Last Updated on November 20, 2025 by Ugurkan Demir

Hemolytic anemia happens when red blood cells are destroyed faster than they’re made. This leads to serious symptoms.
At Liv Hospital, we use advanced tests to find out can anemia cause fever and how hemolytic anemia leads to jaundice and yellow eyes.
Can anemia cause fever? Anemia means not enough red blood cells or hemoglobin. It can cause tiredness and trouble breathing. In some cases, anemia—especially when linked to infections or inflammation—may also be associated with fever.
Hemolytic anemia happens when the body gets rid of red blood cells too quickly. This makes it hard for the body to get enough oxygen. It can cause many health problems because of the lack of red blood cells.
The word “hemolytic” means the breakdown of red blood cells. Hemolytic anemia occurs when the body gets rid of too many red blood cells. This happens faster than the bone marrow can make new ones.
This breakdown can happen inside or outside the blood vessels. It often happens in the spleen or liver. The hemolytic meaning also includes the release of hemoglobin into the blood. This can cause jaundice because of the buildup of bilirubin.
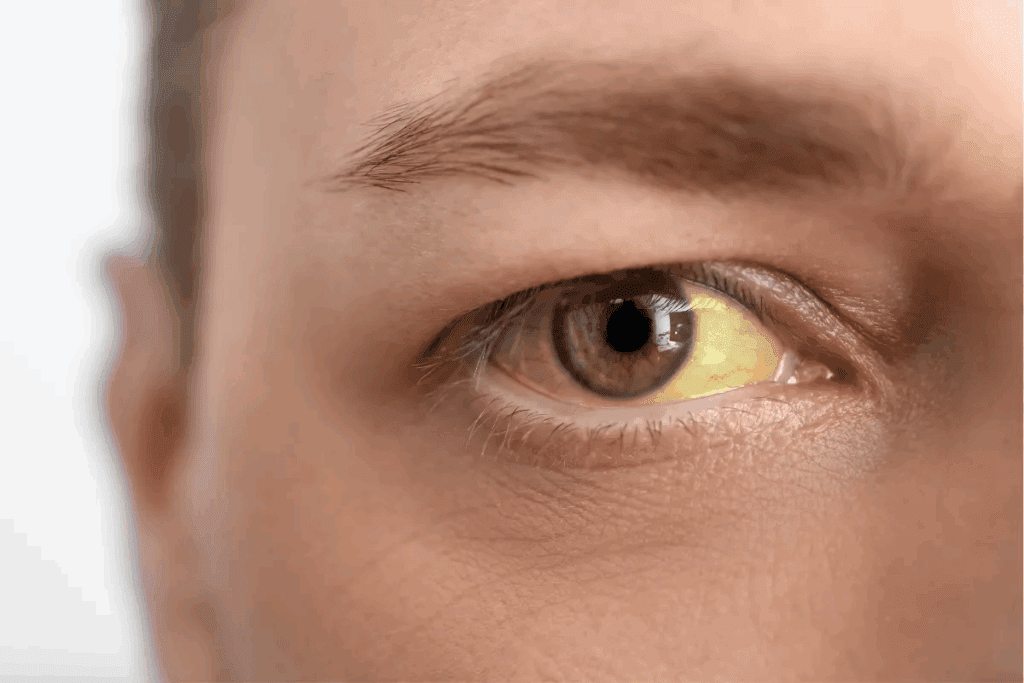
When too many red blood cells are destroyed, bilirubin levels go up. This leads to jaundice and yellow eyes. The body doesn’t have enough red blood cells to carry oxygen to tissues and organs.
This problem can come from many things, like genetic disorders, infections, or some medicines. Knowing what causes and affects hemolytic anemia is key to treating it.

Understanding erythrocyte hemolysis is key to diagnosing and managing hemolytic anemia. This condition is when too many red blood cells are destroyed. It can cause anemia, jaundice, and other health issues.
Red blood cells (RBCs) live about 120 days. They go through changes that lead to their removal. The process of making, maturing, and destroying RBCs is carefully controlled. Any imbalance can cause hemolytic anemia.
Hemolysis is when RBCs are destroyed. This can happen inside or outside blood vessels. It’s caused by autoimmune disorders, infections, and certain medications. The breakdown of RBCs can release hemoglobin into the blood, leading to hemoglobin fever and other issues.
Intravascular hemolysis happens inside blood vessels. It’s linked to paroxysmal nocturnal hemoglobinuria (PNH) and mechanical heart valves. Extravascular hemolysis occurs outside blood vessels, mainly in the spleen. It’s seen in hereditary spherocytosis and autoimmune hemolytic anemia. Knowing the difference is vital for correct diagnosis and treatment.
In conclusion, erythrocyte hemolysis is a complex issue that can cause health problems. Understanding the lifecycle of RBCs and the differences between intravascular and extravascular hemolysis is key to managing hemolytic anemia well.
