Hip surgeries are very common. They help people with severe pain and limited movement. This is due to arthritis, hip fractures, dysplasia, and avascular necrosis.
-Dr. a skilled orthopedic surgeon, says hip replacement and preservation services are key. At Liv Hospital, we focus on top-notch care for international patients.
We’ll explain five main hip surgery types. You’ll learn about their procedures and risks. This will help you make better health choices.
Key Takeaways
- Understanding the different types of hip surgeries available.
- Recognizing the conditions treated by hip replacement surgery.
- Learning about the procedures and risks associated with each surgery type.
- Gaining insights into the expertise of orthopedic surgeons.
- Making informed decisions about your hip health.
Understanding Hip Surgery: When Is It Necessary?
When you face hip problems, knowing when surgery is needed is key. Surgery is often considered when other treatments don’t work or the condition is severe. We’ll look at common conditions that need surgery and signs it’s time to think about it.
Common Conditions Requiring Hip Surgery
Several hip conditions may need surgery. These include:
- Advanced arthritis, which causes significant joint damage and pain.
- Hip fractures, often resulting from falls or osteoporosis.
- Dysplasia, a condition where the hip joint doesn’t form properly.
- Labral tears, which can cause pain and limited mobility.
Procedures like hip arthroscopy are often used to address issues such as labral tears or impingement. In cases of severe arthritis or fractures, hip osteotomy or even total hip replacement might be necessary.
Signs You May Need Hip Surgery
Knowing the signs you need hip surgery is important. These signs include:
- Persistent pain that interferes with daily activities.
- Significant stiffness or limited range of motion.
- Instability or feeling like the hip is going to give way.
- Failure of conservative treatments like physical therapy or medications.
If you’re experiencing any of these symptoms, it’s essential to consult with an orthopedic specialist. They can evaluate your condition and recommend the most appropriate treatment, which may include surgery.
Understanding the necessity of hip surgery involves recognizing both the conditions that require it and the signs that indicate it’s necessary. By addressing these factors, patients can make informed decisions about their care.
The Anatomy of the Hip Joint

Knowing how the hip joint works is key to fixing hip problems. The hip is a ball-and-socket joint that links the femur to the pelvis. It lets us move freely and bear our body’s weight.
Structure and Function
The hip is built for both strength and flexibility. It has the acetabulum, a socket in the pelvis, and the femoral head, the ball at the femur’s top. Both are covered in articular cartilage, making movement smooth and absorbing shock.
The joint is also wrapped in a capsule of ligaments and muscles. These add support and allow for flexion, extension, and rotation.
Common Hip Problems
Despite its strong design, the hip can face many issues. Problems like labral tears and osteoarthritis can occur. Labral tears affect the cartilage ring around the acetabulum, while osteoarthritis wears down the cartilage.
Other issues include hip dysplasia and femoroacetabular impingement (FAI). Hip dysplasia makes the hip socket too shallow, and FAI causes abnormal contact between the femoral head and acetabulum. These can cause pain, less mobility, and may require surgery like hip labrum repair or hip resurfacing surgery.
