White blood cells are key in fighting off infections and diseases. But in rare cases, like autoimmune hemolytic anemia, they can attack red blood cells by mistake.red blood cell eating white blood cellWhat Causes Blood to Thin? Understanding the Dangers of Thin Blood This shows how our body’s systems must work together perfectly to keep us healthy.
At Liv Hospital, we focus on our patients to tackle these complex health issues. Our team uses the latest technology to give top-notch care. This ensures our patients get the help they need to deal with these tough health problems.
Key Takeaways
- White blood cells can mistakenly target red blood cells in autoimmune conditions.
- Autoimmune hemolytic anemia is a rare condition where the immune system produces antibodies against red blood cells.
- Liv Hospital offers a patient-centered approach to diagnosing and treating complex hematological conditions.
- Understanding the balance of the hematological system is key to our health.
- Cutting-edge technology is essential in diagnosing and treating autoimmune hemolytic anemia.
Understanding Blood Cells: The Foundation of Our Immune System

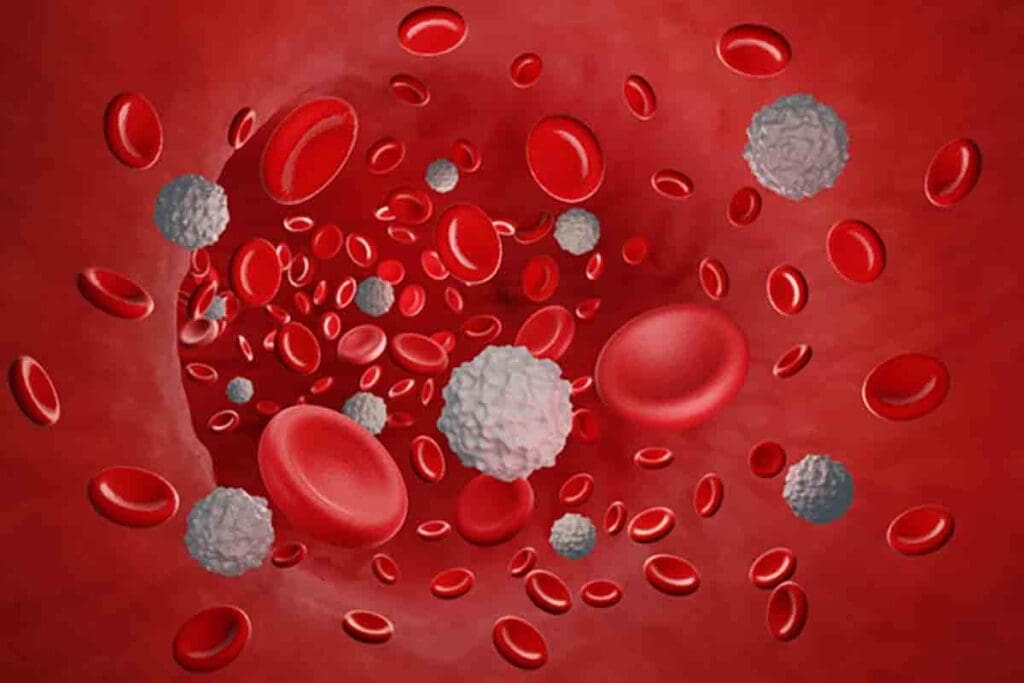
To understand our immune system, we must know about blood cells. Human blood is a complex mix of cells, each with its own role. These roles are key to keeping us healthy.
Let’s look at what makes up human blood. It mainly has red blood cells, white blood cells, and platelets. Together, they carry oxygen, fight infections, and help blood clot.
The Composition of Human Blood
Human blood has red blood cells, white blood cells, and platelets. Red blood cells carry oxygen. White blood cells fight infections. Platelets help blood clot to stop bleeding.
Red Blood Cells: Structure and Function
Red blood cells are disk-shaped and carry hemoglobin. Hemoglobin binds to oxygen, letting it reach our body’s tissues. Their shape lets them move through narrow blood vessels, ensuring oxygen gets where it needs to.
White Blood Cells: The Body’s Defense Force
White blood cells are vital for our immune system. They fight off infections and invaders. There are many types, like neutrophils, lymphocytes, and monocytes, each with its own job in fighting off threats.
Knowing how these blood cells work helps us understand our immune system. It shows how our body responds to challenges.
The Normal Function of White Blood Cells
White blood cells are key to our immune system. They protect us from harmful pathogens. These cells help defend our body by finding and removing foreign substances and microorganisms.
The Protective Role of White Blood Cells
White blood cells, also known as leukocytes, are made in the bone marrow. They travel through the body via the bloodstream and lymphatic system. Their main job is to fight off infections and diseases caused by harmful bacteria, viruses, fungi, and other pathogens.
