The discovery of induced pluripotent stem cells has changed the game in medical research. It opens up new ways to study diseases, find new medicines, and fix damaged tissues.
By changing adult cells into a special state, induced pluripotent stem cells (iPSCs) can turn into many different cell types. This makes them a great tool for scientists.
This technology could change how we understand human health and sickness. It could lead to treatments made just for you.
Key Takeaways
- Understanding induced pluripotent stem cells is key for moving forward in medical research.
- iPSCs are a promising tool for studying diseases and finding new medicines.
- This technology could lead to treatments made just for you.
- By changing adult cells into a special state, iPSCs can become many different cell types.
- Induced pluripotent stem cells are changing the field of regenerative medicine.
The Science Behind Induced Pluripotent Stem Cells
Understandinginducedpluripotent stem cells (iPSCs) is key to seeing their medical promise. These cells are made from adult cells, like skin or blood. They are reprogrammed to be like embryonic stem cells.
Definition and Basic Concepts
iPSCs can turn into almost any cell in the body. This makes them very useful for research and treatments. They are made by adding special genes, called the Yamanaka factors, to adult cells. These genes were found by Shinya Yamanaka in 2006 .
“The discovery of induced pluripotent stem cells has changed stem cell biology,” say researchers. This breakthrough lets scientists study cells and diseases in new ways.
Historical Development of iPSC Technology
The journey of iPSC technology started in 2006 with Shinya Yamanaka’s team. They showed mouse cells could be turned into pluripotent cells with the Yamanaka factors. Then, in 2007, human cells were reprogrammed too. Ever after, iPSC technology has grown, getting better at reprogramming and safer.
- The initial discovery of iPSCs by Yamanaka et al. in 2006.
- The first successful reprogramming of human cells in 2007.
- Ongoing improvements in reprogramming techniques and efficiency.
The creation of iPSC technology is seen as a big step forward. It opens doors for regenerative medicine, studying diseases, and finding new drugs. As research keeps improving, iPSCs could lead to more treatments.
Cell Types Used for IPS Induced Reprogramming
Creating iPSCs begins with selecting the appropriate cell type. The choice is key because it affects how well the iPSCs work and what they can do.
Fibroblasts as Common Starting Cells
Fibroblasts are a top pick for making iPSCs. They’re easy to get from skin samples. This makes them a favorite in labs because they’re simple to work with.
Fibroblast-derived iPSCs are very good at what they do. They’re great for studying diseases and finding new medicines.
Alternative Cell Sources
While fibroblasts are popular, other cells like PBMCs are also used. PBMCs are special because they can be taken from blood easily. This makes getting them less painful.
Alternative cell sources like PBMCs are better because they’re easier to get. They might also be less likely to have genetic problems than cells taken from more invasive places.
Selection Criteria for Source Cells
When choosing cells for iPSC making, several things matter. These include how easy they are to get, how well they can be reprogrammed, and if they stay genetically stable.
| Cell Type | Accessibility | Reprogramming Efficiency |
| Fibroblasts | High | Moderate to High |
| PBMCs | High | Moderate |
Knowing what makes each cell type special is key. It helps make better iPSCs and ensures they’re of high quality.
Methods of Creating Induced Pluripotent Stem Cells
Making iPSCs is a complex process. It uses different reprogramming strategies, like viral and non-viral methods. The choice of method depends on the starting cells, how efficient you want the reprogramming to be, and what you plan to use the iPSCs for.
Viral Vector-Based Reprogramming
Viral vectors are often used to turn somatic cells into iPSCs. This method uses viruses to carry reprogramming factors like Oct4, Sox2, Klf4, and c-Myc into cells. Viruses like lentiviruses or retroviruses are used for this. This way, the factors are delivered efficiently, making the reprogramming process more effective than some non-viral methods.
Advantages: High efficiency, well-established protocols.
Limitations: Risk of insertional mutagenesis, possible viral vector-related toxicity.
Non-Viral Reprogramming Methods
To avoid the risks of viral vectors, scientists have come up with non-viral methods. These include plasmids, episomal vectors, and recombinant proteins to deliver reprogramming factors. Non-viral methods are safer and lower the risk of genetic changes and mutations.
Key benefits: Improved safety profile, reduced risk of insertional mutagenesis.
Challenges: Generally lower efficiency compared to viral vector-based methods, requires optimization.
