Last Updated on November 20, 2025 by Ugurkan Demir

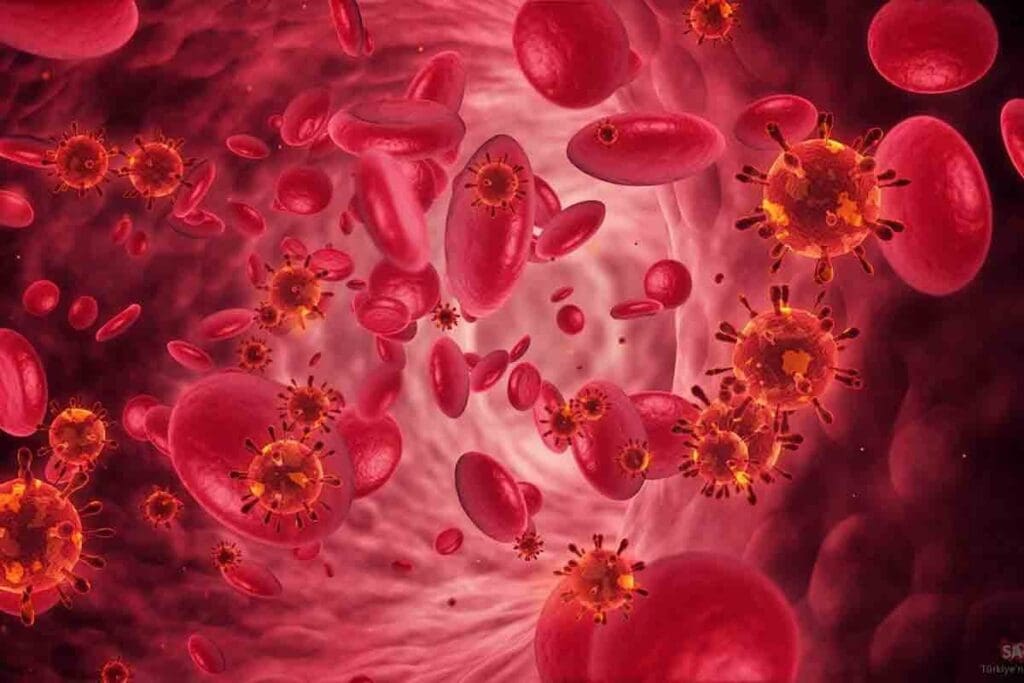
Autoimmune hemolytic anemia (AIHA) is a rare condition. It happens when the body’s defense system sees its own red blood cells as foreign. Then, it makes antibodies to destroy them.
This wrong immune response reduces healthy red blood cells. This leads to symptoms like fatigue, weakness, and shortness of breath. At Liv Hospital, we tackle AIHA’s challenges with care and the latest medical tech.
Our team is all about top-notch healthcare immune system anemia. We make sure patients get the best, most advanced treatments for AIHA.

The human body needs a complex mix of cells to stay healthy. The immune system is key in fighting off infections and diseases. White blood cells are vital in this fight.
White blood cells, or leukocytes, are essential for our immune system. They protect us from infections and foreign materials. There are different types of white blood cells, each with its own job:
Normally, white blood cells get rid of pathogens without harming our own cells. But, in some cases, like autoimmune hemolytic anemia, they can attack and destroy red blood cells.
Red blood cells carry oxygen to all parts of the body. They have hemoglobin, which picks up oxygen in the lungs and releases it in tissues. Keeping red blood cells working right is key to our health.
Red blood cells live about 120 days before being removed by the spleen. In healthy people, new red blood cells are made to replace old ones, keeping the count stable.
A healthy immune system knows the difference between self and non-self, avoiding autoimmunity. Regulatory mechanisms, like certain cytokines and regulatory T cells, keep the immune system in balance.
In a healthy immune response, immune cells are activated just right, preventing too much or too little activity. If this balance is off, it can cause immune disorders, including those that destroy red blood cells.
Knowing how white and red blood cells work and how the immune system regulates itself is key to understanding anemia. By seeing how all these parts work together, we can better understand blood and immune system disorders.
Immune system anemia, also known as autoimmune hemolytic anemia, occurs when the immune system attacks its own red blood cells. This happens when the immune system makes antibodies against these cells, marking them for destruction.
Autoimmune hemolytic anemia (AIHA) is divided into types based on when the antibodies react with red blood cells. The main types are warm AIHA and cold AIHA. Warm AIHA happens at body temperature, while cold AIHA occurs at cooler temperatures, below 30°C.
AIHA can be either primary or secondary. Primary AIHA happens without another condition, while secondary AIHA is linked to diseases like lupus or lymphoma.
