Last Updated on November 20, 2025 by Ugurkan Demir
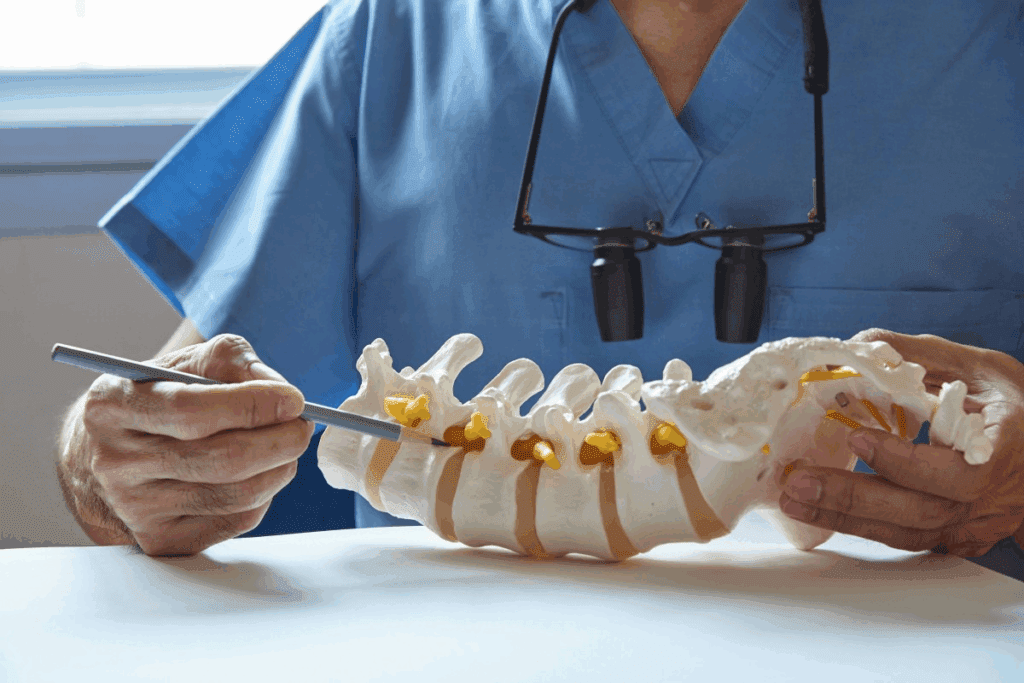
It’s key to know about bone marrow disorders to stay healthy. These issues affect the spongy tissue in bones, which makes blood cells. At Liv Hospital, we offer top-notch care for those with bone marrow diseases. Explore 10 essential bone marrow sickness and diseases, their symptoms, and treatment overview.
Bone marrow disorders include blood cancers like leukemia and other blood issues. We’ll look at what causes them, their signs, and how to treat them. This guide helps you understand your condition and treatment choices.
Bone marrow is a spongy tissue inside our bones, like the hips and thighbones. It’s filled with stem cells. These stem cells turn into red blood cells, white blood cells, and platelets. They are key to our body’s functions.
Bone marrow is vital for making blood cells. It’s where stem cells become different types of blood cells. Research shows that healthy bone marrow is essential for keeping these cells balanced.
The process starts with hematopoietic stem cells. They can renew themselves and turn into all blood cell types. As we age, bone marrow changes, affecting its blood cell production.
Blood cells from bone marrow are divided into three types: red, white, and platelets. Each type has a unique role in keeping us healthy.
Knowing about blood cells and their roles shows how important bone marrow is for our health.
Healthy bone marrow is key to our well-being. It ensures we have enough blood cells for their jobs. For example, enough red blood cells prevent anemia.
It also helps fight infections and respond to injuries. Platelets, for instance, stop too much bleeding.
| Type of Blood Cell | Function | Impact of Dysfunction |
| Red Blood Cells | Carry oxygen throughout the body | Anemia, fatigue |
| White Blood Cells | Fight infections | Increased susceptibility to infections |
| Platelets | Essential for blood clotting | Excessive bleeding, bruising |
In conclusion, bone marrow is vital for our health by making blood cells. Keeping bone marrow healthy is key to avoiding many disorders and staying well.