Latest Technological Advances
New technologies have improved reprogramming efficiency, safety, and scalability. CRISPR/Cas9 genome editing has been used to make reprogramming more precise and reduce unwanted changes. Also, synthetic mRNA and microRNA-based reprogramming methods are showing promise.
- CRISPR/Cas9 genome editing for precise modifications
- Synthetic mRNA and microRNA-based reprogramming
- Small molecule-based approaches to enhance reprogramming efficiency
These advancements are making it easier and safer to create iPSCs. This is key for their use in regenerative medicine and disease modeling.
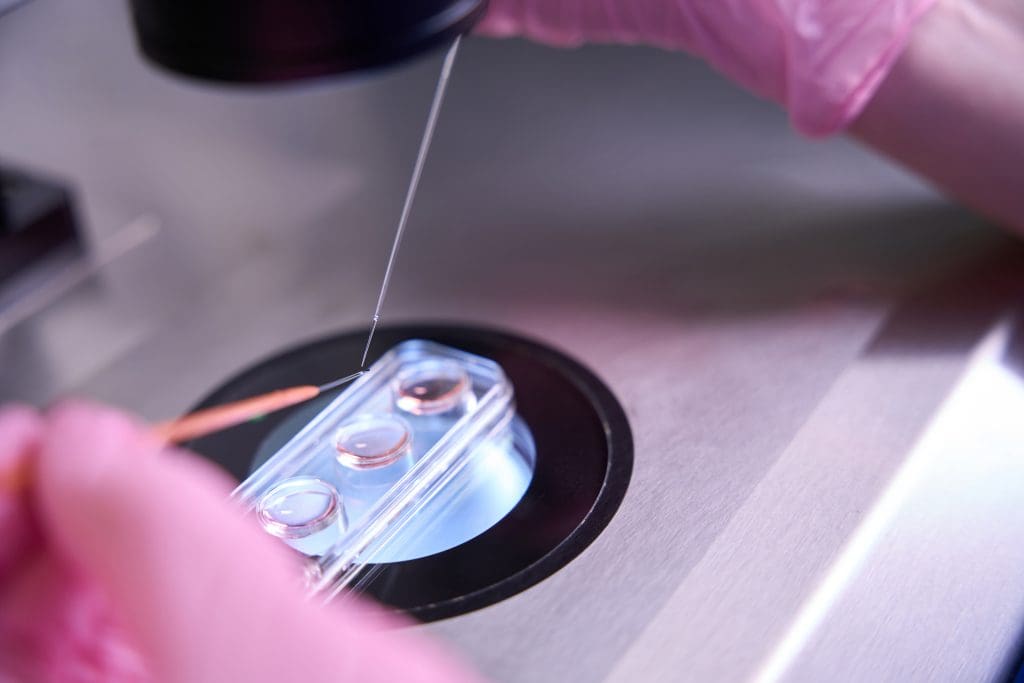
Step-by-Step Process of IPS Cell Generation
Creating iPSCs is a detailed process. It includes choosing cells, adding genes, and setting up specific culture conditions. This complex process changes somatic cells into a pluripotent state.
Cell Selection and Preparation
The first step is picking and preparing the starting cells. Fibroblasts are often chosen because they are easy to reprogram. But,peripheral blood cells and keratinocytes can also be used.
The right cells should be easy to get and reprogram. A study in Nature shows that different cells have different reprogramming success rates (Source: First source).
| Cell Type | Reprogramming Efficiency | Advantages |
| Fibroblasts | High | Ease of access, well-established reprogramming protocols |
| Peripheral Blood Cells | Moderate | Minimally invasive collection method, autologous use possible |
| Keratinocytes | Low | Easy to culture, good for skin-related therapies |
Gene Delivery Systems
Getting the reprogramming factors into the cells is key. Many methods can be used, like viral vectors and non-viral methods. Viruses are efficient but can cause problems.
“The use of viral vectors for reprogramming has been a significant advancement, but safety concerns necessitate the exploration of alternative methods.”
Non-viral methods, like episomal vectors and mRNA delivery, are safer but less efficient.
Culture Conditions and Media Requirements
After adding genes, cells are grown in special conditions. The media includes basic fibroblast growth factor (bFGF) to help them become pluripotent. The right conditions and media are important for making iPSCs.
Verification and Characterization
When colonies look like ESCs, they are isolated and grown. They are checked for pluripotency markers like OCT4 and NANOG. They also see if the cells can become the three germ layers.
