Last Updated on November 20, 2025 by Ugurkan Demir

At Liv Hospital, we know how scary a diagnosis of aplastic anemia can be. Many wonder, “Is aplastic anemia cancer?” We’re here to tell you that aplastic anemia is not cancer. It’s a serious condition where the bone marrow can’t make enough blood cells. Is aplastic anemia cancer? Learn how a aplastic anemia bone marrow transplant treats this serious disorder and the powerful difference between the two.
Even though aplastic anemia isn’t cancer, it can raise the risk of some cancers. Our team is ready to offer top-notch care and treatments. This includes bone marrow transplantation to help our patients get better.
Aplastic anemia is a rare and serious condition where the bone marrow fails to make blood cells. This failure means the bone marrow can’t produce enough red blood cells, white blood cells, and platelets. This leads to pancytopenia.
Aplastic anemia happens when the bone marrow can’t make blood cells. Normally, the bone marrow turns stem cells into different blood cells. But in aplastic anemia, this process stops, causing a lack of blood cells.
The exact reason for this failure is often linked to the immune system attacking the bone marrow’s stem cells. But the exact how and why can vary.
This failure to make blood cells can cause many problems. These include anemia, infections, and bleeding issues. Knowing why it happens is key to finding good treatments.
Aplastic anemia can be caused by many things. Some causes are unknown, while others are linked to genetics or environmental factors. Certain drugs and viruses can also cause it.
Finding out what caused it is important for treatment. Some cases have clear causes, while others don’t. This means a detailed treatment plan is needed.
Patients with aplastic anemia face many symptoms. These include tiredness, infections, bruising, and bleeding. Knowing these symptoms and how doctors diagnose them is key for early treatment.
Aplastic anemia shows through many symptoms. This is because of pancytopenia, a low count of red, white blood cells, and platelets. Symptoms include:
These symptoms can really affect a patient’s life. They need quick medical help.
To diagnose aplastic anemia, doctors use several tests. These tests check for the condition and rule out other causes. Important tests include:
The bone marrow biopsy is very important. It lets doctors see if the bone marrow can make blood cells.
Early diagnosis is critical. It helps start the right treatment and improve patient outcomes.
Aplastic anemia is often thought of as cancer, but it’s not the same. We need to know what makes cancer and how aplastic anemia is different.
Cancer is when cells grow and spread out of control. It can harm nearby tissues and organs. It can also move to other parts of the body through the blood or lymph system.
The main signs of cancer include cells that keep growing, ignore growth stoppers, and don’t die when they should.
“Cancer is a complex disease involving genetic and environmental factors, leading to the uncontrolled proliferation of cells.”
Nobel Prize in Physiology or Medicine, 2018
Aplastic anemia is when the bone marrow can’t make enough blood cells. This isn’t because of too many cells growing. It’s because the bone marrow isn’t working right.
The main difference is that cancer has too many cells, while aplastic anemia has too few. This shows that aplastic anemia is not cancer.
| Characteristics | Cancer | Aplastic Anemia |
| Cell Growth | Uncontrolled cell proliferation | Failure of bone marrow to produce cells |
| Primary Issue | Excessive cell growth | Insufficient cell production |
| Impact on Body | Invasion and damage to tissues and organs | Reduced ability to produce blood cells, leading to anemia, infections, and bleeding |
Even though aplastic anemia is not cancer, people with it might be at higher risk for some cancers. But, it’s not called cancer because of its different cause and effects.
In conclusion, knowing the difference between aplastic anemia and cancer is key for correct diagnosis and treatment. Both affect the body’s function, but they have different causes and effects.
The link between aplastic anemia and cancer is complex. It involves many factors that can lead to secondary malignancies. People with aplastic anemia might face a higher risk of some cancers. This is true, mainly after they’ve had certain treatments or bone marrow transplants.
Research shows that aplastic anemia patients are more likely to get secondary cancers. A study on PubMed found a significant number of cancers in these patients. This is more common in those who have had specific treatments.
