Last Updated on November 18, 2025 by Ugurkan Demir
Degenerative joint disease, also known as osteoarthritis knee, affects nearly 365 million people worldwide. It is a major cause of disability.
We know how much this condition affects daily life. At Liv Hospital, we’re dedicated to helping. We offer advanced treatments for knee joint degeneration and related issues.
We aim to give people the tools to prevent and manage this common condition. In this article, we’ll look at the 7 main causes of degenerative joint disease knee. We’ll also share effective ways to prevent and manage it.
It’s important to know about osteoarthritis knee to improve your life quality. This condition, also known as degenerative joint disease, affects the knee. It causes pain, stiffness, and makes it hard to move.
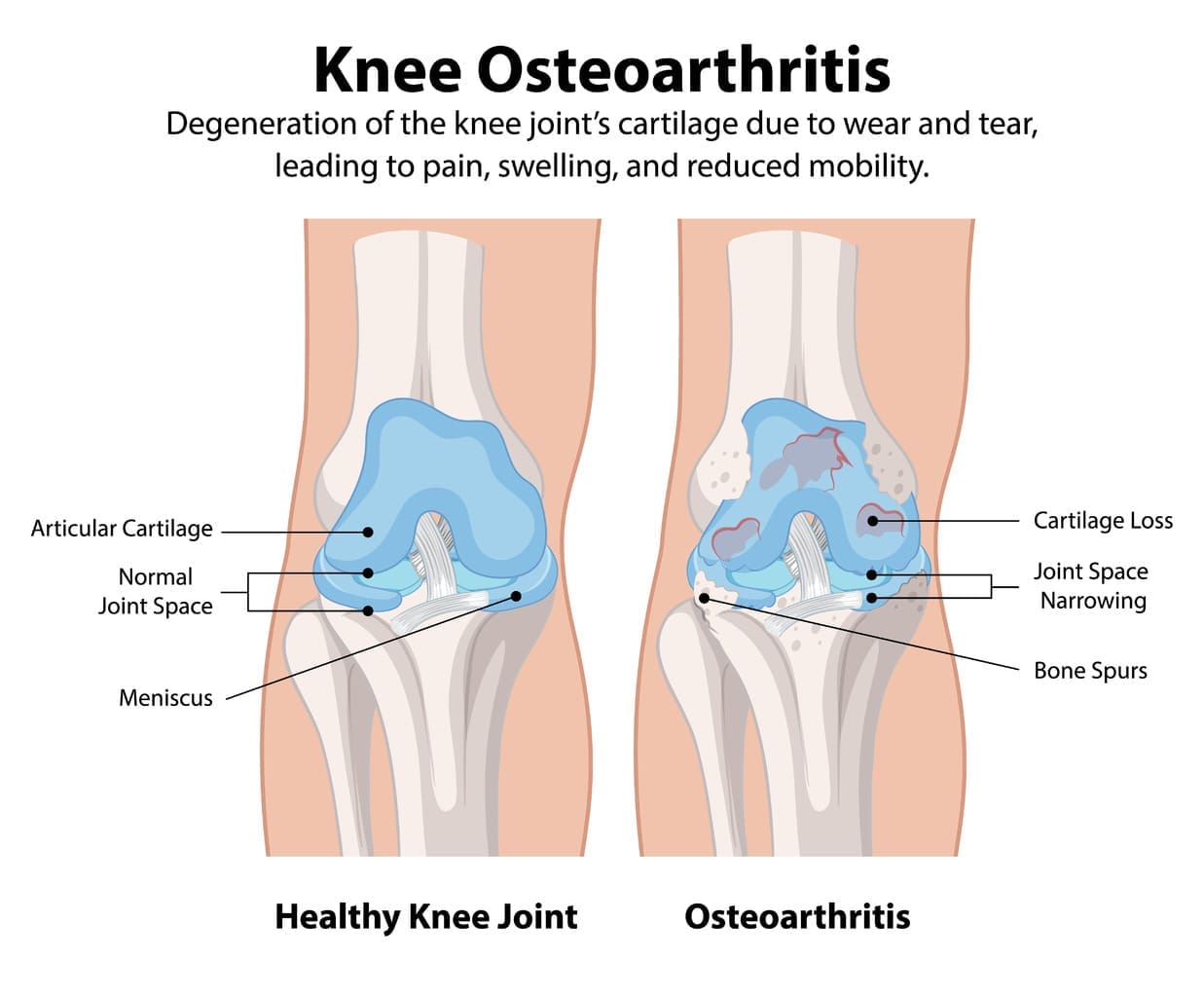
Osteoarthritis knee happens when the cartilage and bone in the knee wear out. Degenerative changes in knee happen when cartilage breaks down. This leads to bone rubbing against bone, causing pain and swelling.