Bone marrow sickness comes from a mix of genetic, environmental, and autoimmune factors. Knowing these causes helps us find who’s at risk. It also guides us in making better prevention and treatment plans. We’ll look at the different factors that lead to bone marrow disorders.
Genetics is key to bone marrow disorders. Some genetic conditions, like Fanconi anemia and Diamond-Blackfan anemia, raise the risk of bone marrow failure or cancer. We’ll dive into the genetic reasons behind these conditions and what they mean for patient care.
Examples of Genetic Predispositions:
Being exposed to certain toxins and chemicals can increase the risk of bone marrow disorders. We’ll talk about how pesticides, heavy metals, and other harmful substances affect bone marrow health.
Autoimmune diseases, where the body attacks its own cells, can cause bone marrow sickness. Conditions like aplastic anemia might come from autoimmune attacks on bone marrow cells. We’ll look into how these autoimmune reactions affect bone marrow disorders.
Some bone marrow sicknesses have no known cause, called idiopathic. We’ll discuss the challenges of diagnosing and treating these disorders. We’ll also highlight the need for more research into their causes.
| Cause/Risk Factor | Description | Examples |
| Genetic Predispositions | Inherited conditions that increase the risk of bone marrow disorders. | Fanconi anemia, Diamond-Blackfan anemia |
| Environmental Exposures | Exposure to toxins and chemicals can damage bone marrow. | Pesticides, heavy metals |
| Autoimmune Factors | Immune system disorders that attack bone marrow cells. | Aplastic anemia |
| Idiopathic Causes | Unknown causes of bone marrow sickness. | N/A |
Aplastic anemia is a rare and serious condition. It happens when the bone marrow can’t make blood cells. This leads to fewer red blood cells, white blood cells, and platelets. Symptoms include tiredness, infections, and bleeding.
The bone marrow fails in aplastic anemia for different reasons. Damage to stem cells is common. This damage can come from toxins, medicines, or autoimmune diseases. Sometimes, the cause is unknown, called idiopathic aplastic anemia.
Symptoms of aplastic anemia include feeling very tired, weak, and short of breath. People might also get infections easily. Bleeding gums, nosebleeds, and long bleeding times are other signs.
To diagnose aplastic anemia, doctors use blood tests and a bone marrow biopsy. Blood tests show low blood cell counts. A bone marrow biopsy shows how much damage there is.
Treatment for aplastic anemia includes medicines to calm the immune system and bone marrow transplants. Supportive care helps manage symptoms. The outcome depends on how well the treatment works and the cause of the condition.
| Diagnostic Criteria | Treatment Options | Prognosis |
| Blood tests showing low blood cell counts | Immunosuppressive therapy | Variable, depending on response to treatment |
| Bone marrow biopsy showing aplastic marrow | Bone marrow transplantation | Improved with successful transplantation |