Total Hip Replacement (Arthroplasty)
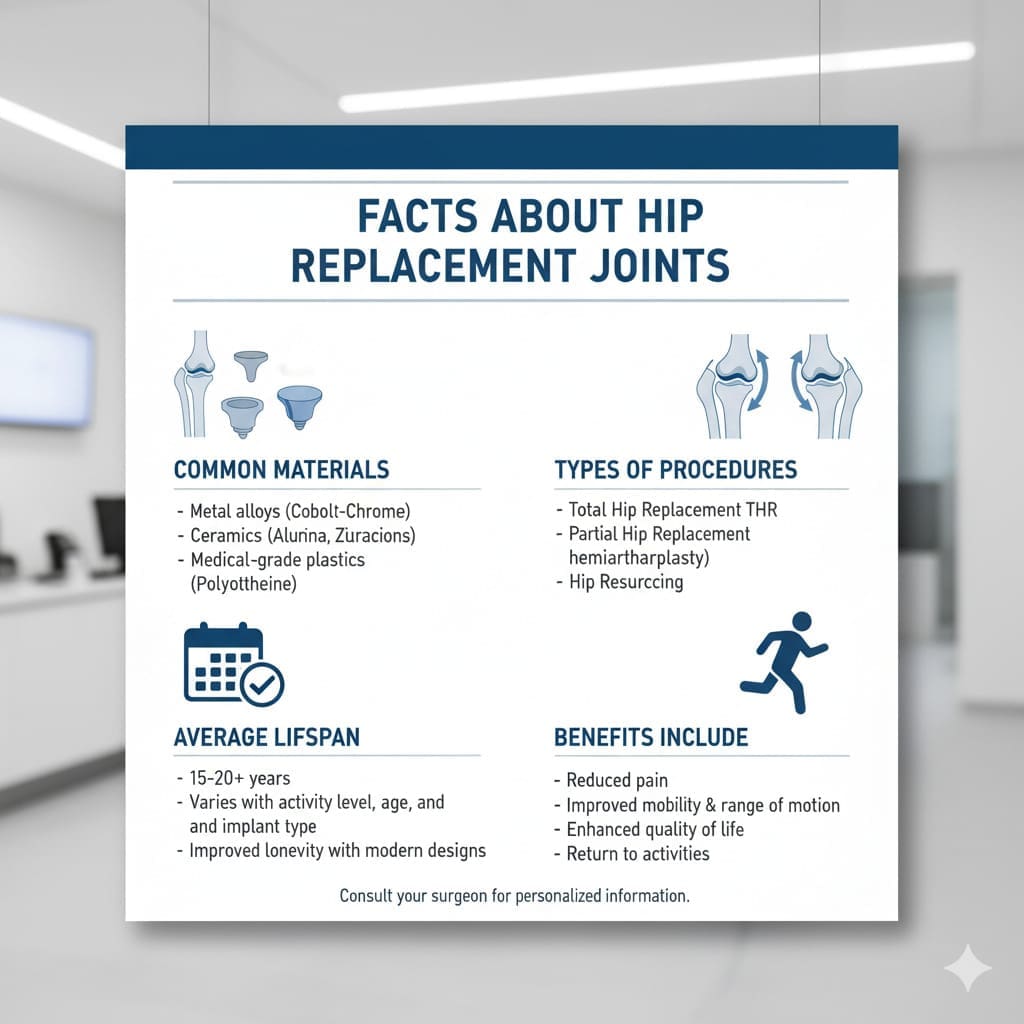
For those with severe hip arthritis or fractures, total hip replacement surgery is a great option. It helps restore mobility and ease pain. The surgery replaces the damaged hip joint with artificial parts, improving life quality.
The Procedure
Total hip replacement is a detailed surgery needing careful planning. It involves removing the damaged parts and replacing them with prosthetics. These parts are made to move like the natural hip, helping patients move freely again.
The surgery is done under general or regional anesthesia, based on the patient’s health and the surgeon’s choice. It usually takes 1-2 hours to complete.
Who Are the Candidates?
Those with severe hip arthritis or fractures are often candidates. These conditions can cause chronic pain and limit movement.
Recent studies show total hip replacement is very effective for these issues. The best candidates are those with:
- Severe hip pain that affects daily life
- Limited mobility due to stiffness or pain
- Failed to improve with conservative treatments
- Significant joint damage or deformity
Recovery and Rehabilitation
Recovery after total hip replacement is key for good results. Patients usually stay in the hospital for a few days. They start their rehabilitation there, focusing on pain management and physical therapy.
A leading orthopedic surgeon emphasizes the importance of a well-planned rehabilitation. It includes physical therapy, pain management, and lifestyle changes.
“Rehabilitation after total hip replacement is not just about regaining strength; it’s about regaining independence and improving the quality of life.”
The rehabilitation process includes several phases:
| Rehabilitation Phase | Timeline | Goals |
|---|---|---|
| Immediate Post-Surgery | 0-2 weeks | Pain management, wound healing, initial mobility |
| Early Rehabilitation | 2-6 weeks | Regaining strength, improving range of motion |
| Advanced Rehabilitation | 6-12 weeks | Improving functional ability, returning to daily activities |
Potential Risks and Complications
While total hip replacement is safe and effective, there are risks. These include infection, blood clots, nerve damage, and implant failure.
To reduce these risks, patients must follow their surgeon’s advice and attend all follow-up appointments. Understanding and managing these risks can help ensure a successful outcome.
Revision hip surgery may be needed if the initial implant fails or loosens over time. This highlights the need for ongoing care and monitoring.