There are different types of white blood cells, each with its own role:
- Neutrophils: These cells are mainly involved in the first response to infections, mostly bacterial ones.
- Lymphocytes: Lymphocytes, including B cells and T cells, are key in specific immune responses. They help in making antibodies and cell-mediated immunity.
- Monocytes: Monocytes turn into macrophages. These cells help in phagocytosis and present antigens to lymphocytes.
- Eosinophils: Eosinophils fight parasitic infections and allergic reactions.
- Basophils: Basophils are involved in inflammatory reactions, mainly in allergic responses.
Phagocytosis: How White Blood Cells Normally “Eat” Foreign Particles
Phagocytosis is a vital process where certain white blood cells engulf and destroy foreign particles and microorganisms. This process is essential for removing pathogens and debris from the body.
The steps in phagocytosis include:
- Recognition: The white blood cell identifies the foreign particle or microorganism.
- Engulfment: The cell membrane of the white blood cell extends around the particle, forming a phagosome.
- Digestion: The phagosome fuses with lysosomes, which contain digestive enzymes, to form a phagolysosome where the particle is broken down.
- Elimination: The digested remnants are then expelled from the cell.
The Immune Recognition Process
The immune recognition process is vital for the immune system to work properly. White blood cells recognize pathogens through various mechanisms. This includes pattern recognition receptors (PRRs) that identify pathogen-associated molecular patterns (PAMPs).
This recognition triggers an immune response. This response can involve:
- Activation of immune cells: Recognition of pathogens leads to the activation of various immune cells, including macrophages and lymphocytes.
- Production of cytokines: Cytokines are signaling molecules that facilitate communication between immune cells, coordinating the immune response.
- Initiation of inflammation: The recognition of pathogens can lead to the initiation of an inflammatory response. This helps to isolate and eliminate the infection.
When Defense Turns Against Itself: Autoimmunity Basics
Autoimmunity happens when the immune system can’t tell the difference between its own cells and foreign invaders. This mistake causes the immune system to attack the body’s own tissues. This leads to different autoimmune disorders.
Understanding Autoimmune Disorders
Autoimmune disorders occur when the immune system mistakenly attacks the body’s own cells, tissues, and organs. Autoimmunity can cause diseases like rheumatoid arthritis, lupus, and autoimmune hemolytic anemia.
These disorders have many causes, including genetics, environmental factors, and immune system problems. Knowing these causes helps in finding better treatments.
How the Immune System Distinguishes “Self” from “Non-Self”
The immune system must know the difference between “self” and “non-self” to work properly. This is done through a complex process involving different immune cells and mechanisms.
- Tolerance Mechanisms: The immune system learns to ignore self-antigens through central and peripheral tolerance.
- Immune Cell Education: T cells are educated in the thymus to avoid reacting to self.
- Regulatory Cells: Regulatory T cells help keep the immune system balanced and prevent autoimmunity.
Breaking of Immune Tolerance
Immune tolerance means the immune system ignores self-antigens, preventing autoimmunity. But when this tolerance is lost, the immune system can attack the body’s own cells.
Things that can break immune tolerance include:
- Genetic Factors: Some genes can make a person more likely to get autoimmunity.
- Environmental Triggers: Infections, drugs, and other environmental factors can start autoimmune reactions.
- Molecular Mimicry: Pathogens with antigens that look like self-antigens can cause autoimmunity.
Understanding these mechanisms is key to finding treatments for autoimmune diseases.
The Phenomenon of Red Blood Cell Eating White Blood Cell: Clarifying the Confusion
The idea that red blood cells eat white blood cells is a myth. The real story is more complex. We need to understand how these cells work together in our blood.
Common Misconceptions in Blood Cell Interactions
Many think red blood cells can eat white blood cells. But that’s not true. White blood cells, not red blood cells, are the ones that can eat and destroy other cells.
Why do people get this wrong? It’s because of:
- Misunderstanding the roles of different blood cells
- Lack of clear information about how cells interact
- Misreading scientific studies
Scientific Evidence: Which Cells Actually “Eat” Which?
Science proves that white blood cells are the ones that can eat and destroy. They engulf and get rid of harmful invaders, dead cells, and debris. This is key to keeping us healthy and fighting off infections.
Research shows white blood cells are the main players in our immune system. They can even attack and destroy red blood cells in some cases. For example, in autoimmune hemolytic anemia, white blood cells target and destroy red blood cells.
The Reality of Cellular Interactions in the Bloodstream
In our blood, red and white blood cells have different jobs. Red blood cells carry oxygen, while white blood cells help fight off infections. Knowing their roles helps us understand how they work together.
