Last Updated on November 20, 2025 by Ugurkan Demir

At Liv Hospital, we aim to give top-notch healthcare. We support patients from around the world. Acute Lymphoblastic Leukemia (ALL) is a fast-growing blood disease. It happens when the bone marrow makes too many immature lymphoblasts.
ALL stands out because it mainly affects lymphoid cells. Knowing this helps us treat it better. We offer top cancer care with a focus on the patient. This ensures they get the best care with kindness.
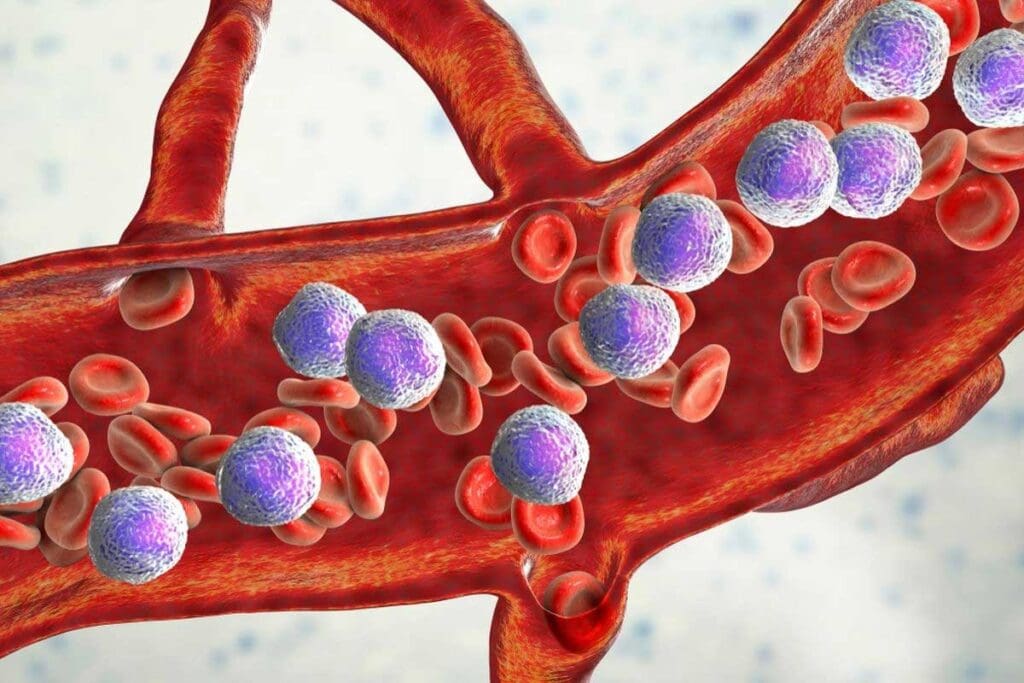
Acute Lymphoblastic Leukemia (ALL) is a cancer that affects the blood and bone marrow. It is caused by the abnormal production of white blood cells called lymphoblasts.
ALL is a serious condition where the bone marrow makes too many immature white blood cells. These cells, or lymphoblasts, can’t fight infections well. The hallmark of ALL is the rapid production of these abnormal cells, which take over the bone marrow and cause health problems.
The basic characteristics of ALL include:
The bone marrow is key in the development of Acute Lymphoblastic Leukemia. It’s the spongy tissue inside bones like the hips and thighbones. It’s responsible for making blood cells. In ALL, genetic mutations in the bone marrow cells cause it to produce lymphoblasts instead of normal blood cells.
Because of this, the bone marrow gets filled with these abnormal cells. This makes it hard to produce healthy blood cells. This can cause anemia, infections, and easy bruising or bleeding.
“The bone marrow’s role in ALL is critical, as it is the site where the disease originates and progresses.”
Expert in Hematology
Understanding the bone marrow’s role in ALL is key to finding effective treatments. It helps target the disease’s root cause.