Checking iPSCs is key to make sure they are good for use in ips induced therapy and ips induced research. This helps understand their role in regenerative medicine and disease modeling.
Challenges in IPS Cell Production
IPS cell technology has made big strides, but it’s not without its hurdles. The journey to create these cells is complex. It faces many challenges, like making the process more efficient, ensuring safety, and maintaining quality.
Efficiency Issues
One big challenge is making the reprogramming process more efficient. The reprogramming efficiency can change a lot. It depends on the method, the starting cells, and the genes used. Making IPS cells more efficiently is key for research and treatments.
To boost efficiency, scientists are trying new things. They’re looking at better ways to mix the reprogramming factors and how to deliver them. For example, using non-integrating vectors can lower the risk of genetic problems while keeping efficiency high.
Safety Concerns
Safety is a top worry in IPS cell production. There’s a fear of ips side effects and the chance of tumors. The use of viral vectors can lead to genetic issues, making safety a big concern for using IPS cells in treatments.
To tackle these risks, scientists are working on safer ways to make IPS cells. They’re looking into using small molecules instead of viral vectors. Also, it’s vital to check and control the quality of IPS cells. This ensures they’re safe for research and treatments.
Quality Control Measures
It’s essential to ensure IPS cells are of high quality. This means testing them for ips induced effects on cell behavior and genetic stability. They should also be able to turn into the right cell types. Quality checks also look for any ips induced theory-related problems, like odd gene expression.
Having strong quality control is key for using IPS cells in medicine. It involves standard ways to check and confirm the safety and effectiveness of IPS cells.
In summary, while IPS cell technology is promising, we must overcome its challenges. By focusing on making the process more efficient, ensuring safety, and keeping quality high, we can unlock the full power of IPS cells. This will lead to major medical breakthroughs.
Applications of Induced Pluripotent Stem Cells in Medicine
iPSCs are a powerful tool in medicine. They help researchers model diseases, find new drugs, and create regenerative therapies. Their ability to become different cell types makes them very useful for medical research and treatments.
Disease Modeling
Disease modeling is a key use of iPSCs. By changing cells from patients with certain diseases, researchers can make patient-specific cell models. These models help understand diseases better and create treatments that fit each patient.
- Modeling genetic disorders such as cystic fibrosis and muscular dystrophy
- Studying complex diseases like Alzheimer’s and Parkinson’s
- Understanding the progression of diseases at the cellular level
Drug Discovery and Testing
iPSCs are also used in drug discovery and testing. They help researchers test drugs in cells that are relevant to specific diseases. This makes it easier and faster to find effective drugs.
Some key benefits include:
- High-throughput screening: Allows the testing of many compounds against specific disease models.
- Personalized medicine: Tests drugs on patient-specific cells, helping predict how patients will respond.
- Reduced reliance on animal models: iPSC-based models can reduce the need for animal testing, aligning with ethical considerations.
Regenerative Medicine
Regenerative medicine is another area where iPSCs are making a big difference. They can create healthy cells to replace damaged or diseased ones. This offers new hope for treating many conditions.
Examples of regenerative applications include:
- Repairing damaged heart tissue after a heart attack
- Treating degenerative diseases such as macular degeneration
- Replacing damaged cells in the spinal cord to treat paralysis
In conclusion, iPSCs have a huge role in advancing medical research and treatment. Their use in disease modeling, drug discovery, and regenerative medicine is leading to new therapies and better patient outcomes.
IPS Induced Technology in Personalized Medicine
IPS induced technology is changing personalized medicine. It uses Induced Pluripotent Stem Cells (iPSCs) to create cells specific to each patient. This is a big step forward in medical science.
Patient-Specific Therapies
One key benefit of IPS technology is making patient-specific iPSCs. These cells can be turned into different types of cells for treatments. This could lead to new ways to treat diseases.
Immunocompatibility Advantages
Using patient-specific iPSCs also helps with immune issues. These cells come from the patient, so there’s less chance of the body rejecting them. This is a big plus for transplant treatments.