AIHA is rare, affecting about 1-3 people per 100,000 each year. It can happen to anyone, but mostly affects adults, and women more than men. The exact number can change based on who is studied and how they are diagnosed.
| Characteristics | Warm AIHA | Cold AIHA |
| Antibody Reaction Temperature | Body temperature (37°C) | Cooler temperatures (<30°C) |
| Common Age Group | Adults | Typically older adults |
| Associated Conditions | Lymphoma, lupus | Infections, lymphoproliferative disorders |
AIHA can cause anemia, leading to symptoms like fatigue, shortness of breath, and pale skin. In severe cases, it can lead to heart problems because the heart has to work harder without enough red blood cells.
This condition can greatly affect a person’s health and quality of life. It’s important to understand and manage AIHA to improve patient outcomes.
The way white blood cells attack red blood cells is quite complex. It involves many parts of the immune system. This is key to understanding anemia, where the balance of blood cells is off.
Hemolysis is when red blood cells are destroyed. This can happen inside or outside blood vessels, mainly in the spleen. Antibodies and complement proteins mark red blood cells for destruction.
When red blood cells are damaged or marked by antibodies, they’re easier for the immune system to destroy. The spleen filters out these damaged red cells from the blood.
White blood cells, like macrophages, eat and destroy red blood cells through phagocytosis. Antibody opsonization helps by making red blood cells more visible to macrophages.
The complement system is a group of proteins important in the immune response. It works with antibodies on red blood cells to create a membrane attack complex. This complex directly breaks down red blood cells.
| Component | Role in Hemolysis |
| Antibodies | Mark red blood cells for destruction |
| Complement Proteins | Activate to form the membrane attack complex |
| Macrophages | Engulf and digest marked red blood cells |
Knowing how white blood cells attack red blood cells is vital for diagnosing and treating autoimmune hemolytic anemia. The interaction between antibodies, complement, and macrophages shows how complex the immune system’s role in hemolysis is.
AIHA, or autoimmune hemolytic anemia, happens when the body’s immune system attacks its own red blood cells. This attack is caused by antibodies. The condition can be divided into types based on the temperature at which the antibodies work best.
Warm AIHA is the most common type. In this case, the antibodies target red blood cells at body temperature. Symptoms can range from mild to severe and include fatigue, jaundice, and shortness of breath. Doctors use lab tests to find these antibodies.
Treatment for warm AIHA usually involves medicines to lower antibody production. Sometimes, blood transfusions are needed to help tissues get enough oxygen.
Cold AIHA happens when antibodies work best at temperatures below body temperature. It often gets worse when exposed to cold. Symptoms include acrocyanosis and hemolytic crises upon cold exposure. Tests for cold agglutinins help diagnose it.
To manage cold AIHA, avoiding cold is key. Doctors might also prescribe immunosuppressive drugs or rituximab to reduce antibody production.
Mixed-type AIHA combines features of both warm and cold AIHA. It’s less common but poses challenges in diagnosis and treatment. The symptoms can vary widely, requiring a tailored treatment approach.
Treating mixed-type AIHA involves a mix of therapies for warm and cold AIHA. This includes immunosuppression and avoiding cold when necessary.
In conclusion, AIHA is a complex condition with different types. Each type needs a specific approach to diagnosis and treatment. Understanding these differences is key to effective management.
To understand how white corpuscles eat red corpuscles, we need to look at the immune system’s role. The process of white blood cells destroying red blood cells is complex. It involves many cell interactions.
Macrophage-mediated phagocytosis is key in this process. Macrophages are white blood cells that eat and break down debris and foreign substances. In cases of anemia, they help remove red blood cells from the blood.
Macrophages find and grab red blood cells marked for destruction. This marking often comes from antibody opsonization. It makes it easier for macrophages to spot and eat the red blood cells.
A study on hemolytic disease shows how important phagocytosis is. It helps get rid of damaged red blood cells from the blood. This keeps the balance of red blood cells in the body.
Antibody opsonization is when antibodies stick to red blood cells, marking them for destruction. This makes it easier for macrophages to find and eat the red blood cells.
Antibodies play a big role in marking red blood cells for destruction. This shows how the immune system works together to destroy red blood cells.
We can see how white blood cells destroy red blood cells using microscopes.
Learning about how white corpuscles eat red corpuscles helps us understand anemia better. By looking at macrophage-mediated phagocytosis and antibody opsonization, we see how the immune system works.
To understand immune dysregulation in anemia, we look at both inside and outside factors. Genetic predisposition and environmental triggers play big roles. We’ll see how these factors lead to anemia.
Genetics are key in autoimmune hemolytic anemia (AIHA). Some genes make people more likely to get anemia. Studies have found certain genes that mess with the immune system, raising AIHA risk.