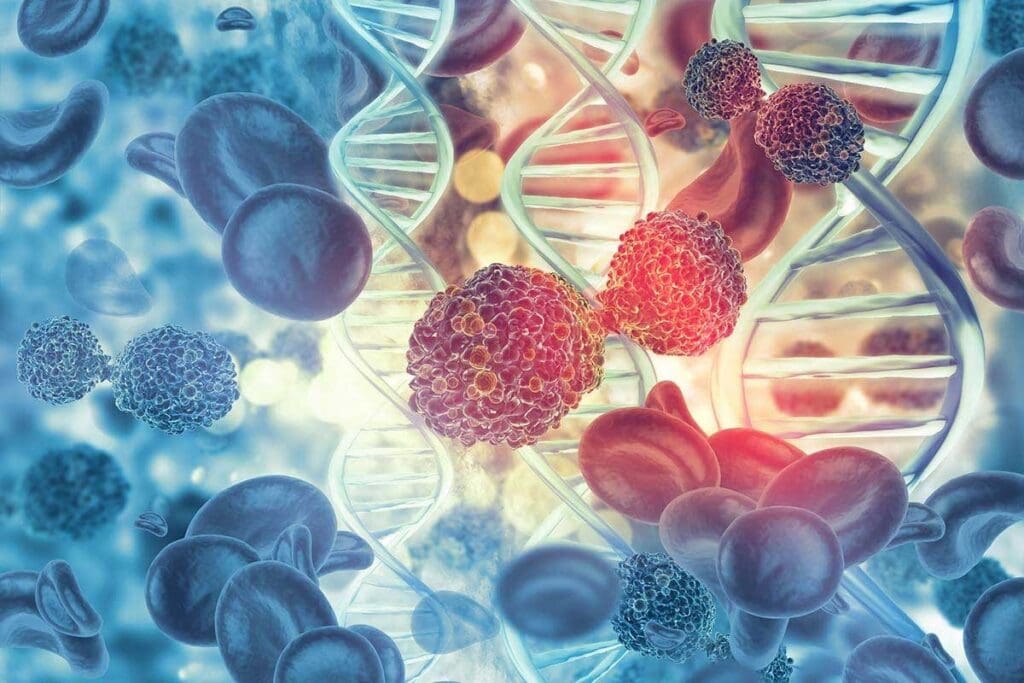
To understand ALL, we must look at the changes in lymphoblasts. Acute Lymphoblastic Leukemia (ALL) is a complex disease. It causes lymphoblasts to grow out of control in the bone marrow.
In ALL, lymphoblasts grow and fail to mature. This leads to a buildup of immature cells in the bone marrow. Normal blood cells are pushed out.
The mutations in ALL make bone marrow cells grow and divide without stopping. This causes too many immature lymphoblasts. It disrupts normal blood production, causing problems.
Genetic and chromosomal changes are key in ALL. They affect how cells grow, differentiate, and survive.
Common genetic changes include mutations in TP53 and the Philadelphia chromosome. These changes help ALL cells grow and multiply.
| Genetic Mutation | Description | Impact on ALL |
| Philadelphia Chromosome | A chromosomal translocation between chromosomes 9 and 22 | Results in the creation of a fusion gene, BCR-ABL, promoting leukemic cell proliferation |
| TP53 Mutation | A mutation in the tumor suppressor gene TP53 | Impaired cell cycle regulation and apoptosis, contributing to cancer progression |
| Hyperdiploidy | Presence of more than 50 chromosomes per leukemic cell | Associated with a favorable prognosis in pediatric ALL |
ALL gets worse as more lymphoblasts build up in the bone marrow. They also spread to other organs. This can cause anemia, infections, and bleeding problems.
Knowing how ALL works is key to finding better treatments. By focusing on the root causes, we can help patients live better lives.
The exact reasons for Acute Lymphoblastic Leukemia (ALL) are not known. But several risk factors have been found. Knowing these can help figure out who might be at risk and how to prevent it.
Genetics is a big part of ALL. Some genetic disorders, like Down syndrome, raise the risk of getting ALL. Other genetic changes can also make someone more likely to get this disease.
People with certain genetic syndromes are more at risk. This shows how important it is to screen and watch for these conditions.
Some environmental factors can raise the risk of ALL. High levels of radiation, like from nuclear accidents, can increase this risk. Some studies also hint at a link between ALL and certain chemicals, but more research is needed.
Being treated for other cancers with chemotherapy or radiation can raise the risk of ALL. These treatments can harm DNA in cells, leading to leukemia.
Knowing the risks from past cancer treatments helps in caring for patients who have had these therapies.
Even though we don’t know all the causes of ALL, knowing the risks helps in early detection and prevention. More research is needed to understand how genetics, environment, and other factors play a role in ALL.
It’s important to know the signs of Acute Lymphoblastic Leukemia (ALL) for early treatment. ALL affects the blood and immune system in different ways.
Symptoms related to blood happen because of too many lymphoblasts in the bone marrow. This leads to fewer normal blood cells. Common signs include:
These symptoms show that the bone marrow can’t make enough healthy blood cells. This is a key sign of Acute Lymphoblastic Leukemia.
ALL also causes symptoms that affect the whole body. These can include:
These symptoms can be mistaken for other illnesses. It’s key to see a doctor if they don’t go away or get worse.
If you or someone you know has these symptoms, get medical help right away. Early treatment can greatly improve the chances of recovery from ALL. We suggest talking to a doctor if you notice:
Knowing these signs can help catch ALL early. This can lead to better treatment results.
It’s important to know the difference between “Acute Lymphoblastic Leukemia” and “Acute Lymphocytic Leukemia.” Both names describe the same cancer that affects the blood and bone marrow.