| Exclusion of other causes of bone marrow failure | Supportive care (transfusions, antibiotics) | Dependent on the underlying cause and treatment response |
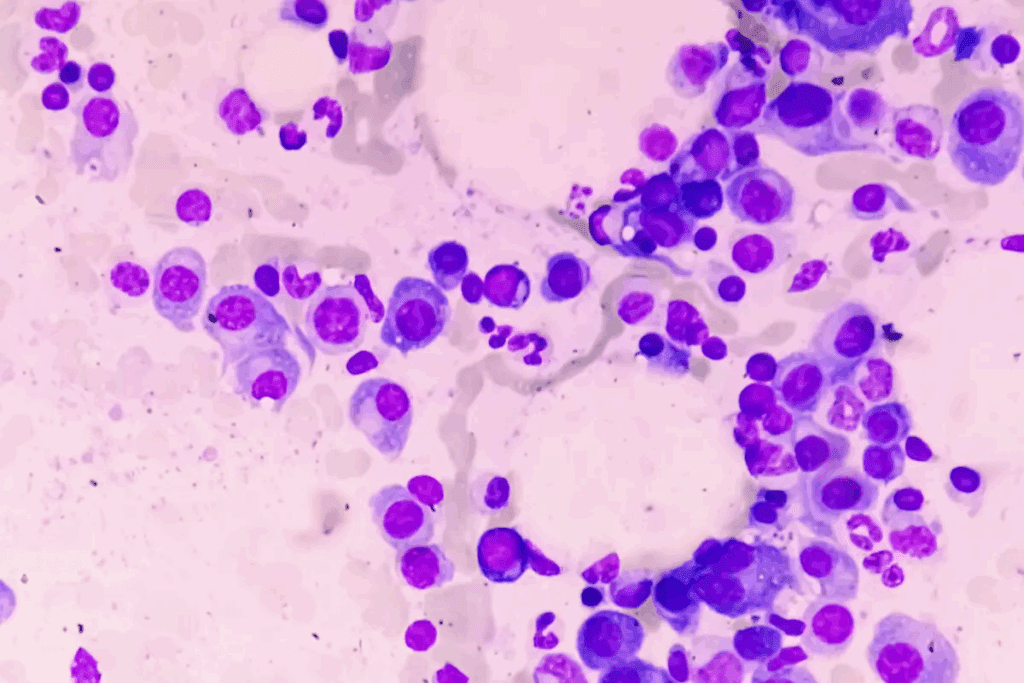
Leukemia is a complex group of blood cancers that start in the bone marrow. It disrupts normal blood cell production. This leads to too many abnormal white blood cells, which are key to our immune system.
There are many types of leukemia. Modern treatments have greatly improved how we fight these diseases.
Acute Myeloid Leukemia (AML) quickly grows in the bone marrow. It affects the myeloid cells. Treatment for AML often includes strong chemotherapy and sometimes bone marrow transplantation.
Symptoms of AML include feeling very tired, getting sick easily, and bleeding or bruising easily. Doctors use bone marrow biopsies and genetic tests to diagnose it.
Acute Lymphoblastic Leukemia (ALL) is a fast-growing leukemia that affects lymphoid cells. It’s more common in kids, but it can happen in adults, too. ALL treatment usually involves chemotherapy and targeted therapy.
Children with ALL have a high cure rate thanks to modern treatments. Adults also see better outcomes with treatments like stem cell transplants.
Chronic Lymphocytic Leukemia (CLL) grows slowly and affects lymphoid cells. It’s marked by the buildup of mature lymphocytes in the blood and bone marrow. For advanced cases, CLL treatment may include targeted therapy or immunotherapy.
Doctors watch CLL patients closely for signs of the disease getting worse. Treatment plans are made based on the patient’s risk and health.
Today’s leukemia treatments offer new hope. They include targeted therapies, immunotherapies, and CAR-T cell therapy. The right treatment depends on the leukemia type, the patient’s health, and genetic factors.
We’re seeing a big change in how we treat leukemia. It’s moving towards personalized medicine and precision oncology. Clinical trials are finding new ways to help patients live better lives.
In conclusion, leukemia is a diverse group of cancers needing specific treatments. By understanding each type and using modern treatments, we can greatly improve patient outcomes and quality of life.
Myelodysplastic syndromes (MDS) are complex disorders where the bone marrow can’t make healthy blood cells. This leads to ineffective hematopoiesis, causing anemia, neutropenia, and thrombocytopenia.
The World Health Organization (WHO) and the International Prognostic Scoring System (IPSS) have updated MDS classification. It’s based on bone marrow features, genetic changes, and blast percentages.
The main types of MDS include:
Symptoms of MDS vary and depend on the type of cytopenia. Common signs are fatigue, infections, and bleeding. Disease progression can be slow or fast, sometimes turning into AML.
Progression is influenced by genetic mutations, blast percentages, and cytogenetic abnormalities.
Risk assessment is key for MDS prognosis and treatment planning. The IPSS and IPSS-R categorize patients based on blast percentages, cytogenetics, and cytopenias.
Knowing the prognosis helps in making treatment decisions and when to consider aggressive treatments.