The most common cancers include:
Several factors can raise the risk of cancer in aplastic anemia patients. These include:
Knowing these factors is key to managing the risk of secondary cancers. We’ll look at the data in more detail below.
| Risk Factor | Description | Impact on Cancer Risk |
| Immunosuppressive Therapy | Treatment that suppresses the immune system | Increases risk of secondary malignancies |
| Bone Marrow Transplantation | Procedure to replace damaged bone marrow | May increase risk due to conditioning regimens |
| Genetic Predisposition | Inherited genetic factors | May predispose to certain cancers |
Treatment for aplastic anemia has changed a lot. Now, we use many ways to help the bone marrow work right again. Our goal is to ease symptoms, help the bone marrow heal, and make patients feel better.
Supportive care is key in treating aplastic anemia. It helps manage symptoms and avoid serious problems. This includes:
These steps improve patients’ lives and lower the chance of serious issues.
Immunosuppressive therapy is a main treatment for aplastic anemia. It’s for those who can’t get a bone marrow transplant. This therapy uses medicines to calm down the immune system. It helps the bone marrow work better.
| Therapy Type | Medications Used | Benefits |
| Immunosuppressive Therapy | Antithymocyte globulin (ATG), Cyclosporine | Restores bone marrow function, improves blood cell counts |
Growth factors are also a big part of treating aplastic anemia. Growth factors, like granulocyte-colony stimulating factor (G-CSF), help the bone marrow make more blood cells. This lowers the risk of infections and other problems.
In summary, treating aplastic anemia involves supportive care, immunosuppressive therapy, and growth factors. Knowing these treatments helps patients and doctors choose the best plan.
Hematopoietic stem cell transplantation is a key treatment for aplastic anemia. It can greatly improve a patient’s life. A bone marrow transplant is a chance for a new start.
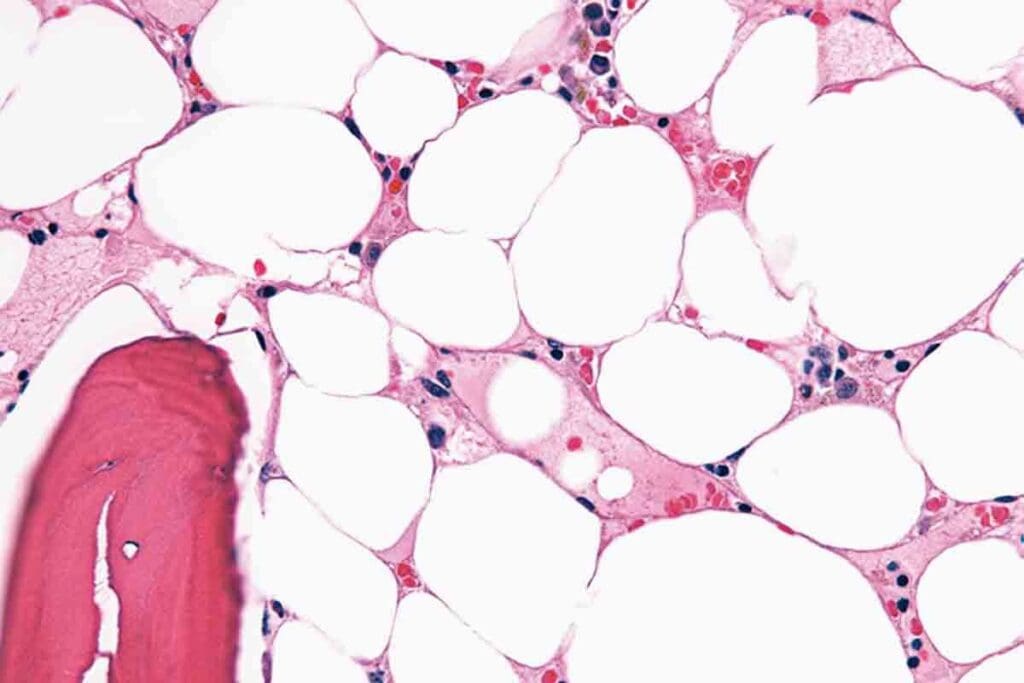
Hematopoietic stem cell transplantation (HSCT) replaces bad bone marrow with healthy cells from a donor. It’s a detailed process that needs careful planning. The main goal is to fix the bone marrow so it can make healthy blood cells again.
