. It requires careful evaluation to rule out other causes of bone marrow failure.”
Severity Classification Based on Blood Counts
The severity of aplastic anemia is based on blood counts. The Camitta criteria are used to classify it. They categorize it as severe or very severe based on the neutrophil count and other factors.
| Severity | Neutrophil Count | Other Criteria |
| Severe Aplastic Anemia | < 0.5 x 10/L | At least two of the following: platelet count < 20 x 10/L, reticulocyte count < 40 x 10/L, or anemia |
| Very Severe Aplastic Anemia | < 0.2 x 10/L | Meets criteria for severe aplastic anemia |
Knowing these diagnostic criteria and severity classifications is key to managing aplastic anemia well.
Differentiating Aplastic Anemia from Other Causes of Pancytopenia
When pancytopenia is found, it’s important to determine if it’s aplastic anemia or something else, like myelodysplastic syndromes or leukemia. Pancytopenia means low counts of red, white blood cells, and platelets. It can be caused by many bone marrow problems. Getting the right diagnosis is key to the right treatment.
Myelodysplastic Syndromes vs. Aplastic Anemia
Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. Both MDS and aplastic anemia can cause pancytopenia. But they are different. MDS has a normal or too many cells in the bone marrow, unlike aplastic anemia, which has too few cells. Also, MDS shows changes in blood cells that aplastic anemia doesn’t.
Key distinguishing features:
- Bone marrow cellularity: Hypocellular in aplastic anemia vs. normocellular or hypercellular in MDS
- Presence of dysplastic cells: Typically absent in aplastic anemia, present in MDS
- Cytogenetic abnormalities: More common in MDS
Leukemia and Lymphoma vs. Aplastic Anemia
Leukemia and lymphoma can also cause pancytopenia by filling the bone marrow. In leukemia, the bone marrow is full of cancer cells. Lymphoma in the bone marrow also leads to pancytopenia. These conditions have specific signs, like certain cell shapes or genetic changes, that aplastic anemia doesn’t have.
Key distinguishing features:
- Presence of blasts or abnormal lymphocytes in the peripheral blood or bone marrow
- Specific immunophenotypic or cytogenetic markers
- Bone marrow biopsy findings, such as infiltration by lymphoma cells
Other Conditions with Similar Laboratory Profiles
Other conditions, like megaloblastic anemia, paroxysmal nocturnal hemoglobinuria (PNH), and systemic lupus erythematosus (SLE), can also show pancytopenia. Each has its own signs that help tell it apart from aplastic anemia.
Diagnostic considerations:
- Megaloblastic anemia: Characterized by macrocytic anemia and specific findings on bone marrow examination
- PNH: Diagnosed by flow cytometry, showing deficiency of GPI-linked proteins on blood cells
- SLE: Presence of specific autoantibodies and clinical criteria for systemic lupus
To tell if it’s aplastic anemia or something else, doctors need to look closely at the bone marrow, do tests, and analyze cells. Knowing the differences helps doctors give the right treatment.
Conclusion: Understanding Your Aplastic Anemia Test Results
It’s key for patients and doctors to get the lab results right for aplastic anemia. At Liv Hospital, we make sure you understand your aplastic anemia test results. This helps us give you the best care.
The 7 key lab findings we talked about are vital for diagnosing and managing aplastic anemia. Knowing these helps patients understand their condition better. It also shows them what steps to take for treatment.
We aim to provide top-notch healthcare, including support for international patients. Our team is here to help you understand your aplastic anemia diagnosis. We’ll guide you through the treatment process every step of the way.
FAQ
What are the typical blood test results for aplastic anemia?
Blood tests for aplastic anemia show a drop in all blood cell types. This includes red blood cells, white blood cells, and platelets.
What is pancytopenia, and how is it related to aplastic anemia?
Pancytopenia means a drop in all blood cell types. It’s a key sign of aplastic anemia. It shows the bone marrow can’t make enough blood cells.
How is aplastic anemia diagnosed using laboratory tests?
To diagnose aplastic anemia, doctors start with a Complete Blood Count (CBC). Then, they do a bone marrow biopsy. These tests help figure out if it’s aplastic anemia.
What are the key findings on a CBC in aplastic anemia?
A CBC for aplastic anemia shows low red blood cells, white blood cells, and platelets. This is because the bone marrow isn’t making enough.
What is the significance of a low reticulocyte count in aplastic anemia?
A low reticulocyte count is a big clue for aplastic anemia. It shows the bone marrow can’t make new red blood cells.
How does a bone marrow biopsy help in diagnosing aplastic anemia?
A bone marrow biopsy is key to diagnosing aplastic anemia. It shows the bone marrow isn’t full of cells. This is a big sign of the condition.
Are biochemical parameters such as liver and kidney function tests affected in aplastic anemia?
Usually, liver and kidney tests are normal in aplastic anemia. But doctors might check iron and vitamin levels to rule out other problems.
How is the severity of aplastic anemia classified?
The severity of aplastic anemia is based on blood counts. Doctors look at how low the counts are and the number of neutrophils. International standards help with this.
How is aplastic anemia differentiated from other causes of pancytopenia?
Aplastic anemia is different from other pancytopenia causes by specific tests. Doctors look at bone marrow biopsy results and blood cell shapes.
What is the role of reticulocyte count in differentiating aplastic anemia?
The reticulocyte count is very important in telling aplastic anemia apart from other causes. A low count means the bone marrow can’t make new red blood cells.
References:
- For detailed guidelines on creating high-quality hospital websites and evidence-based online healthcare content, see this thorough review on hospital website quality criteria:https://pmc.ncbi.nlm.nih.gov/articles/PMC5410906/
