The breakdown of cartilage is a key part of this disease. It’s caused by a mix of factors like age, genetics, and how much stress the knee gets.
The symptoms of osteoarthritis knee include pain when moving, stiffness, and trouble moving. Swelling, redness, and warmth around the knee can also happen.
Doctors look at your medical history and do a physical exam to check for osteoarthritis. They check for signs like a grinding feeling, limited movement, and pain when touched.
Some common symptoms to watch for are:
In summary, osteoarthritis knee is a condition that affects the knee. It causes a lot of discomfort and limits movement. Knowing about it helps in managing it better.
As the world’s population gets older, more people are getting knee osteoarthritis. This condition affects not just the person’s life quality but also puts a big strain on healthcare systems globally.
Knee osteoarthritis is a common type of arthritis. It’s getting more common as more people age. Over 237 million people worldwide have osteoarthritis, with many cases being knee osteoarthritis. It’s more common in women and people over 50, showing a clear trend.
Some groups are more likely to get knee osteoarthritis. These include:
Osteoarthritis knee changes the joint in complex ways, causing pain and less mobility. As it gets worse, people may feel a lot of pain and have a lower quality of life. We will look at how cartilage wears down and the changes in the knee joint. This will help us understand how osteoarthritis knee progresses.
Cartilage loss is a key part of osteoarthritis knee. It starts with cartilage softening and then gets worse to fibrillation, making the cartilage rough and cracked. Eventually, cartilage loss happens, showing the bone underneath. This can cause pain and stiffness because of bone rubbing against bone.
The stages of cartilage loss can be divided into several main phases:
Osteoarthritis knee also has structural changes in the joint. These include bone spurs or osteophytes, which are abnormal bone growths that can cause pain and limit joint mobility. The joint space may also become narrower because of cartilage loss, putting more stress on the bone.
Other structural changes include:
Understanding these changes is key for effective treatment plans and managing symptoms. By focusing on both cartilage loss and structural changes, healthcare providers can give better care to patients with osteoarthritis knee.
Knowing what causes osteoarthritis in the knee is key to preventing and managing it. Osteoarthritis of the knee is a disease where cartilage and bone break down. Several factors can lead to its development and worsening.
Age is a big risk factor for osteoarthritis knee. As we get older, our cartilage wears down, making joints more prone to damage. Age-related wear and tear is unavoidable, but we can slow its effects with care and prevention.
Being overweight is another major risk for osteoarthritis knee. Extra weight puts more stress on the knee, speeding up cartilage loss. Keeping a healthy weight through diet and exercise can lower the risk of osteoarthritis knee.
Knee injuries, like fractures or sprains, can raise the risk of osteoarthritis. Trauma can start a degenerative process that may lead to osteoarthritis over time. Treating and rehabbing injuries well is key to avoiding long-term damage.
Knee joint malalignment, like knock knees or bow legs, can cause uneven weight distribution. This leads to faster wear and tear on cartilage. Fixing biomechanical issues with orthotics or physical therapy can help prevent osteoarthritis knee.
The following table summarizes the 7 key causes of osteoarthritis knee:
| Cause | Description | Preventive Measures |
|---|---|---|
| Age-Related Wear and Tear | Natural deterioration of cartilage with age | Proper care, exercise, and nutrition |
| Obesity and Excess Body Weight | Additional stress on the knee joint due to excess weight | Weight management through diet and exercise |
| Previous Joint Injuries | Trauma to the joint initiating degenerative processes | Proper treatment and rehabilitation of injuries |
| Joint Malalignment | Uneven weight distribution due to malaligned joints | Orthotics, physical therapy |
| Genetic Predisposition | Inherited traits increasing susceptibility | Awareness and early intervention |
| Repetitive Stress or Overuse | Repeated strain on the knee joint | Proper training, equipment, and rest |
| Muscle Weakness | Inadequate muscle support around the knee | Strengthening exercises |
By understanding these causes, we can take steps to lower our risk of osteoarthritis knee. Early action and preventive steps can greatly improve life quality for those at risk.
To diagnose degenerative joint disease of the knee, doctors use a detailed strategy. This includes clinical checks, imaging, and lab tests. This method helps ensure patients get the right diagnosis and treatment.