First, the patient gets conditioning therapy to weaken their immune system. This clears the way for the new stem cells. Then, the donor stem cells are given to the patient. They go to the bone marrow and start making new blood cells.
This process takes time, and the patient is watched closely. They need to be ready for any problems or if the transplant fails.
Not every patient with aplastic anemia can get a bone marrow transplant. The choice to have HSCT depends on age, health, and if a good donor is found. Young patients with a matched donor are usually the best candidates. Each case is looked at carefully.
To qualify for HSCT, the disease’s severity, past treatments, and health issues are checked. It’s important to pick the right patients to ensure success and safety. This way, we can help more people and reduce risks.
Aplastic anemia bone marrow transplant is a detailed process. It starts with a thorough pre-transplant evaluation. This step is key to check if the patient is a good candidate for the transplant.
The pre-transplant evaluation includes many tests. These tests check the patient’s health and the severity of their aplastic anemia. They also include blood counts and bone marrow biopsies.
We also look at the patient’s medical history. This helps us spot any risks or complications that might happen during or after the transplant. This detailed check helps us make a treatment plan that fits the patient’s needs.
Choosing the right donor is very important. We look for a donor whose Human Leukocyte Antigen (HLA) type matches the patient’s. HLA matching is key to lower the risk of graft-versus-host disease (GVHD), a possible transplant complication.
The donor can be a family member or someone unrelated. We do detailed HLA typing to find the best match. This involves testing for several HLA genes to check compatibility.
The transplant procedure involves putting the donor’s healthy stem cells into the patient’s bloodstream. This is done through an intravenous line, like a blood transfusion.
Before the infusion, the patient gets conditioning treatment. This treatment gets rid of any bad bone marrow and weakens the immune system. This helps the donor’s stem cells to grow and make healthy blood cells.
Recovering from a bone marrow transplant is a long journey. It needs careful medical care and the patient’s full cooperation. The path to getting better includes several stages, from right after the transplant to ongoing check-ups.
The early recovery stage, which can last weeks to months, is very important. During this time, doctors watch for signs of the transplant working, graft-versus-host disease, and infections. “This early phase is when patients are most at risk,”
Patients might feel tired, sick to their stomach, and have mouth sores. To help, doctors use medicines to ease symptoms and prevent infections. It’s key for patients to stick to their treatment plans and keep up with doctor’s visits.
Long-term care is vital for catching any late transplant effects. This includes checking for organ problems, new cancers, and chronic GVHD. Regular visits with the healthcare team are important for catching and treating these issues early.
Doctors also advise on lifestyle changes to aid in recovery. This includes eating right, exercising, and staying away from germs. “Long-term care is about more than just managing problems,” Potential Complications and Management
Complications like GVHD, infections, and the cancer coming back are possible after a transplant. We use treatments like immunosuppressive drugs and antibiotics to prevent these issues.
If problems do happen, acting fast is key. “Quickly finding and treating problems can greatly help patients,”
By knowing the recovery process and following the recommended care, patients can have a better chance of success after a bone marrow transplant for aplastic anemia.
Bone marrow transplantation is a top treatment for aplastic anemia, bringing hope to patients globally. This field has made big strides, leading to better results for many.
The success of bone marrow transplants for aplastic anemia changes with age. Children and young adults often do better than older adults. Research shows that those under 20 have a better chance of long-term survival and cure.