Treatment for MDS varies based on risk, age, and health. Options include supportive care, hypomethylating agents, and stem cell transplantation.
Supportive care improves quality of life. Hypomethylating agents can slow disease progression by reducing DNA methylation.
Allogeneic stem cell transplantation can cure MDS but comes with risks. It’s a serious option that needs careful thought.
The Philadelphia chromosome is a key feature of Chronic Myelogenous Leukemia (CML). It comes from a swap between chromosomes 9 and 22. This swap creates a BCR-ABL fusion gene. This gene is at the heart of CML’s growth, spread, and treatment choices.
In CML, the Philadelphia chromosome is found in over 95% of patients. The BCR-ABL fusion gene makes a tyrosine kinase that never stops working. This leads to too many leukemic cells. This genetic change is what makes CML grow and spread.
CML goes through three stages: chronic, accelerated, and blast. The chronic phase is usually mild or without symptoms. The accelerated and blast phases get worse and are harder to treat. Knowing these stages is key to managing CML well.
| Phase | Characteristics | Typical Symptoms |
| Chronic | Often asymptomatic, mild symptoms | Fatigue, weight loss, mild leukocytosis |
| Accelerated | Increasing severity, resistance to treatment | More pronounced cytopenias, increasing blasts |
| Blast | Aggressive disease, blast crisis | Severe cytopenias, high blast count, organ infiltration |
Tyrosine kinase inhibitors (TKIs) have changed how we treat CML. TKIs target the BCR-ABL tyrosine kinase. This has greatly improved patient results. We will look at the different TKIs and their role in targeted therapy.
Managing CML well means watching the disease closely over time. It’s important to check BCR-ABL transcript levels often. This helps adjust treatments and keep patients healthy.
Polycythemia vera is a condition where the body makes too many red blood cells. This happens because of abnormal growth in the bone marrow. It also leads to an overproduction of white blood cells and platelets.
Many people with polycythemia vera have a specific gene mutation. This mutation, JAK2V617F, makes the body’s cells grow and live longer than they should. This is because of a problem in the JAK-STAT signaling pathway.
This mutation is key in making too many red blood cells. Knowing about this helps doctors find better treatments.
People with polycythemia vera might feel:
These symptoms come from the blood being too thick. It also increases the risk of blood clots. Treating these problems is very important.
To diagnose polycythemia vera, doctors look at several things. They check:
These signs help doctors tell polycythemia vera apart from other conditions.
Treatment for polycythemia vera aims to prevent blood clots and manage symptoms. Doctors use:
Keeping a close eye on treatment and making changes as needed is key to managing polycythemia vera.
Essential thrombocythemia is a condition where the body makes too many platelets. This can cause serious health problems, like blood clots. We will look at what causes this, its symptoms, how doctors diagnose it, and how to treat it.
The cause of essential thrombocythemia is linked to certain gene mutations. These include JAK2, MPL, and CALR. These genes help control how platelets are made in the bone marrow. Knowing this helps doctors diagnose and treat the condition.
Genetic testing is key in finding these mutations. It helps doctors understand the risk of blood clots.
People with essential thrombocythemia may have headaches, dizziness, or a burning feeling in their hands and feet. The biggest worry is blood clots, which can lead to heart problems.
Having too many platelets can cause thrombotic complications. This includes blood clots in the legs, lungs, or brain. It’s important to manage this risk.
To diagnose essential thrombocythemia, doctors do blood tests, bone marrow biopsies, and genetic tests. They look for specific mutations and rule out other conditions.
A detailed check is needed to make sure it’s essential thrombocythemia and not something else.
Treatment plans for essential thrombocythemia depend on the risk of blood clots. Low-risk patients might just take low-dose aspirin and get regular check-ups. High-risk patients might need stronger treatments to lower platelet counts.
Doctors use a personalized approach to treat essential thrombocythemia. This aims to reduce the risk of blood clots while considering the treatment’s side effects.
Inherited bone marrow failure syndromes are a group of conditions where the bone marrow can’t make enough blood cells. These conditions are often caused by genes and can cause health problems like anemia and infections. They also increase the risk of cancer.
