Last Updated on November 20, 2025 by Ugurkan Demir
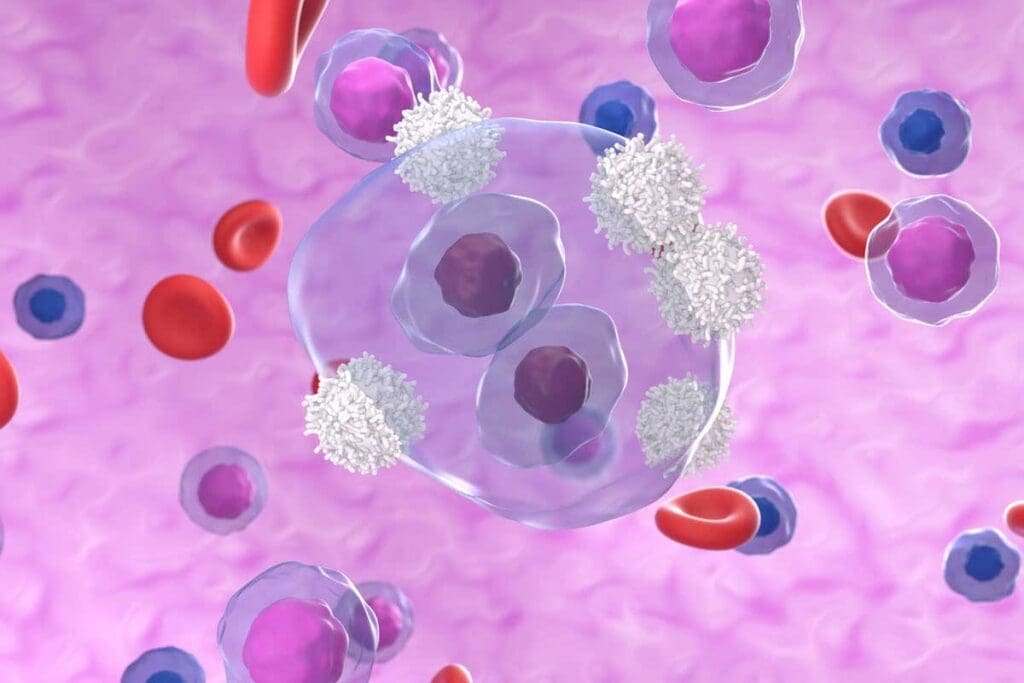
Precursor B-cell acute lymphocytic leukemia (B-ALL) is a fast-growing blood cancer. It starts in the bone marrow. It makes too many immature white blood cells, called lymphoblasts, which can’t fight off infections well.What is precursor B cell acute lymphocytic leukemia (B-ALL)? Learn the key symptoms and serious facts about this type of blood cancer.
At Liv Hospital, we know how complex B-ALL is and how it affects patients.
Key symptoms of B-ALL include fatigue, anemia, and frequent infections. You might also notice easy bruising or bleeding, swollen lymph nodes, bone or joint pain, and unexplained weight loss. Our team is dedicated to top-notch healthcare. We offer full support and guidance to international patients.
To understand B-cell lymphoblastic leukemia, we need to know its definition, characteristics, and how it differs from other leukemias. B-cell lymphoblastic leukemia, or B-ALL, is a cancer that affects the blood and bone marrow.
B-ALL is caused by the uncontrolled growth of immature B cells, called lymphoblasts, in the bone marrow. This growth stops normal blood cells from being made, causing many problems.
Key characteristics of B-ALL include:
B-ALL is the most common type of acute lymphoblastic leukemia (ALL) in children. It makes up about 80% of ALL cases in kids.
The terms “Pre-B ALL” and “B-ALL” are often used the same way, but they mean the same thing. B-ALL is a type of ALL that starts from B-cell precursors. Knowing the terms is important for correct diagnosis and treatment.
Related terms include:
B-ALL is different from other leukemias like acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL) in its cell lineage and how it acts. Knowing these differences is key for choosing the right treatment.
The main differences between B-ALL and other leukemia types are:
| Leukemia Type | Cell Lineage | Clinical Behavior |
| B-ALL | B-cell precursors | Acute, rapid progression |
| AML | Myeloid cells | Acute, rapid progression |
| CLL | Mature B cells | Chronic, slow progression |

To understand B-ALL, we must explore normal B-cell development and how it’s disrupted in leukemia.
