If you’re dealing with back pain from bulging or herniated discs, it’s time to look into lumbar discectomy options. At Liv Hospital, we offer a detailed look at the top disc surgery options out there.
Our hospital is dedicated to top-notch healthcare, supporting patients from around the world. Studies show that minimally invasive approaches have fewer complications and can be just as good as open surgeries. We aim to help you move freely and live better, backed by our expert team and cutting-edge methods.
Key Takeaways
- Effective lumbar discectomy options for relieving nerve compression
- Minimally invasive approaches for lower complication rates
- World-class expertise and innovative solutions at Liv Hospital
- Comprehensive support for international patients
- Personalized care for optimal outcomes
Understanding Lumbar Disc Herniation and Nerve Compression
It’s important to know about lumbar disc herniation to treat nerve compression well. This happens when the soft center of the disc leaks out. This can press on nearby nerves.
Anatomy of the Lumbar Spine and Disc Structure
The lumbar spine has five vertebrae, from L1 to L5. Between each vertebra, there’s a disc that acts as a shock absorber. These discs help the spine move and stay strong. The disc has a soft center and a tough outer layer.
Causes of Bulging, Slipped, and Herniated Discs
Disc herniation can come from many things, like getting older or injuries. Heavy lifting or bending can also cause it. Sometimes, herniated disc surgery is needed if other treatments don’t work.
| Cause | Description | Common Symptoms |
|---|---|---|
| Age-related wear | Degeneration of disc material over time | Pain, stiffness |
| Trauma | Sudden injury to the spine | Acute pain, numbness |
| Strain | Overuse or repetitive strain on the spine | Pain, weakness |
Symptoms Indicating Need for Surgical Intervention
Symptoms of lumbar disc herniation can be different. They often include back pain, numbness, or weakness in the legs. Nerve compression can cause more serious problems, like cauda equina syndrome. This is a medical emergency.
When treatments don’t help, surgical treatment for disc problems might be needed.
Signs that surgery is needed include:
- Severe pain that doesn’t go away with treatment
- Getting worse neurological problems
- Big nerve compression symptoms
In summary, knowing the causes and symptoms of lumbar disc herniation is key. If symptoms don’t get better or get worse, decompression surgery or other surgeries might be needed. This can help relieve nerve compression and improve life quality.
Back Surgery for Disc: When Conservative Treatments Fail
For many, back surgery for disc issues starts when other treatments don’t work. This change can be tough, both in body and mind. We aim to help you understand when surgery might be needed.
Progression from Non-Surgical to Surgical Options
Switching to surgery is a step taken when other treatments don’t help. Conservative treatments like physical therapy and medicine are tried first. If these don’t work, surgery might be suggested.
We focus on you, making sure surgery is right for your health and wishes. This means looking at your overall health, how bad your condition is, and what you prefer.
Diagnostic Criteria for Surgical Candidates
Figuring out if you need surgery involves a detailed check-up. This includes looking at your scans and how your symptoms affect you. Key criteria include nerve pressure, how bad the pain is, and how it affects your daily life.
- Significant nerve compression shown on MRI or CT scans
- Pain that’s very bad and stops you from doing daily things
- Other treatments not helping after a while
Setting Realistic Expectations for Surgical Outcomes
It’s important to know what to expect from back surgery for disc problems. Surgery can help a lot, but it’s not a fix-all. It might not get rid of all pain or let you do everything you could before.
We make sure you understand what surgery can and can’t do. This way, we work together to take care of you.
Traditional Open Lumbar Discectomy
The traditional open lumbar discectomy is a common and effective surgery for lumbar disc herniation. It has been improved over time to help those with disc problems.
Procedure Overview and Surgical Technique
This surgery involves an incision in the back to reach the herniated disc. The surgeon removes the part of the disc pressing on the nerve. This relieves pain and symptoms. This method is used for more complex cases or when other options are not good. It’s done under general anesthesia, so the patient is comfortable.
The surgeon uses special tools to move muscles and tissues. This gives a clear view of the disc. The goal is to remove the bad disc material without harming nearby tissues.
Ideal Candidates for Open Discectomy
Open discectomy is suggested for those with severe disc herniation who haven’t gotten better with other treatments. Ideal candidates have nerve compression causing pain, numbness, or weakness that affects daily life. The choice to do open discectomy is based on thorough evaluation and tests.
Those with complex disc herniations or scar tissue from previous surgeries may also benefit from this approach.
Recovery Timeline and Post-Operative Care
Recovery from open lumbar discectomy varies, but most can start with light activities in a few weeks. Post-operative care includes managing pain, physical therapy, and gradually increasing activity. It’s important to avoid heavy lifting and bending early on.