Environmental factors and infections also cause AIHA. Toxins or infections can set off an immune attack on red blood cells. For example, some viruses can make the immune system attack red blood cells by mistake.
People with other autoimmune diseases are more likely to get AIHA. Diseases like lupus or rheumatoid arthritis can lead to anemia. Having one autoimmune disease can make you more likely to get others, causing more immune problems.
Knowing these causes helps us treat anemia better. The mix of genetics, environment, and other diseases shows how complex this issue is. We need a detailed treatment plan to tackle it.
Aplastic anemia is a rare and serious condition. It happens when the immune system mistakenly attacks the stem cells in the bone marrow.
This condition is different from other anemias, like hemolytic anemia. In hemolytic anemia, the immune system targets mature red blood cells. But in aplastic anemia, the problem is with the production of blood cells, not just their survival.
Hemolytic anemia occurs when the immune system makes antibodies against the patient’s own red blood cells. This marks them for destruction. On the other hand, aplastic anemia is when the immune system attacks the stem cells in the bone marrow. These stem cells are responsible for making all types of blood cells.
To understand the difference, let’s consider the following table:
| Characteristics | Aplastic Anemia | Hemolytic Anemia |
| Primary Issue | The immune system attacks stem cells in the bone marrow | The immune system targets mature red blood cells |
| Effect on Blood Cells | Reduced production of all blood cell types | Destruction of red blood cells |
| Common Symptoms | Fatigue, infections, bruising | Jaundice, fatigue, shortness of breath |
The attack on stem cells in the bone marrow leads to a big drop in the production of red blood cells, white blood cells, and platelets. This can cause anemia, infections, and bleeding disorders.
The exact ways the immune system attacks stem cells in aplastic anemia are complex. Both cellular and humoral immunity are involved in the disease.
Understanding these mechanisms is key to finding effective treatments. Immunosuppressive therapies aim to reduce the abnormal immune response. This helps the bone marrow to recover its blood cell production abilities.
Immune-mediated anemias are a big challenge for doctors. They need a detailed plan to diagnose and treat them. We’ll look at the latest ways to do this, focusing on what works best.
To find out if someone has immune-mediated anemia, doctors use several tests. These include:
Doctors also look at symptoms and medical history. Getting the diagnosis right is key to a good treatment plan.
Immunosuppressive treatments are a mainstay for immune-mediated anemias. They help stop the immune system from attacking red blood cells. Common treatments include:
It’s important to customize treatment for each patient to get the best results.
Blood transfusions are often needed for severe anemia. We match the blood type carefully to avoid bad reactions. Supportive care, like folic acid and watching for problems, is also key.
Each type of immune-mediated anemia, like warm AIHA, cold AIHA, and mixed AIHA, needs its own treatment plan. Knowing the details of each type helps doctors choose the right therapy.
We keep learning and improving how to treat immune-mediated anemias. This helps patients live better lives.
Immune system anemia, like autoimmune hemolytic anemia (AIHA), is a big challenge in medicine. We’ve looked into how white blood cells attack red blood cells. This leads to hemolysis and health problems.
It’s key to understand AIHA well. This helps in giving the right care and treatment for each patient. Doctors can then use immunosuppressive therapies and supportive care.
As we learn more about AIHA, we can help patients more. Treating AIHA means managing the condition and other autoimmune diseases. It’s about making sure patients are well overall.
Knowing how the immune system affects anemia helps us find better treatments. Our aim is to give top-notch healthcare with full support. Understanding the immune system and anemia is a big part of this goal.
Autoimmune hemolytic anemia occurs when the immune system attacks and destroys red blood cells. This leads to anemia.
White blood cells destroy red blood cells. They do this through antibodies and macrophages.
Symptoms include fatigue, pale skin, shortness of breath, and jaundice. These happen because red blood cells are being destroyed.
There are warm, cold, and mixed types. Each type has its own characteristics and how it reacts to temperature.
Doctors use tests like the direct Coombs test and the indirect Coombs test. They also look for autoantibodies against red blood cells.
The complement system helps destroy red blood cells. It makes antibodies work better or marks cells for destruction.
Yes, genetics can play a part. It can affect how the immune system works.
Aplastic anemia stops blood cell production. Hemolytic anemia destroys red blood cells.
Treatment includes immunosuppressive therapies and blood transfusions. Supportive care is also important, depending on the type of AIHA.
A healthy immune system keeps autoimmunity in check. It makes sure white blood cells target pathogens, not the body’s own cells.
It can cause severe anemia and cardiovascular problems. It also reduces the quality of life.
Yes, infections and environmental factors can trigger it in some people.
Yes, having other autoimmune conditions can raise the risk. This is because of shared immune system problems.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!