B-cells, or B lymphocytes, are vital for our immune system. They grow in the bone marrow through a complex process. Normal B-cell development involves changing immunoglobulin genes and showing specific surface antigens at each stage.
In B-ALL, normal B-cell development goes wrong. This is often due to genetic mutations that mess with cell growth, differentiation, or death. As a result, too many precursor B-cells build up in the bone marrow, causing unchecked proliferation.
Genetic changes are key in B-ALL. These can be chromosomal translocations, mutations in cell signaling and transcription genes, or changes in gene copy numbers. These alterations disrupt normal cell control, helping the disease grow and spread.
The disease comes from genetic changes in precursor B-cells, causing them to grow out of control. Knowing these genetic changes is vital for creating targeted treatments and better patient care.
It’s important to know about B-ALL’s epidemiology and risk factors for early detection and treatment. B-ALL can happen in both kids and adults, with different rates and risk factors.
B-ALL is mostly a childhood cancer, making up 80% of ALL cases in kids. But it also occurs in adults, though less often. Kids between 2 and 5 years old are most likely to get it.
In adults, B-ALL is rarer and often has a poorer outlook than in children. It’s more common in adults over 60.
Several risk factors for B-ALL have been found, including:
Genetics are key in B-ALL development. Some genetic changes make people more likely to get B-ALL. For example, people with Down syndrome are at higher risk because of an extra chromosome 21.
Other genetic syndromes, like ataxia-telangiectasia and Li-Fraumeni syndrome, also raise the risk. Ongoing research aims to find more genetic markers for B-ALL.
Knowing these risk factors and patterns helps doctors spot high-risk individuals. They can then take steps to prevent and diagnose B-ALL early.
It’s important to know the symptoms of B-ALL early for better treatment. We’ll talk about the main signs that B-ALL patients might show. These signs can really affect their life and how well they do with treatment.
The first signs of B-ALL can be hard to spot because they’re not very specific. Common early signs include fatigue, anemia, and frequent infections. These happen because the bone marrow can’t make enough blood cells.
As B-ALL gets worse, patients might experience a lot of physical symptoms. These include swollen lymph nodes, bone or joint pain, and unexplained weight loss. The disease can also cause pale skin and shortness of breath because of anemia.
In some cases, B-ALL can cause the spleen or liver to get bigger. This can be seen during a check-up. These symptoms can really hurt a patient’s quality of life and need to be treated quickly.
B-ALL can also affect different parts of the body. Patients might feel fever, night sweats, and loss of appetite. If it gets really bad, it can even go to the brain, causing headaches, vomiting, and seizures.
It’s key for doctors to know these signs to plan the best treatment. Spotting these symptoms early can really help patients do better.
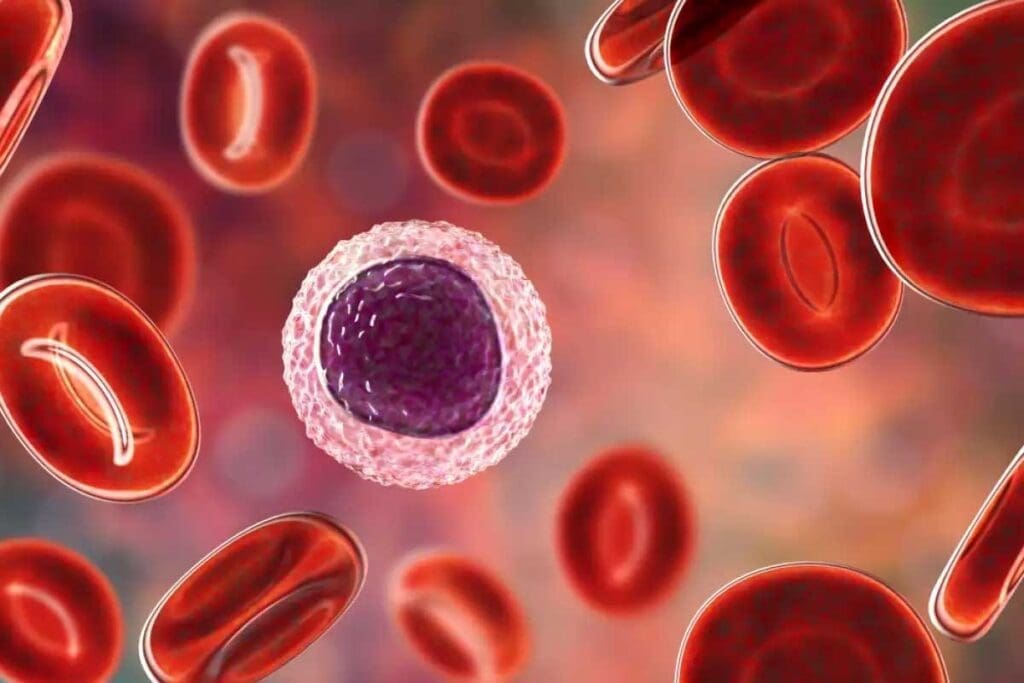
B-ALL affects the bone marrow, causing blood-related symptoms. These symptoms are key for diagnosis and treatment. They happen because the bone marrow can’t make blood cells right.