We will look at several key syndromes, like Fanconi anemia, Diamond-Blackfan anemia, and GATA2 deficiency. We’ll talk about their genetic and clinical features.
Fanconi anemia is a rare genetic disorder. It causes bone marrow failure, birth defects, and a higher risk of cancer. It’s caused by DNA repair gene mutations, leading to unstable chromosomes.
Clinical manifestations include aplastic anemia, leukemia, and physical abnormalities. Doctors diagnose it through genetic tests and chromosomal breakage tests.
Diamond-Blackfan anemia is a bone marrow failure syndrome. It’s caused by problems with ribosomes, which are key to making blood cells. It’s often linked to mutations in genes that code for ribosomal proteins.
To diagnose Diamond-Blackfan anemia, doctors use clinical evaluation, bone marrow tests, and genetic tests. They look for mutations in ribosomal protein genes.
GATA2 deficiency is caused by GATA2 gene mutations. It leads to blood and immune system problems. People with this condition are at risk of myelodysplastic syndrome, leukemia, and severe infections.
“GATA2 deficiency highlights the complex interplay between hematopoiesis and immune function, underscoring the need for comprehensive care in managing these patients.” – Hematologist
Genetic testing is key for diagnosing these syndromes. It confirms the diagnosis and finds carriers in families.
Family counseling is vital for support and guidance. It covers genetic implications, family risks, and family planning options.
Understanding the genetic basis helps manage these syndromes. It also helps counsel families effectively.
Recent years have brought big changes in diagnosing and treating bone marrow disorders. This has led to better results for patients. We’ve looked at diseases like aplastic anemia, leukemia, and myelodysplastic syndromes. We’ve talked about what causes them, their symptoms, and how to treat them.
Thanks to new diagnostic tools, doctors can spot these conditions faster and more accurately. Treatments have also gotten better, with new therapies giving patients hope.
Managing bone marrow diseases well needs a team effort. It involves using the latest research and medical breakthroughs. We’re seeing better care for patients because of this ongoing work.
Looking ahead, we must keep focusing on top-notch healthcare for all patients. This includes those from around the world. By doing this, we make sure patients get the best care for their bone marrow issues.
Bone marrow disorders affect the bone marrow’s ability to make healthy blood cells. This can cause anemia, infections, and bleeding problems.
Bone marrow disease includes conditions like aplastic anemia, leukemia, and myelodysplastic syndromes. These affect how the bone marrow makes blood cells.
Causes include genetic factors, environmental exposures, and autoimmune issues. Sometimes, the cause is unknown.
Aplastic anemia makes the bone marrow fail to produce blood cells. This leads to fatigue, infections, and bleeding. It can be caused by toxins and autoimmune disorders.
Leukemia is a blood and bone marrow cancer. There are Acute Myeloid Leukemia (AML), Acute Lymphoblastic Leukemia (ALL), and Chronic Lymphocytic Leukemia (CLL). Each has its own treatment.
Myelodysplastic syndromes (MDS) are disorders with poorly formed blood cells. They can lead to more serious conditions like AML.
Chronic Myelogenous Leukemia (CML) is a cancer of white blood cells. It’s marked by the Philadelphia chromosome. It’s treated with tyrosine kinase inhibitors.
Polycythemia vera causes the bone marrow to make too many red blood cells. This makes blood thick and can lead to blood clots.
Essential thrombocythemia makes too many platelets. This can cause blood clots. Treatment aims to lower platelet counts and prevent clots.
Inherited bone marrow failure syndromes are genetic disorders. They affect the bone marrow’s blood cell production. Examples include Fanconi anemia and Diamond-Blackfan anemia.
Diagnosing bone marrow disorders involves blood tests, bone marrow biopsies, and genetic testing. These help find the cause and extent of the condition.
Treatments vary by condition. They include medications, blood transfusions, bone marrow transplants, and therapies to manage symptoms and improve life quality.
Cure chances vary by disorder and treatment. Some, like certain leukemias, aim for a cure. Others need ongoing management.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!