Benefits of Immunocompatibility:
- Reduced risk of immune rejection
- Improved graft survival rates
- Enhanced patient outcomes
Precision Medicine Applications
IPS technology is also key in precision medicine. It lets researchers create iPSCs from patients with certain genetic conditions. This helps them study diseases and test treatments in a real-life setting.
| Disease | iPSC Application | Potential Outcome |
| Cardiovascular Disease | Modeling with patient-specific iPSCs | Better understanding of disease mechanisms |
| Neurodegenerative Disorders | Drug testing using iPSC-derived neurons | Identification of effective treatments |
| Genetic Disorders | Gene correction and therapy development | Potential cure or significant disease management |
The role of IPS technology in personalized medicine is huge. As research improves, we’ll see more patient-specific treatments and better disease management. This opens up new ways to treat many diseases.
Current Clinical Trials Using iPSCs
Researchers are now using iPSCs in clinical trials for regenerative medicine. These cells can turn into many different types of cells. This makes them a great tool for treating many diseases.
Macular Degeneration Treatment
One big area of research is treating macular degeneration. Scientists are testing if iPSCs can help restore vision in patients. The ips induced treatment might fix the root causes of this condition.
Parkinson’s Disease Therapy
iPSCs are also being studied for Parkinson’s disease. Researchers aim to turn these cells into dopamine-making neurons. These neurons could help patients with Parkinson’s by easing their symptoms. This ips induced therapy could be a game-changer for the disease.
Other Promising Clinical Applications
iPSCs are also being looked at for other diseases. These include heart disease, diabetes, and spinal cord injuries. Their ability to adapt makes them a strong candidate for treating many conditions.
The ongoing trials with iPSCs are a big leap in regenerative medicine. As research continues, we’ll see more ips induced treatment options for various diseases.
Commercial Development and Industry Applications of iPSCs
The biotech sector is seeing a big jump in the use of iPSC technology. This is because it holds great promise in treating many diseases. As research gets better, it’s clear that iPSCs could change healthcare a lot.
Biotech Companies Specializing in iPSC Technology
Many biotech companies are leading in iPSC research and development. They are putting a lot of money into this technology. They see its big chance for ips induced prevention and treating many conditions.
- Company A: Focused on developing iPSC-based therapies for degenerative diseases.
- Company B: Specializing in the use of iPSCs for drug discovery and testing.
- Company C: Working on iPSC-derived cell therapies for regenerative medicine.
Manufacturing Challenges and Solutions
Even with the promise of iPSC technology, there are big challenges in making it. These include making sure the quality and safety of iPSC products are good. Also, making more of these products to meet demand is hard.
| Challenge | Solution |
| Quality Control | Implementing stringent quality control measures |
| Scalability | Developing more efficient manufacturing processes |
| Safety Concerns | Enhancing safety protocols for iPSC-derived therapies |
Market Growth and Investment Trends
The market for iPSC technology is growing fast. This is because more money is going into research and development. There’s a big push towards ips induced diagnosis and personalized medicine.
As the industry keeps growing, we’ll see big steps forward in using iPSC technology. This includes new treatments and diagnostic tools. The chance for ips induced treatments to meet medical needs is huge.
Ethical Considerations of IPS Technology
IPS technology has changed how we do stem cell research. It helps solve some big ethical problems. IPSCs, or Induced Pluripotent Stem Cells, are a promising alternative to embryonic stem cells. This solves many ethical issues.
Advantages Over Embryonic Stem Cell Research
IPS technology has a big ethical plus. It bypasses the need for embryonic stem cells. This is a big deal because using human embryos for research is very controversial. IPSCs are made by turning adult cells into a pluripotent state. This avoids the ethical problems of using embryos.
Using IPSCs for research and treatments is seen as more ethical. It doesn’t harm embryos. This is key for ips induced therapy, where treatments must be both effective and ethical.
Remaining Ethical Concerns
Even with its benefits, IPS technology has its own ethical worries. There are fears about the misuse of IPSCs, like cloning or making human gametes. There are also worries about the genetic stability and safety of IPSCs, which is critical for treatments.
The ips induced effect on the genome and the chance of unintended effects during reprogramming need careful thought. Making sure IPSCs are safe and work well for treatments is very important.
Regulatory Frameworks
To tackle the ethical issues of IPS technology, rules have been made. These rules help make sure IPSCs are used right and research is done ethically.
Groups like the FDA in the U.S. have set guidelines for using IPSCs in research and treatments. These guidelines cover things like donor consent, cell characterization, and safety protocols. They offer a clear way to use IPSCs ethically.
Limitations and Risks of Induced Pluripotent Stem Cells
iPSCs have a lot of promise for medical treatments. But, they also come with some big challenges and risks. Making and using iPSCs is a complex task. It involves changing adult cells into a state similar to embryonic stem cells.