The first step is a detailed clinical check and physical exam. Doctors learn about the patient’s health history, symptoms, and lifestyle. They also check the knee’s movement, stability, and pain.
Key components of the clinical evaluation include:
Imaging is key in confirming degenerative joint disease of the knee. Doctors use X-rays, MRI, and CT scans for this purpose.
| Imaging Modality | Primary Use in DJD Knee Diagnosis |
|---|---|
| X-ray | Assessing joint space narrowing and bone spurs |
| MRI | Evaluating cartilage damage, ligament injuries, and soft tissue abnormalities |
| CT Scan | Detailed assessment of bone structure and detection of fractures or cysts |
Laboratory tests are also vital. They help rule out other conditions that might look like degenerative joint disease. These tests check for inflammation or other arthritis signs.
Differential diagnosis is a key part of the process. Doctors must look at other possible causes of knee pain, like rheumatoid arthritis or ligament injuries. By using clinical findings, imaging, and lab tests, they can accurately diagnose and treat the knee disease.
In conclusion, diagnosing degenerative joint disease of the knee needs a detailed approach. By combining clinical checks, imaging, and lab tests, doctors can accurately diagnose and manage this common condition. This improves patient outcomes and quality of life.
Osteoarthritis in the knee comes from both things you can change and things you can’t. Knowing these factors helps in preventing and managing the condition.
There are several risk factors for knee osteoarthritis that you can change. Obesity is a big one because extra weight stresses the knee. Eating right and exercising can help keep your weight in check.
Physical activity level is also something you can change. While exercise is good, some activities can harm your knees. Low-impact activities like cycling or swimming are better for your joints.
| Modifiable Risk Factor | Impact on Knee Osteoarthritis | Mitigation Strategy |
|---|---|---|
| Obesity | Increased stress on the knee joint | Maintain a healthy weight through diet and exercise |
| Physical Activity Level | High-impact activities may increase risk | Engage in low-impact exercises like cycling or swimming |
Some risk factors you can’t change, but knowing them helps in early detection. Age is a big one because the risk goes up as you get older. Also, genetic predisposition matters, with a family history increasing your risk.
Knowing both types of risk factors helps you take steps to manage your risk for DJD of the knee. By changing what you can and being aware of what you can’t, you can prevent or delay knee osteoarthritis.
To prevent osteoarthritis knee, we need to make lifestyle changes and take proactive steps. Knowing the risk factors and using prevention strategies can lower the chance of getting degenerative joint disease in the knee.
Keeping a healthy weight is key to preventing osteoarthritis knee. Being overweight adds stress to the knee joint, speeding up wear and tear. Eating a balanced diet with fruits, vegetables, and omega-3 fatty acids can help reduce inflammation and keep joints healthy.
Some important nutritional tips include:
| Nutrient | Benefit | Food Sources |
|---|---|---|
| Omega-3 Fatty Acids | Reduces inflammation | Salmon, Walnuts, Chia Seeds |
| Vitamin D | Supports bone health | Fatty Fish, Fortified Dairy, Sunlight Exposure |
| Antioxidants | Combats oxidative stress | Berries, Leafy Greens, Nuts |
Doing regular, low-impact exercise is vital for knee health. Swimming, cycling, and brisk walking strengthen the muscles around the knee without putting too much stress on the joint.
“Exercise is essential for keeping joints mobile and strong, which helps prevent osteoarthritis knee.”
A renowned orthopedic specialist
Protecting the knee joint during daily tasks can prevent unnecessary wear and tear. Use proper lifting methods, avoid repetitive strain, and wear supportive shoes.
Some supplements, like glucosamine and chondroitin, may support joint health. But, always talk to a healthcare professional before taking any supplements.
Early interventions, such as physical therapy and bracing, are also important in preventing knee degeneration from getting worse.
Managing osteoarthritis knee involves many steps to ease symptoms and improve life quality. We will look at different ways to handle osteoarthritis knee well.
Physical therapy is key in managing osteoarthritis knee. It includes exercises to improve joint movement, strengthen muscles, and boost function. A physical therapist creates a program that fits the patient’s needs, focusing on safe and effective exercises.