Anemia is common in B-ALL patients. It’s when there aren’t enough red blood cells. Symptoms of anemia include feeling tired, weak, and pale. You might also have trouble breathing.
We treat anemia with blood transfusions and other care. Keeping an eye on hemoglobin levels helps us know how bad it is and what to do next.
Thrombocytopenia, or low platelet count, is also common in B-ALL. It makes bleeding more likely. You might bruise easily, see small spots on your skin, or have trouble stopping bleeding.
Neutropenia, or low neutrophil count, raises the risk of infections in B-ALL patients. Neutrophils fight infections, and without enough, you’re more likely to get sick.
Symptoms of neutropenia include fever, chills, and infections in places like the skin, lungs, or urinary tract. We stress the need to quickly treat infections in neutropenic patients to avoid serious problems.
“The management of neutropenia involves careful monitoring, prophylactic antibiotics, and granulocyte-colony stimulating factor (G-CSF) therapy to mitigate the risk of infections.”
Understanding and treating these symptoms can greatly improve care and outcomes for B-ALL patients.
Diagnosing B-ALL is a detailed process. It involves blood tests, bone marrow checks, and genetic tests. Getting the diagnosis right is key to the right treatment and better health outcomes.
The first step in diagnosing B-ALL is blood work. A complete blood count (CBC) checks the levels of blood cells. If there’s anemia, thrombocytopenia, or leukocytosis, it might mean leukemia.
The American Cancer Society says, “A diagnosis of acute lymphoblastic leukemia is suspected when there are abnormal cells in the blood or bone marrow.”
A bone marrow examination is a key tool for B-ALL diagnosis. It takes a bone marrow sample for a microscope check. This shows if cancer cells are there and what they look like.
Genetic and molecular tests are vital for B-ALL diagnosis. They find specific genetic issues that guide treatment and predict outcomes.
Immunophenotyping is a lab method to identify cell types. For B-ALL, it confirms the diagnosis by finding B-cell markers on leukemia cells. This is important for telling B-ALL apart from other leukemias.
“Immunophenotyping is essential for the diagnosis and classification of acute lymphoblastic leukemia.”
Healthcare experts use blood work, bone marrow tests, and genetic tests together. This way, they can accurately diagnose Pre-B Cell Acute Lymphoblastic Leukemia. Then, they can plan the best treatment.
Understanding Pre-B Acute Lymphoblastic Leukemia (ALL) is key to knowing how well a patient will do. Doctors look at the leukemia cells and how far the disease has spread. This helps decide the best treatment plan.
The World Health Organization (WHO) has a system to sort Pre-B ALL. It looks at the cells’ shape, what proteins they have, and their genes. This helps doctors tell Pre-B ALL apart from other cancers and find special types that might need different treatments.
Key components of the WHO classification system include:
This system uses different tests to understand the many types of Pre-B ALL.
Pre-B ALL can be divided into genetic subtypes based on certain changes in the genes or chromosomes. These subtypes affect how well a patient might do and what treatments work best.
For example, some genetic subtypes have a better outlook, while others might not respond as well to common treatments.
Some important genetic subtypes are:
Knowing these subtypes helps doctors plan the best treatment for each patient.