Genetic Instability
One big worry with iPSCs is genetic instability. The process of changing adult cells into iPSCs can introduce genetic mutations. This can lead to abnormal cell behavior.
Studies have found that iPSCs can get genetic changes during the reprogramming and culturing process. This genetic instability is a big problem. It can affect how safe and effective iPSC-based treatments are, potentially causing ips syndrome.
- Genetic mutations can occur during reprogramming.
- Culturing conditions can contribute to genetic instability.
- Monitoring genetic integrity is essential for iPSC applications.
Tumorigenic Potencial
iPSCs can sometimes form tumors, called teratomas, when put into animals. This tumorigenic potencial is a big risk for using iPSCs in treatments. It could lead to ips side effects in patients. Researchers are trying to find ways to reduce this risk by improving how iPSCs are made and screened before use.
“The tumorigenic potencial of iPSCs is a major concern that needs to be addressed before these cells can be used in clinical applications.”
Expert in Stem Cell Research
Technical Challenges
Making iPSCs is a complex task that needs advanced equipment and skills. The success of reprogramming can vary a lot. It depends on the method used and the type of cells being reprogrammed. Making iPSC generation more efficient and consistent is key for large-scale use, including ips treatment development.
- Optimizing reprogramming protocols.
- Standardizing culturing conditions.
- Developing scalable production methods.
Cost and Scalability Issues
Right now, making and testing iPSCs is very expensive. This makes it hard to produce them on a large scale for treatments. Lowering costs and making production more efficient is vital. This will help make iPSC-based treatments more affordable for more people, reducing the ips causes of high treatment costs.
In conclusion, iPSCs have a lot of promise for medical treatments. But, we need to understand and tackle their challenges and risks. By working on these issues, researchers can make iPSC-based treatments safer and more effective. This will help improve ips diagnosis and ips prevention strategies.
Conclusion: The Transformative IPSC Technology
Induced pluripotent stem cells (iPSCs) have changed the game in biomedical research and medicine. IPS induced technology is set to change how we tackle disease modeling, drug discovery, and regenerative medicine. By turning adult cells into a pluripotent state, researchers can make iPSC-derived cells that can become many different cell types, like heart cells.
This technology is a big step towards personalized medicine. It lets doctors create treatments that fit each patient’s needs. As research gets better, IPS induced technology will open up new areas in biomedicine.
IPS induced technology is on the verge of a big leap in medicine. As scientists get better at making and changing iPSCs, we’ll see huge improvements in health. The growth of iPSC technology is exciting for learning more about diseases and finding new treatments.
FAQ
What are the commercial development and industry applications of iPSCs?
The use of iPSCs in business is growing fast. Many biotech companies are working with iPSCs. They aim to make new treatments and improve how these cells are made.
What is the current status of clinical trials using iPSCs?
Clinical trials with iPSCs are underway. They’re looking at treating diseases like macular degeneration and Parkinson’s. These trials check if iPSC-based treatments are safe and work well in people.
What are the limitations and risks associated with iPSCs?
There are risks with iPSCs. They can have genetic problems and might grow into tumors. There are also technical and cost issues. These need to be managed to use iPSCs safely.
What is the role of IPS induced technology in personalized medicine?
IPS technology is changing personalized medicine. It lets doctors create cells just for a patient. This makes treatments more precise and safer.
What are the challenges in IPS cell production?
Making iPSCs can be tricky. It’s not always efficient, and there are safety worries. There’s also a need to ensure the quality of the cells.
What are the possible uses of induced pluripotent stem cells?
iPSCs can be used in many ways. They help in studying diseases, testing drugs, and in regenerative medicine. They can model diseases, test drug safety, and even replace damaged cells.
What are Yamanaka factors?
Yamanaka factors are four genes. They are Oct4, Sox2, Klf4, and c-Myc. Shinya Yamanaka found them to be key in turning adult cells into iPSCs.
How are induced pluripotent stem cells made?
To make iPSCs, adult cells like fibroblasts are changed. This is done by adding special genes called Yamanaka factors. These genes help the cells become pluripotent, allowing them to become different types of cells.
What are induced pluripotent stem cells (iPSCs)?
Induced pluripotent stem cells (iPSCs) are made from adult cells. They can turn into almost any cell in the body. This makes them very useful for research and could help in treating diseases.