The names for leukemia have changed over time. “Acute Lymphocytic Leukemia” and “Acute Lymphoblastic Leukemia” were once used in the same way. This was because of how the disease was first described and understood.
At first, doctors focused on the type of cells involved, calling it “lymphocytic.” Later, “lymphoblastic” became more common. It highlights the disease’s characteristic immature cells.
Even though the terms are often used in the same way, there are regional differences. In some places, one term is more common than the other. This is due to local medical traditions or historical reasons.
Here’s a table showing these differences:
| Region | Preferred Term | Frequency of Use |
| North America | Acute Lymphoblastic Leukemia (ALL) | High |
| Europe | Acute Lymphoblastic Leukemia (ALL) | High |
| Some Older Literature | Acute Lymphocytic Leukemia | Moderate |
In summary, “Acute Lymphoblastic Leukemia” and “Acute Lymphocytic Leukemia” are the same disease. Knowing the history and regional differences helps in understanding their use. Clear communication is essential for the best care for our patients.
It’s important to know the differences between Acute Lymphoblastic Leukemia (ALL) and other acute leukemias. This knowledge helps in making the right diagnosis and treatment plan. Acute leukemias are cancers that grow fast and affect the blood. Each type has its own unique features that affect treatment and how well a patient does.
ALL and AML are two main types of acute leukemia. The main difference is where the cancer starts. ALL starts in lymphoid cells, while AML starts in myeloid cells. Knowing this is key because it helps decide the best treatment and how likely a patient is to get better.
Key differences between ALL and AML:
| Characteristics | ALL | AML |
| Cell Origin | Lymphoid cells | Myeloid cells |
| Typical Age Group | Children and young adults | Adults, especially older adults |
| Treatment Approach | Chemotherapy, targeted therapy | Chemotherapy, stem cell transplant |
APL is a subtype of AML. It’s known for having too many abnormal promyelocytes. Like ALL, APL needs quick diagnosis and treatment because it’s aggressive. APL is linked to a specific genetic change, t(15;17), which is not seen in ALL.
It’s very important to tell ALL and APL apart. APL responds well to certain treatments like all-trans retinoic acid (ATRA) and arsenic trioxide. These treatments are not used for ALL.
To tell ALL from other acute leukemias, doctors use several tests. These include:
By using these tests together, doctors can accurately diagnose and tell ALL apart from other acute leukemias. This helps in creating a treatment plan that fits the patient’s needs.
The journey to diagnose Acute Lymphoblastic Leukemia (ALL) starts with a detailed medical check-up and special tests. Accurate diagnosis is key to creating a good treatment plan.
The first steps in diagnosing ALL include blood tests and a physical exam. A complete blood count (CBC) checks for abnormal white and red blood cells and platelets. A physical exam looks for swollen lymph nodes, an enlarged spleen or liver, and other signs of leukemia.
A bone marrow biopsy is a key step in diagnosing ALL. It involves taking a bone marrow sample, usually from the hipbone, for analysis. The sample is checked for lymphoblasts, immature white blood cells typical of ALL. Research from the National Center for Biotechnology Information shows that bone marrow analysis is vital for confirming the diagnosis.
After suspecting ALL, we use advanced tests like immunophenotyping and cytogenetic testing. Immunophenotyping looks at the proteins on leukemia cells to identify their type. Cytogenetic testing checks the genetic material of leukemia cells for abnormalities. This information helps predict the prognosis and guide treatment.
By combining these test results, we can accurately diagnose and classify ALL. This allows us to tailor treatment to meet each patient’s unique needs.
Acute Lymphoblastic Leukemia (ALL) treatment is complex. It uses many methods to fight the disease. Each patient gets a treatment plan that fits their needs and risk level.
Chemotherapy is key in treating ALL. It’s given in different phases. The first phase, induction therapy, aims to clear leukemia from the bone marrow and blood.
The consolidation phase then tries to get rid of any remaining leukemia cells. The last phase, maintenance therapy, uses less intense treatment to keep the disease from coming back.
Targeted therapies and immunotherapies are also important in treating ALL. Targeted therapies, like tyrosine kinase inhibitors, target specific genetic flaws in leukemia cells. Immunotherapies, including monoclonal antibodies and CAR-T cell therapy, use the immune system to fight cancer.
One example is CAR-T cell therapy. It has shown great promise in treating ALL that doesn’t respond to other treatments. A study found that CAR-T cell therapy can be a life-saving option for these patients.
Stem cell transplantation is a possible cure for ALL, mainly for those at high risk or with the disease coming back. This involves replacing the bone marrow with healthy stem cells, either from a donor or the patient themselves.
Radiation therapy is not the main treatment for ALL, but it can be used in certain cases. It’s often used to treat leukemia in the brain or other hard-to-reach areas. It’s usually given with chemotherapy or before a stem cell transplant.