Partial Hip Replacement (Hemiarthroplasty)
Partial hip replacement is different from total hip replacement. It only replaces the damaged part of the hip. This is often chosen for those with hip fractures, like older adults whose bones might not be strong enough for a full replacement.
Differences from Total Hip Replacement
Partial hip replacement only replaces one part of the joint, usually the ball. Total hip replacement, on the other hand, replaces both the ball and socket. This makes partial hip replacement less complex and can lead to quicker recovery times.
Choosing between these options depends on the patient’s health and the extent of the damage. Partial hip replacement is less invasive and might have fewer complications.
Ideal Candidates
Partial hip replacement is often for patients with hip fractures, mainly the elderly. The best candidates have:
- A significant hip fracture that can’t be fixed other ways
- Poor bone quality, making total hip replacement hard
- Limited mobility or activity, which reduces stress on the joint
But, each case is different. The decision to have partial hip replacement should consider the patient’s health, bone quality, and activity level.
Recovery Timeline
The recovery time for partial hip replacement varies. It depends on the patient’s age, health, and surgery complexity. Here’s what to expect:
| Recovery Stage | Timeline | Expected Progress |
|---|---|---|
| Immediate Post-Surgery | 0-2 weeks | Pain management, initial mobility |
| Early Rehabilitation | 2-6 weeks | Increased mobility, strengthening exercises |
| Advanced Rehabilitation | 6-12 weeks | Improved strength, range of motion, and function |
Risks and Complications
Partial hip replacement is generally safe but comes with risks. Possible complications include:
“Complications after hemiarthroplasty can include infection, dislocation, and fracture of the femur. Careful patient selection and surgical technique are key to reducing these risks.”
Other risks and complications include:
- Infection
- Dislocation of the prosthesis
- Nerve damage
- Blood clots
It’s important for patients to talk to their healthcare provider about these risks. This way, they can understand the possible complications and how to avoid them.
Hip Resurfacing Surgery
Hip resurfacing surgery is a choice for those who don’t want a full hip replacement. It saves more bone by just covering the femoral head and lining the acetabulum with prosthetics. This is different from replacing the whole femoral head and neck.
Technique and Materials Used
There are many ways to do hip resurfacing surgery, depending on the doctor and the patient. The surgery starts with an incision to get to the hip joint. Then, the femoral head and acetabulum are prepared for the prosthetics.
The prosthetics used are metal-on-metal or metal-on-polyethylene. These are made to last a long time.
A study in the Journal of Orthopaedic Research found hip resurfacing is good for younger, active patients. It saves more bone and might lower the chance of needing more surgery later.
Advantages Over Traditional Replacement
Hip resurfacing saves more bone than traditional hip replacement. This makes it easier for future surgeries if needed. It also might make the joint more stable and lower the chance of dislocation.
“Hip resurfacing is a valuable option for patients who are looking for a more conservative approach to hip replacement. It offers several advantages, including reduced risk of dislocation and preservation of bone stock.” – Dr. an Orthopedic Surgeon
Potential Complications
Hip resurfacing surgery has its risks. These include metal ion release, loosening of the prosthetic components, and femoral neck fracture. It’s important for patients to talk to their surgeon about these risks before deciding.
Choosing the right patient and using the right technique are key to avoiding complications. This helps ensure a good outcome from the surgery.
Minimally Invasive Hip Surgery Techniques
Minimally invasive hip surgery has changed orthopedic surgery a lot. It helps patients recover faster and with less damage. These new methods aim to reduce scarring, lower pain, and speed up healing. This makes them a great choice for many.
Anterior Approach
The anterior approach is a new way to get to the hip from the front. It’s known for less muscle damage and quicker healing. Surgeons say it leads to less pain and better movement for patients.
Benefits of the Anterior Approach:
- Reduced muscle trauma
- Faster recovery times
- Less postoperative pain
- Improved hip mobility
Posterior Approach
The posterior approach gets to the hip from the back. It’s a common method with many successful results. It lets surgeons fix or replace the hip with little harm to nearby tissues.