It’s not like one cell eats the other. Instead, they work together in a complex way. In some cases, white blood cells might attack red blood cells, but that’s due to immune system problems, not normal function.
Important points to remember:
- White blood cells are responsible for eating and destroying other cells.
- Red blood cells mainly carry oxygen.
- Immune system problems can cause white blood cells to attack red blood cells.
Mechanisms of White Blood Cells Attacking Red Blood Cells
The immune system sometimes attacks red blood cells by mistake. This is a big problem in autoimmune hemolytic anemia. In this condition, the immune system can’t tell the difference between self and non-self. It makes antibodies against the body’s own red blood cells.
The Process of Antibody Production Against Red Blood Cells
Antibodies against red blood cells are a key part of the immune system’s attack. Autoantibodies are made by B cells, a type of white blood cell. They see red blood cells as foreign and bind to them, marking them for destruction.
The process involves several key steps:
- Recognition of red blood cell antigens by the immune system
- Activation of B cells and production of autoantibodies
- Binding of autoantibodies to red blood cell surfaces
Complement System Activation in Hemolysis
The complement system is a group of proteins that help fight off infections. When autoantibodies bind to red blood cells, they activate the complement system. This leads to the formation of a membrane attack complex (MAC). The MAC creates pores in the red blood cell membrane, causing it to burst.
The activation of the complement system in hemolysis involves:
- Binding of autoantibodies to red blood cell surfaces
- Activation of C1, the first component of the complement system
- Cascade of reactions leading to the formation of the membrane attack complex
Cellular Pathways Leading to Red Blood Cell Destruction
Cellular pathways also play a big role in getting rid of red blood cells. Macrophages, a type of white blood cell, recognize and engulf red blood cells. This happens when the cells are marked by autoantibodies or complement proteins.
The key cellular pathways involved include:
- Recognition of opsonized red blood cells by macrophages
- Phagocytosis of red blood cells by macrophages
- Degradation of red blood cells within macrophages
Autoimmune Hemolytic Anemia: When White Cells Target Red Cells
When the immune system mistakes its own red blood cells, it can cause autoimmune hemolytic anemia. This happens when the body makes antibodies against its own red blood cells. This marks them for destruction, leading to anemia because red blood cells are destroyed faster than they can be made.
This condition is not just one disease but a group of conditions with different causes and symptoms. Knowing the different types is key to treating them right.
Types of Autoimmune Hemolytic Anemia
Autoimmune hemolytic anemia is divided into types based on how the antibodies react with red blood cells and other signs.
Warm Autoimmune Hemolytic Anemia: Affecting 1 in 8,000 People
Warm autoimmune hemolytic anemia is the most common type. It happens when antibodies bind to red blood cells at body temperature. It affects about 1 in 8,000 people and is often linked to other autoimmune diseases or lymphoproliferative disorders.
The symptoms can range from mild to severe. They include fatigue, jaundice, and shortness of breath because of fewer red blood cells.
Cold Agglutinin Disease and Other Variants
Cold agglutinin disease is another type of autoimmune hemolytic anemia. It occurs when antibodies react with red blood cells at cold temperatures. This can cause hemolysis when exposed to cold.
Other types include mixed-type autoimmune hemolytic anemia, with both warm and cold antibodies, and drug-induced autoimmune hemolytic anemia, caused by certain medications.
To understand the different types of autoimmune hemolytic anemia and their characteristics, let’s look at the following table:
| Type | Characteristics | Triggers |
| Warm Autoimmune Hemolytic Anemia | Antibodies bind to red blood cells at body temperature | Often associated with autoimmune diseases or lymphoproliferative disorders |
| Cold Agglutinin Disease | Antibodies react with red blood cells at cold temperatures | Exposure to cold |
| Mixed-Type | Presence of both warm and cold antibodies | Varies; can be associated with infections, autoimmune diseases, or lymphoproliferative disorders |
Knowing the specific type of autoimmune hemolytic anemia is key to finding the right treatment. Some patients might not need treatment, while others might need immunosuppressive therapy, blood transfusions, or other interventions to manage their condition.
Causes and Risk Factors for Immune Dysregulation
Autoimmune conditions develop from a mix of genetic, environmental, and external factors. Knowing these causes and risk factors helps us understand why the immune system sometimes attacks the body’s own cells.
Genetic Predisposition to Autoimmune Disorders
Genetics plays a big role in who gets autoimmune disorders. Some genetic markers make people more likely to get conditions like autoimmune hemolytic anemia. But having these markers doesn’t mean someone will definitely get a disease.