A study in a top medical journal found a big difference in survival rates. Children’s 5-year survival rate was about 80%, while those over 40 had a 50% rate.
Many things affect how well a bone marrow transplant works for aplastic anemia. These include the donor match, the patient’s health before the transplant, and the transplant method.
Knowing these factors helps manage patient hopes and make informed treatment choices. By looking at each patient’s situation, we can guess the transplant’s success better.
Now, patients with aplastic anemia can get top-notch care at specialized centers. These places offer a wide range of services. They are designed to meet the specific needs of those with aplastic anemia.
Managing aplastic anemia well needs a team effort. A team of doctors, including hematologists and oncologists, work together. They create care plans that fit each patient’s needs.
Key components of the multidisciplinary approach include:
Liv Hospital is known for its bone marrow transplant expertise. This is a key treatment for many with aplastic anemia. Our team uses the latest research and guidelines to ensure safe and effective care.
The success of bone marrow transplantation depends on several factors. These include donor selection, HLA matching, and post-transplant care. Our experienced team focuses on each step to improve outcomes.
| Aspect of Care | Description | Benefit to Patient |
| Donor Selection | Careful matching of donors to ensure compatibility | Reduced risk of graft-versus-host disease |
| HLA Matching | Advanced HLA typing for optimal donor-recipient matching | Improved graft survival and function |
| Post-Transplant Care | Comprehensive follow-up care to manage complications | Enhanced recovery and quality of life |
At Liv Hospital, we aim to provide top care for aplastic anemia patients. Our team works together to create personalized plans. We offer hope and healing to those with this condition.
Aplastic anemia is a serious condition that needs quick and effective treatment. It’s not cancer, but knowing its unique traits is key for proper care. We’ve looked at different treatments for aplastic anemia, focusing on bone marrow transplant as a cure for some patients.
Bone marrow transplant, or hematopoietic stem cell transplantation, can cure aplastic anemia. It replaces damaged bone marrow with healthy stem cells. This method has shown great success, mainly for those who can get a transplant.
At places like Liv Hospital, a team of experts works together to care for aplastic anemia patients. Their advanced treatments and knowledge ensure patients get the best care. If you’re looking into treatments, including bone marrow transplant, talk to doctors to find the right cure for you.
Aplastic anemia is a rare blood disorder. It happens when the bone marrow can’t make blood cells. This includes red blood cells, white blood cells, and platelets.
No, it’s not cancer. But, it can raise the risk of getting secondary cancers.
The exact cause is often unknown. But, it can be caused by toxins, certain medicines, viral infections, and autoimmune disorders.
Doctors use blood tests and a bone marrow biopsy. They check how well the bone marrow makes blood cells.
Bone marrow transplant is a key treatment. It replaces the damaged bone marrow with healthy stem cells. This can cure aplastic anemia.
First, there’s an evaluation and donor selection. Then, HLA matching and the transplant procedure. After that, recovery and rehabilitation follow.
Success rates depend on age, donor match, and health. Younger patients with a matched donor tend to have higher success rates.
Some patients might respond to other treatments. But, bone marrow transplant is usually the most effective cure for severe cases.
Recovery starts with a hospital stay. Then, long-term care is needed to manage complications and watch for relapse or graft-versus-host disease.
Liv Hospital uses a team approach. They combine expertise in hematology, oncology, and bone marrow transplantation for complete care.
Yes, with the right treatment, like bone marrow transplant, many patients can achieve long-term remission or cure.
Complications include graft-versus-host disease, infections, and organ damage. These are managed with close monitoring and supportive care.
No, bone marrow is vital for making blood cells. Without it, life-threatening complications can occur, making transplant a critical treatment.
National Center for Biotechnology Information. (2018). Severe aplastic anemia: allogeneic bone marrow transplantation as treatment. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6093726
Medical News Today. (2024). Is aplastic anemia cancer? Retrieved from https://www.medicalnewstoday.com/articles/is-aplastic-anemia-cancer
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!