Advantages of the Posterior Approach:
- Well-established surgical technique
- Effective for a wide range of hip conditions
- Good long-term outcomes
Benefits of Minimally Invasive Procedures
Both the anterior and posterior approaches have big advantages over old surgery methods. They use smaller cuts, cause less damage, and lead to less blood loss. Patients often feel less pain and get back to their lives sooner.
| Benefit | Minimally Invasive Surgery | Traditional Open Surgery |
|---|---|---|
| Incision Size | Smaller (2-4 inches) | Larger (6-12 inches) |
| Tissue Damage | Less damage | More extensive damage |
| Recovery Time | Faster recovery | Longer recovery period |
Limitations and Risks
Even with their benefits, these new surgeries have some downsides. They can be hard for surgeons to learn, might hurt nerves, and not fix the hip fully. It’s key for patients to talk to their doctor about these risks and benefits.
Knowing about these hip surgery options helps patients make better choices. Always talk to a skilled orthopedic surgeon to find the best treatment for you.
Different Hip Surgeries for Specific Conditions
Different hip surgeries are designed to treat specific conditions. They improve patient outcomes and quality of life. We will explore the various surgical options available for conditions such as labral tears and dysplasia.
Hip Arthroscopy for Labral Tears
Hip arthroscopy is a minimally invasive surgical procedure. It is used to diagnose and treat hip labral tears. This technique involves inserting a small camera and surgical instruments through tiny incisions.
According to a study published in the Journal of Orthopaedic & Sports Physical Therapy, hip arthroscopy has shown significant improvements in patient-reported outcomes for those with labral tears. The procedure is beneficial for younger patients and athletes who wish to return to their active lifestyles.
“Hip arthroscopy has revolutionized the treatment of labral tears, providing a less invasive alternative to traditional open surgery.”
Hip Osteotomy for Dysplasia
Hip osteotomy is a surgical procedure that involves cutting and realigning the bones of the hip joint. This surgery is often used to treat hip dysplasia, a condition where the hip socket is too shallow.
By reorienting the acetabulum or femoral head, hip osteotomy can help alleviate pain. It improves joint congruence and delays the onset of osteoarthritis. The success of this procedure depends on careful patient selection and precise surgical technique.
| Procedure | Condition Treated | Benefits |
|---|---|---|
| Hip Arthroscopy | Labral Tears | Minimally invasive, quicker recovery |
| Hip Osteotomy | Hip Dysplasia | Improved joint congruence, delayed osteoarthritis |
Hip Labrum Repair Techniques
Hip labrum repair involves the surgical correction of labral tears or detachments. Techniques vary depending on the extent and location of the damage. Surgeons may use arthroscopic or open methods to repair or reconstruct the labrum.
The choice of technique depends on the patient’s anatomy, the severity of the labral damage, and the surgeon’s expertise. Advances in arthroscopic techniques have made labrum repair more accessible and effective.
Revision Hip Surgery
Revision hip surgery is performed to correct or replace a previously implanted hip prosthesis that has failed or is causing complications. This complex procedure requires careful planning and execution.
Revision hip surgery can be challenging due to factors like bone loss, scar tissue, and the need to remove the existing implant. Surgeons must be experienced in handling these complexities to achieve a successful outcome.
By understanding the different hip surgeries available for specific conditions, patients and healthcare providers can make informed decisions about the most appropriate treatment options.
Comprehensive Risk Assessment of Hip Surgeries
It’s important to know the risks of different hip surgeries. These surgeries can treat many hip problems but come with possible complications.
Infection and Blood Clots
Infection is a big risk with hip surgeries. Even with careful cleaning, infections can happen. We use antibiotics and keep the operating area clean to lower this risk.
Blood clots are another risk. We use blood thinners and encourage patients to move early to prevent this.
Key Measures to Reduce Infection and Blood Clots:
- Use of antibiotics
- Maintaining a sterile operating environment
- Use of blood thinners
- Early mobilization post-surgery
Nerve Damage and Dislocation
Nerve damage is a risk, mainly with complex surgeries. It can cause numbness or weakness in the leg. Though rare, it’s a serious issue.
Dislocation is also a risk, mostly in the first few weeks after surgery. We teach patients how to avoid it by not sitting in certain ways and using supports.
Precautions to Minimize Nerve Damage and Dislocation:
- Careful surgical planning
- Patient education on post-operative care
- Use of supportive devices
Implant Failure and Loosening
Implant failure and loosening are risks for hip replacements. The implant’s life depends on the type, patient activity, and health. Regular check-ups are key to catch any problems early.
Long-term Complications
Long-term issues include wear and tear, bone loss, or instability. These problems are not common but knowing them helps manage expectations and prevent them.