As research improves, new hopes for ALL treatment emerge. Understanding the different treatments helps patients make informed choices. This way, they can work towards the best possible outcome.
Acute Lymphoblastic Leukemia (ALL) shows different signs in kids and adults. It’s the top cancer in kids but also hits adults, with unique traits and results.
ALL hits kids most between 2 and 5 years old, with more boys getting it. Adults get it less, but more as they get older, after 60.
| Age Group | Incidence Rate | Risk Factors |
| Children (2-5 years) | Higher incidence | Genetic predisposition, environmental factors |
| Adults (60+ years) | Lower incidence, increasing with age | Previous cancer treatments, genetic mutations |
Kids usually do better with ALL treatment than adults, with better cure rates. Adults, mainly older ones, face more challenges because of health issues and weaker bodies.
“The treatment of ALL in adults is more challenging due to the presence of comorbidities and the decreased tolerance to intensive chemotherapy.”
Adults might need special treatments, like targeted therapies, and changes to their chemotherapy plans.
Both kids and adults who beat ALL need close follow-up for treatment side effects. These can include new cancers, heart problems, and hormone issues.
Knowing these differences is key to giving the best care for ALL patients at any age.
Acute Lymphoblastic Leukemia (ALL) survival rates and prognostic factors depend on many things. These include the patient’s health and the disease itself. It’s important to look at how ALL affects kids and adults differently. We also need to understand what makes treatment work better and how to handle relapse.
Pediatric ALL survival rates have greatly improved. Studies show that over 90% of kids with ALL now survive in developed countries. This success comes from better chemotherapy, care support, and knowing which patients need more intense treatment.
“The cure rate for pediatric ALL has dramatically improved, giving hope to families.” This progress is thanks to research and the developing treatments that match each child’s risk.
Adult ALL is harder to beat than pediatric ALL. While treatments have gotten better, adult survival rates are not as high. Adults often face more challenging diseases and health problems that make treatment harder.
Adults with ALL have a 30% to 50% chance of survival. This depends on age, blood cell count, and genetic markers. An expert says,
“Adult ALL is tough to treat, needing custom and intense treatments.”
Many things can affect how well ALL treatment works. These include age, blood cell count, genetic markers, and how well the body responds to treatment. Some genetic changes, like the Philadelphia chromosome, used to mean a worse outlook. But new treatments have helped these patients more.
Dealing with ALL relapses is a big challenge. Relapse often means a tougher fight ahead. But new treatments and stem cell transplants have helped some patients.
When ALL comes back, doctors use strong chemotherapy. They also check if a stem cell transplant is possible. Researchers are looking into new treatments, like CAR-T cell therapy, to help those with relapsed or resistant ALL.
As we learn more about ALL, survival rates and how we predict them will keep being key. By making treatments fit each patient and using the latest research, we can keep improving care for ALL patients.
Recent years have brought big changes in treating Acute Lymphoblastic Leukemia (ALL). Survival rates have gone up, mainly for kids. Knowing the difference between ALL and other leukemias has helped us create better treatments.
We’ve learned a lot about ALL, including how it works and how it’s different from other leukemias. This knowledge lets us make treatments that fit each patient’s needs. This has led to better results for many.
We’re always working to lead in ALL research and treatment. Our goal is to give our patients the best care possible. We’re committed to top-notch healthcare and support for patients from around the world.
It’s key to know the difference between Acute Lymphoblastic Leukemia and Acute Lymphocytic Leukemia. This shows how important it is to get the right diagnosis and treatment plan. We’re always looking to improve care for ALL patients.
ALL is a blood cancer that affects the bone marrow. It’s caused by the fast growth of immature white blood cells, called lymphoblasts.
ALL and Acute Lymphocytic Leukemia (ALL) are the same disease. The difference is in the names used in different places.
Symptoms include feeling very tired, looking pale, and getting sick often. You might also bruise easily, have swollen lymph nodes, or experience pain in bones or joints.
Doctors use blood tests, bone marrow biopsies, and special tests to diagnose ALL. These tests help identify the leukemia cells.
Treatments include chemotherapy, targeted therapies, and immunotherapies. Sometimes, stem cell transplants or radiation therapy are used, based on the patient’s needs.
ALL is more common in kids and is often more aggressive in adults. Children usually have a better chance of recovery than adults.
Survival rates for ALL have gotten better, thanks to new treatments. The chance of recovery depends on age, genetic factors, and how well the leukemia responds to treatment.
Many people with ALL can be cured with today’s treatments. But the chance of a cure varies based on the patient’s health and the leukemia’s characteristics.
Genetic changes are key in ALL’s development and growth. Certain mutations can affect how well the patient does and guide treatment choices.
Risk factors include genetic predisposition, environmental exposures, and past cancer treatments. But many cases have no known risk factors.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!