Hemolytic anemia occurs when the body breaks down red blood cells too fast. This can start an inflammatory response, leading to fever. It happens when the body can’t make new red blood cells fast enough.
When red blood cells break down, they release hemoglobin into the blood. This can start an inflammatory response. The body’s defense mechanism is at work.
The inflammatory response is caused by cytokines and other substances. These can make you feel feverish by affecting your body’s temperature control.
The process involves several key steps:
Fever from hemolytic anemia, known as “hemoglobin fever,” is complex. It’s not just the free hemoglobin that causes fever. It’s how the body reacts to it.
The severity of the fever can vary. Some people might just have a mild fever. Others might have a more serious reaction.
The factors that affect how severe the fever is include:
In conclusion, anemia and fever are mainly linked in cases of hemolytic anemia. Understanding this connection is key to diagnosing and treating patients with fever.
Hemolytic anemia shows itself in many ways, like jaundice and yellow eyes. This happens because too many red blood cells are destroyed. The body can’t make enough new ones, so bilirubin builds up.
When red blood cells break down too fast in hemolytic anemia, more bilirubin is made. The liver usually gets rid of bilirubin through bile. But if too much is made, the liver can’t keep up.
This leads to bilirubin building up in the blood. It makes the skin and eyes turn yellow, known as jaundice. Jaundice anemia is when someone with anemia also has jaundice, showing they are connected.
Yes, anemia can cause yellow eyes, mainly in hemolytic anemia. The breakdown of red blood cells increases bilirubin, turning the yes yellow.
Not all anemia causes yellow eyes. But, in hemolytic anemia, it’s a common sign. Knowing the link between anemia and yellow eyes helps in diagnosing and treating hemolytic anemia.
To figure out why eyes turn yellow, doctors do blood tests. They check bilirubin levels and red blood cell health. Understanding the connection between hemolytic anemia and its symptoms is key to good care.
It’s important to know the types and causes of hemolytic anemia for proper treatment. This condition can be inherited or acquired, each with its own causes and effects.
Inherited hemolytic anemias come from genetic mutations. These affect how red blood cells are made or work. Sickle cell disease and thalassemia are examples. These conditions lead to ongoing red blood cell breakdown, needing constant care.
Acquired hemolytic anemia can come from autoimmune disorders or certain drugs. Autoimmune hemolytic anemia happens when the body attacks its own red blood cells. Drug-induced hemolytic anemia occurs when some medications destroy red blood cells.
Drugs like some antibiotics and anti-inflammatory medicines can cause this. Finding the cause is key to diagnosing acquired hemolytic anemia.
Chronic hemolysis, whether inherited or acquired, has serious long-term effects. It can cause jaundice, anemia, and gallstones. Managing it requires careful monitoring, medication, and lifestyle changes.
Knowing the causes and types of hemolytic anemia helps in creating effective treatment plans. Healthcare providers can then tailor treatments to manage the condition better and improve patient outcomes.
To diagnose hemolytic anemia, doctors use several steps. These include blood tests, looking at your medical history, and a physical check-up. Lab tests are key in confirming the diagnosis.
Tests like hemoglobin levels, blood smears, and the Coombs test are used. A doctor will look at these results to find out why you have hemolytic anemia.
Knowing how to diagnose hemolytic anemia is important. It helps doctors create a treatment plan that works for you. This plan combines what they find in your tests and your overall health.
Getting the right diagnosis is vital for treating hemolytic anemia. By learning how to diagnose it, doctors can help patients live better lives. This improves their health and happiness.
Hemolytic anemia happens when red blood cells are destroyed too quickly. This leads to a shortage of these cells.
Symptoms include feeling very tired, short of breath, and jaundice. You might also notice yellow eyes.
Yes, fever can occur in hemolytic anemia. It’s due to the body’s reaction to the destruction of red blood cells.
Jaundice is a sign of hemolytic anemia. It happens when too many red blood cells are broken down, causing bilirubin to build up.
Doctors use blood tests, medical history, and physical exams to diagnose it. It’s a thorough process.
Intravascular hemolysis happens inside blood vessels. Extravascular hemolysis occurs outside, like in the spleen.
It can be caused by genetic disorders, infections, certain medicines, and autoimmune diseases.
Yes, yellow eyes can happen in hemolytic anemia. It’s because of the buildup of bilirubin.
Chronic hemolysis is when red blood cells are destroyed over a long time. It can cause ongoing anemia and other issues.
Treatment varies based on the cause. It might include medicines, transfusions, or other interventions.
Erythrocyte hemolysis is when red blood cells are destroyed. It can be due to genetic disorders or infections.
Some types are inherited. Others are caused by infections or medicines.
National Institutes of Health, PMC. (n.d.). Hemolytic anemia. Retrieved from
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!