Understanding these risks helps patients make better choices. They can work with their doctors to reduce these risks.
Choosing the Right Hip Surgery: Factors to Consider
Choosing the right hip surgery is a big decision. It depends on several important factors. Patients need to think about these to get the best results for their condition.
Age and Activity Level
The patient’s age and how active they are matter a lot. Young, active people might do well with minimally invasive hip surgery or hip resurfacing. These options save more bone and help you recover faster.
On the other hand, older folks or those who are less active might do better with hip replacement surgery. This method has been around for a long time and can really improve your life.
Underlying Condition
The reason you need hip surgery is also key. Problems like osteoarthritis, fractures, or hip dysplasia need different solutions. For example, severe osteoarthritis might call for total hip replacement. But, some fractures might need partial hip replacement.
Surgeon Experience and Hospital Quality
The surgeon’s experience and the hospital’s quality are also important. A skilled surgeon can make a big difference in how well the surgery goes. Also, a top-notch hospital with a great orthopedic department can help you heal better.
We suggest talking over your options with your doctor. Think about the type of hip replacement surgery or the benefits of minimally invasive techniques. Making an informed choice can lead to better results and happiness.
In short, picking the right hip surgery takes careful thought. You need to consider your age, how active you are, your condition, the surgeon’s skills, and the hospital’s quality. By weighing these factors, you can make a choice that leads to good outcomes.
Conclusion: Advances in Hip Surgery and Future Outlook
Hip surgery has made big strides, leading to better results for patients. Now, there are many options for hip surgeries. Hip arthroscopy, for example, is a minimally invasive method that cuts down on recovery time.
New materials and surgical techniques have opened up more possibilities for hip surgery. This means patients can move better and feel less pain. They can choose from total hip replacement, partial hip replacement, and hip resurfacing, based on their condition and needs.
There’s always new stuff coming in hip surgery, like better implants and ways to avoid complications. The future looks bright, with robotic-assisted surgery and custom implants on the horizon. These could make surgery even better for patients.
As tech keeps getting better, hip surgery will get safer and more effective. This brings hope to those with hip problems. Keeping up with the latest in hip surgery, like hip arthroscopy, helps patients make smart choices about their care.
What are the different types of hip surgeries available?
We offer many hip surgeries. These include total hip replacement, partial hip replacement, and hip resurfacing. We also do minimally invasive hip surgery, hip arthroscopy, hip osteotomy, and revision hip surgery. Each is for different conditions and needs.
When is hip surgery necessary?
Hip surgery is needed for severe arthritis, fractures, or hip dysplasia. These conditions must be severe and not helped by other treatments.
What is the difference between total hip replacement and partial hip replacement?
Total hip replacement replaces the whole joint. Partial hip replacement only fixes the damaged part, keeping the healthy parts.
What is hip resurfacing surgery, and who is it suitable for?
Hip resurfacing caps the femoral head with a metal implant. It keeps more of the natural bone. It’s good for younger, active patients.
What are the benefits of minimally invasive hip surgery?
Minimally invasive hip surgery has many benefits. It uses smaller incisions and causes less tissue damage. This means less pain and a quicker recovery.
What is hip arthroscopy used for?
Hip arthroscopy is a small procedure to diagnose and treat hip problems. It’s used for labral tears, femoroacetabular impingement, and other hip issues.
What is revision hip surgery, and why is it performed?
Revision hip surgery corrects or replaces a failed hip prosthesis. It’s often needed for complications like loosening, infection, or wear.
What are the possible risks and complications of hip surgeries?
Risks include infection, blood clots, nerve damage, and dislocation. There’s also a chance of implant failure and long-term problems like loosening or wear.
How do I choose the right hip surgery for my condition?
The right surgery depends on your age, activity level, condition, and the surgeon’s advice. We consider these to find the best option for you.
What can I expect during the recovery and rehabilitation after hip surgery?
Recovery starts with rest, followed by physical therapy. This helps regain strength and mobility. The process varies based on the surgery and your needs.
How do advances in hip surgery techniques and materials impact patient outcomes?
Advances in hip surgery have improved outcomes. They include longer-lasting implants, quicker recovery times, and better patient satisfaction. These advancements offer new hope for patients.

