A study in the Journal of Orthopaedic & Sports Physical Therapy found that physical therapy can greatly reduce pain and improve function in those with knee osteoarthritis
“Physical therapy interventions, including exercise and manual therapy, are effective in reducing pain and improving function in patients with knee osteoarthritis.”
| Exercise Type | Benefits |
|---|---|
| Strengthening Exercises | Improve muscle strength around the knee |
| Aerobic Exercises | Enhance cardiovascular health and reduce pain |
| Flexibility Exercises | Increase range of motion and reduce stiffness |
Medications help manage pain and inflammation in osteoarthritis knee. We’ll talk about the benefits and risks of these medications to help patients make smart choices.
Acetaminophen is often the first choice for pain relief. NSAIDs help reduce inflammation but can cause stomach problems. Corticosteroid injections offer quick pain relief during flare-ups.
Assistive devices and braces are important in managing osteoarthritis knee. Canes, walkers, and orthotics reduce knee joint load. Braces offer extra support and stability.
Lifestyle changes are key in managing osteoarthritis knee. Keeping a healthy weight, staying active, and adopting joint-friendly habits can greatly help symptoms.
Managing weight is critical, as extra weight worsens the condition. A balanced diet and regular exercise help maintain a healthy weight.
When simple treatments don’t work, more advanced options are needed. These treatments help manage pain and improve function. We’ll look at injections, regenerative medicine, and surgery.
Injections are a key treatment for knee osteoarthritis. Viscosupplementation therapy uses hyaluronic acid to improve joint lubrication and reduce pain. It offers relief for many patients.
Corticosteroid injections also help by reducing inflammation. But, they should be used carefully due to possible side effects. We weigh the benefits and risks to choose the best treatment.
Regenerative medicine is a new area in treating knee osteoarthritis. Platelet-rich plasma (PRP) therapy uses the patient’s own blood to stimulate healing. It may help repair damaged tissue.
Stem cell therapy is another new method. It uses stem cells to repair cartilage. More research is needed to fully understand its benefits.
For severe cases, surgery is often the best option. Joint replacement surgery can greatly improve quality of life. It replaces the damaged joint with an artificial one.
Other surgeries include osteotomy and arthroscopy. Osteotomy realigns the knee to better distribute weight. Arthroscopy is a minimally invasive procedure to remove damaged tissue. The right surgery depends on the disease’s severity and the patient’s health.
Advanced treatments for knee osteoarthritis offer hope. Understanding these options helps patients make better choices for their care.
We’ve looked into osteoarthritis knee, also known as degenerative joint disease knee. It affects the knee joint. Knowing the causes, how to diagnose it, and treatment options is key to managing it well.
Managing osteoarthritis knee needs a mix of approaches. This includes physical therapy and making lifestyle changes. Sometimes, injections or surgery are needed. Taking action early can greatly improve life quality.
It’s vital to work with healthcare experts to create a treatment plan that fits you. The right mix of medical care and self-care can help control symptoms and keep you moving.
We stress the need for a supportive and informed way to handle osteoarthritis knee. Being well-informed and active in your care helps you face the challenges of degenerative joint disease knee. This way, you can live an active and meaningful life.
Osteoarthritis of the knee is a condition where cartilage in the knee joint breaks down. This leads to pain, stiffness, and limited mobility.
Symptoms include pain, stiffness, and limited mobility. You might also feel swelling and a grinding sensation in the knee.
Causes include age, obesity, and previous injuries. Other factors are joint malalignment, genetics, and repetitive stress.
Diagnosis involves a clinical evaluation and imaging studies. Tests like X-rays or MRI are used to confirm the condition.
Prevention is possible by maintaining a healthy weight and exercising. Using joint protection techniques and supplements can also help.
Treatment includes physical therapy and medications. Advanced options are injections, regenerative medicine, and surgery.
Manage symptoms by making lifestyle changes. Use assistive devices and follow a treatment plan with a healthcare professional.
Yes, it is a degenerative condition. It involves the progressive breakdown of cartilage and changes in the knee joint.
Yes, many people manage symptoms without surgery. This is through conservative management and advanced non-surgical treatments.
Maintaining a healthy weight is key. Excess weight adds stress to the knee joint, worsening symptoms.
Physical activity helps manage symptoms. It improves joint mobility and strengthens muscles around the knee.
National Center for Biotechnology Information (NCBI). PMC12351899. https://pmc.ncbi.nlm.nih.gov/articles/PMC12351899
National Center for Biotechnology Information (NCBI). PMC11993502. https://pmc.ncbi.nlm.nih.gov/articles/PMC11993502
Centers for Disease Control and Prevention (CDC). Osteoarthritis. https://www.cdc.gov/arthritis/osteoarthritis/index.html
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!