Studies have found genes linked to higher risks of autoimmune diseases. For example, changes in the HLA gene complex are tied to many autoimmune conditions. Knowing these genetic links helps us spot who’s at higher risk.
| Gene | Associated Autoimmune Disease | Risk Factor |
| HLA-DRB1 | Rheumatoid Arthritis | High |
| HLA-B27 | Ankylosing Spondylitis | High |
| CTLA-4 | Type 1 Diabetes, Autoimmune Thyroid Disease | Moderate |
Environmental Triggers and Infections
Environmental factors and infections can start autoimmune responses in people who are already at risk. Being exposed to certain toxins or infections can lead to an autoimmune reaction.
For instance, some research links infections like Epstein-Barr virus (EBV) to autoimmune diseases in people with the right genes. Also, being exposed to certain chemicals can raise the risk of getting autoimmune conditions.
Medications and Other External Factors
Some medications and external factors can mess with the immune system. Drugs like procainamide and hydralazine can cause autoimmune reactions in some people. Lifestyle choices and other exposures also play a part in autoimmune diseases.
It’s important to understand how these factors work together. By knowing and reducing risk factors, we might be able to lower the number of people who get autoimmune diseases.
Diagnosis and Treatment Approaches
Understanding how to diagnose and treat autoimmune hemolytic anemia is key. It helps manage the condition well and improves patient results. Diagnosing this condition requires a mix of clinical checks, lab tests, and sometimes ruling out other causes of hemolysis.
Symptoms and Clinical Manifestations
Autoimmune hemolytic anemia can cause fatigue, shortness of breath, and jaundice. These symptoms happen because there are fewer red blood cells. The severity of these symptoms can differ a lot among patients.
Laboratory Tests and Diagnostic Criteria
Several lab tests are used to diagnose autoimmune hemolytic anemia. The direct antiglobulin test (DAT) checks for antibodies or complement proteins on red blood cells. Other tests include a complete blood count (CBC), reticulocyte count, and lactate dehydrogenase (LDH) levels to measure hemolysis.
Treatment Strategies for Autoimmune Hemolytic Anemia
Treatment for autoimmune hemolytic anemia starts with corticosteroids to lessen the immune system’s attack on red blood cells. For severe cases or when corticosteroids don’t work, treatments like immunosuppressive drugs, rituximab, or splenectomy might be used.
Conclusion: Current Research and Future Directions
Autoimmune hemolytic anemia is a complex condition. Ongoing research is key to understanding it better and finding new treatments. Scientists are working hard to uncover the causes and find new ways to treat it.
They are looking into how genetics, the environment, and infections might play a part. They also want to explore new treatments like immunosuppressive therapies and biologics. The goal is to make treatments more effective for each patient.
As we learn more, we’ll see better treatments come along. This will help improve life for those with this condition. We’re on the path to making a big difference in their lives.
FAQ
What is the normal function of white blood cells in the body?
White blood cells protect us from infections and invaders. They find and destroy harmful cells. This keeps our body healthy.
Can red blood cells eat white blood cells?
No, red blood cells can’t eat white blood cells. It’s the other way around. White blood cells can engulf and destroy other cells, including red blood cells in some cases.
What happens when white blood cells mistakenly target red blood cells?
When white blood cells attack red blood cells by mistake, it causes autoimmune hemolytic anemia. This is when the immune system attacks the red blood cells, marking them for destruction.
What are the different types of autoimmune hemolytic anemia?
There are several types, like warm autoimmune hemolytic anemia and cold agglutinin disease. Each has its own effects on patients.
How is autoimmune hemolytic anemia diagnosed?
Doctors use a mix of clinical checks and lab tests, like the direct Coombs test. They look for signs of the condition to make a diagnosis.
What are the treatment strategies for autoimmune hemolytic anemia?
Treatments include corticosteroids and immunosuppressive therapy. Sometimes, blood transfusions are needed. These aim to stop the immune system from attacking red blood cells and manage symptoms.
Are there any genetic factors that contribute to autoimmune hemolytic anemia?
Yes, genes can influence the risk of autoimmune disorders, including autoimmune hemolytic anemia. They affect how the immune system works.
Can external factors trigger autoimmune hemolytic anemia?
Yes, things like certain medicines, infections, and environmental factors can trigger it. These can set off an immune response in people who are prone to it.
What is the role of the complement system in hemolysis?
The complement system helps fight off pathogens. But in autoimmune hemolytic anemia, it can attack red blood cells. This contributes to their destruction.
How do white blood cells identify and destroy pathogens?
White blood cells recognize and destroy pathogens in various ways. They engulf and break down harmful cells. This keeps us safe from infections.
References
- Michalak, S. S., Wozniak, K., Bolkun, L., & Wiktor-Jedrzejczak, W. (2020). Autoimmune hemolytic anemias: classifications, pathogenesis, and therapies. Frontiers in Immunology, 11, 1931. https://pmc.ncbi.nlm.nih.gov/articles/PMC7677104/