Regular follow-ups with the surgeon are key to check on healing and address any issues. Physical therapy helps patients regain strength and flexibility.
Long-Term Outcomes and Success Rates
Research shows that traditional open lumbar discectomy can offer lasting relief for many. Success rates are high, with many patients seeing improvement in symptoms and quality of life. But, as with any surgery, there are risks and complications to discuss with a healthcare provider.
“The open discectomy technique has been a cornerstone in the treatment of lumbar disc herniations, providing a reliable solution for patients with severe symptoms.”
Long-term results depend on the patient’s health, the severity of the herniation, and following post-operative care.
Microscopic Lumbar Discectomy: Enhanced Precision
Microscopic lumbar discectomy is a big step forward in treating lumbar disc herniation. It brings better precision and results for patients. This method has improved to handle spinal issues better, making it a more precise way to relieve nerve pressure.
Advanced Visualization Technology
Microscopic lumbar discectomy uses advanced tech for better views. Surgeons use a microscope to see in detail, making it easier to remove the herniated disc. This enhanced visualization helps them avoid harming nearby tissues, lowering the chance of problems.
Surgical Approach and Technique
The surgery starts with a small cut in the back. The microscope and tools are then inserted through this small opening. The surgeon looks at the disc and nerves through the microscope, carefully taking out the herniated part. This minimally invasive method aims to cause less damage and help the body heal faster.
Reduced Tissue Trauma and Faster Recovery
Microscopic lumbar discectomy leads to less damage and quicker healing. It causes less pain after surgery and lets patients get back to their lives sooner. Research shows that patients have shorter hospital stays and can get back to their daily activities faster than with traditional surgery.
Comparative Outcomes with Traditional Methods
Comparing microscopic lumbar discectomy to traditional surgery shows some big differences. Here’s a table that highlights these differences:
| Outcome Measure | Microscopic Lumbar Discectomy | Traditional Open Discectomy |
|---|---|---|
| Surgical Precision | High, due to advanced visualization | Dependent on surgeon’s experience |
| Tissue Trauma | Minimal, due to smaller incision | More extensive, due to larger incision |
| Recovery Time | Faster, with less post-operative pain | Longer, with more post-operative pain |
In summary, microscopic lumbar discectomy is a precise and effective treatment for lumbar disc herniation. Its use of advanced tech, small incision, and quick recovery times make it a great choice for those looking for back pain relief.
Minimally Invasive Microdiscectomy Procedures
Minimally invasive microdiscectomy has changed how we treat lumbar disc herniations. It allows for a quicker recovery and less damage to tissues. This method uses advanced technology and tools to reduce harm to surrounding tissues. This leads to less pain after surgery and a faster return to daily activities.
Specialized Tools and Surgical Techniques
This surgery uses special tools and techniques. High-resolution microscopes and micro-instruments help surgeons remove the herniated disc material. This is done through smaller incisions, causing less tissue damage.
- High-resolution microscopes for enhanced visualization
- Micro-instruments for precise removal of herniated disc material
- Specialized retractors to minimize tissue disruption
Benefits for Reducing Hospital Stay and Complications
The minimally invasive approach lowers the risk of complications and shortens hospital stays. It reduces tissue damage and post-operative pain. This means patients can recover faster and get back to their normal activities sooner.
Key benefits include:
- Reduced hospital stay due to faster recovery
- Lower risk of complications such as infection and bleeding
- Less post-operative pain and discomfort
Patient Selection Criteria
Not every patient is a good fit for this surgery. The decision to have the procedure depends on a detailed evaluation. This includes the severity of the disc herniation, overall health, and previous treatments.
Ideal candidates typically have:
- Symptomatic lumbar disc herniation confirmed by imaging studies
- Failed conservative treatment options
- No significant spinal instability or other complicating factors
Recovery Protocol and Return to Activities
A good recovery plan is key for the best results after this surgery. Patients usually follow a rehabilitation program. This includes physical therapy and exercises to strengthen muscles.
- Immediate post-operative care focusing on pain management and wound healing
- Gradual mobilization and physical therapy to restore strength and flexibility
- Progressive return to normal activities and sports
Targeted Discectomy for L5-S1 Herniation
We specialize in targeted discectomy procedures for L5-S1 herniation. This treatment is precise and effective. The lumbosacral junction, where the lumbar spine meets the sacrum, is a common area for disc herniation. This often leads to significant discomfort and nerve compression.
Anatomical Considerations of the Lumbosacral Junction
The L5-S1 level is subject to unique anatomical stresses. This makes disc herniation a frequent occurrence. Understanding the complex anatomy of this region is key for effective surgical planning.