Risk stratification is vital in managing Pre-B ALL. It helps doctors find out who is at a higher or lower risk of the cancer coming back. This info guides how intense the treatment should be.
“Risk stratification is based on a combination of clinical features, biological characteristics of the leukemia cells, and the patient’s response to initial therapy.”
Doctors use several factors to determine risk, including:
By accurately figuring out a patient’s risk, doctors can offer more tailored and effective care.
Managing B-ALL needs a detailed treatment plan. This includes standard treatments and new therapies. The right treatment depends on the patient’s age, health, and the leukemia’s genetic makeup.
For B-ALL, treatment often combines chemotherapy and supportive care. Chemotherapy is key, aiming to kill leukemia cells. The treatment goes through several phases: induction, consolidation, and maintenance.
The induction phase aims for remission. Consolidation therapy targets any leftover leukemia cells. Maintenance therapy helps prevent the disease from coming back.
Targeted therapies are a big part of B-ALL treatment. They focus on specific molecules that help leukemia cells grow. Tyrosine kinase inhibitors and monoclonal antibodies are examples used in B-ALL treatment.
Stem cell transplantation is an option for some B-ALL patients, mainly those with high-risk disease or relapse. It replaces the patient’s bone marrow with healthy stem cells. These can be from the patient themselves or a donor.
New treatments are being developed for B-ALL. These include immunotherapies like CAR-T cell therapy. This therapy modifies T cells to attack leukemia cells. Other new treatments include bispecific antibodies and checkpoint inhibitors.
These new therapies are changing how B-ALL is treated. They offer hope to patients and their families.
Treating Precursor B-Cell Acute Lymphocytic Leukemia comes with several challenges. It’s important to know these issues to give the best care. This helps in managing the treatment’s effects.
Complications can happen during or after B-ALL treatment. These include:
Managing these complications is key to better outcomes. Regular checks and support can lessen their impact.
Relapse is a big worry in B-ALL treatment. It happens when leukemia comes back after treatment. Knowing the risks and signs can help catch it early.
Keeping an eye on health long-term is critical for B-ALL patients. Regular check-ups and tests help spot any lasting effects early.
One lasting effect of B-ALL treatment is the risk of new cancers. These cancers happen in people who’ve had B-ALL before. The types and risks vary, and research is ongoing to understand and lower this risk.
Understanding B-ALL treatment’s complications and long-term effects helps healthcare providers. They can offer better care and support. This includes managing treatment’s immediate effects and watching for long-term health issues.
Living with B-cell acute lymphoblastic leukemia (B-ALL) needs a full treatment plan and ongoing support. At Liv Hospital, we aim to give top-notch healthcare to our patients. We make sure they get the best care possible.
Looking ahead, new treatments like targeted therapies and stem cell transplants are making a big difference. Our team is always learning about these new ways to help patients. We make sure our patients get the newest treatments and join clinical trials.
The fight against B-ALL is tough, but with the right care and support, patients can beat it. We keep working to improve our services. We want to make sure our patients get the care and kindness they need.
B-ALL is a blood cancer that affects the bone marrow. It’s caused by the fast growth of immature white blood cells called lymphoblasts.
Symptoms include feeling very tired, anemia, and getting sick often. You might also bruise easily, have swollen lymph nodes, or experience pain in bones or joints. Losing weight without trying can also be a sign.
Doctors start with blood tests and bone marrow exams. They also do genetic and molecular tests. This helps figure out the exact type of leukemia.
B-ALL is unique because it quickly makes immature B lymphoblasts in the bone marrow. It’s the most common ALL in kids.
Treatments include standard care, targeted therapies, and stem cell transplants. There are also new ways to treat it.
Treatment can cause problems, and the disease might come back. Long-term health checks are needed. There’s also a risk of getting another cancer.
Genetics play a part in B-ALL. Knowing this can help find people at higher risk.
Bone marrow tests are key for diagnosing B-ALL. They help see if there are lymphoblasts in the bone marrow.
Yes, B-ALL has genetic subtypes. These affect how the disease will progress and how it’s treated. The WHO classification system helps sort them out.
Yes, targeted therapies are used to treat B-ALL. They offer a more tailored approach to treatment.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!