Specialized Approaches for L5-S1 Disc Problems
Targeted discectomy for L5-S1 herniation uses specialized techniques. These techniques are tailored to the individual’s anatomy and condition. This approach ensures minimal tissue disruption and optimal decompression of the affected nerves.
Managing Sciatic Nerve Compression
Sciatic nerve compression is a common complication of L5-S1 disc herniation. Effective management involves relieving pressure on the nerve through precise surgical techniques.
Post-Operative Rehabilitation for Optimal Results
Post-operative care is critical for recovery. A well-structured rehabilitation program helps in regaining strength, improving mobility, and ensuring long-term success.
| Aspect | Description | Benefit |
|---|---|---|
| Anatomical Consideration | Understanding the lumbosacral junction anatomy | Effective surgical planning |
| Specialized Approach | Tailored techniques for L5-S1 disc problems | Minimal tissue disruption |
| Nerve Compression Management | Relieving pressure on the sciatic nerve | Symptom relief |
| Post-Operative Rehabilitation | Structured rehabilitation program | Optimal recovery and long-term success |
Surgical Options for L3-L4 and L4-L5 Disc Herniation
Surgery for L3-L4 and L4-L5 disc herniation needs a careful plan. This is because the middle lumbar area is complex. We will look at the special challenges and how to tackle them surgically.
Unique Challenges of Middle Lumbar Region
The middle lumbar spine, with L3-L4 and L4-L5 discs, has its own set of problems. It’s close to important nerves and has a complex structure. This makes surgery here very precise.
Key challenges include:
- Navigating complex spinal anatomy
- Managing nerve root compression
- Minimizing tissue trauma
Tailored Surgical Approaches for Different Levels
Doctors use different methods for L3-L4 and L4-L5 herniations. These include microscopic and minimally invasive discectomy. The choice depends on the patient’s body, the herniation’s severity, and the doctor’s skill.
Advanced visualization technologies help make these surgeries more precise.
Treatment of Lumbar Herniated Nucleus Pulposus (HNP)
Lumbar HNP, or herniated disc, happens when the nucleus pulposus bulges out. This can press on nerves. Surgery aims to ease this pressure and stabilize the spine.
Recovery Considerations and Success Rates
Recovering from L3-L4 and L4-L5 surgery involves rest, physical therapy, and managing pain. Most people see a big improvement in their symptoms. Success rates are high.
Factors influencing recovery include:
- Pre-operative condition of the patient
- Surgical technique used
- Post-operative care and rehabilitation
Endoscopic and Percutaneous Discectomy Innovations
Endoscopic and percutaneous discectomy are new ways to treat lumbar disc herniations. These minimally invasive back surgery methods aim to fix the flaws of old surgeries. They help patients heal faster and with less damage.
Cutting-Edge Minimally Invasive Techniques
Endoscopic discectomy uses a small endoscope to see the disc and area around it. This lets doctors remove the herniated disc material accurately. Percutaneous discectomy, by contrast, uses a needle or small tool to reach the disc through the skin, often under local anesthesia. Both methods aim to cause less harm and speed up healing.
Advantages for Selected Patient Populations
These new methods have many benefits for certain patients. Those with contained disc herniations or at high risk for open surgery complications might benefit most. The lower risk of infection, less pain, and shorter hospital stays make these options appealing to patients and doctors alike.
Reduced Tissue Damage and Faster Recovery
Endoscopic and percutaneous discectomy reduce tissue damage. With smaller incisions and less muscle retraction, more of the natural anatomy is preserved. This leads to faster recovery times and quicker return to normal activities compared to traditional surgery.
Limitations and Future Developments
Despite their benefits, these methods have their limits. Success depends on choosing the right patients, and they’re not for all disc herniations. Research and new tech are expected to broaden their use and improve results. Future advancements might include better visualization tools, more precise instruments, and possibly robotics or other advanced technologies.
Conclusion: Making Informed Decisions About Lumbar Discectomy
It’s important to know about disc surgery options if you’re thinking about back surgery. Lumbar disc surgery can help if you have a herniated disc or nerve compression.
Learning about different surgeries like open, microscopic, and minimally invasive procedures helps. This way, you can make better choices for your care. We help our patients by giving them all the information they need.
We offer top-notch healthcare and support for patients from around the world. Our team is here to guide you from the first visit to after surgery. We aim for a smooth recovery and the best results.
Choosing the right lumbar disc surgery means understanding your options well. Talk to your surgeon about your needs and worries. This will help decide the best treatment for you.
What is lumbar discectomy, and when is it necessary?
Lumbar discectomy is a surgery to ease pressure on spinal nerves from a herniated disc. It’s needed when other treatments don’t work and you have severe pain, numbness, or weakness in your legs.
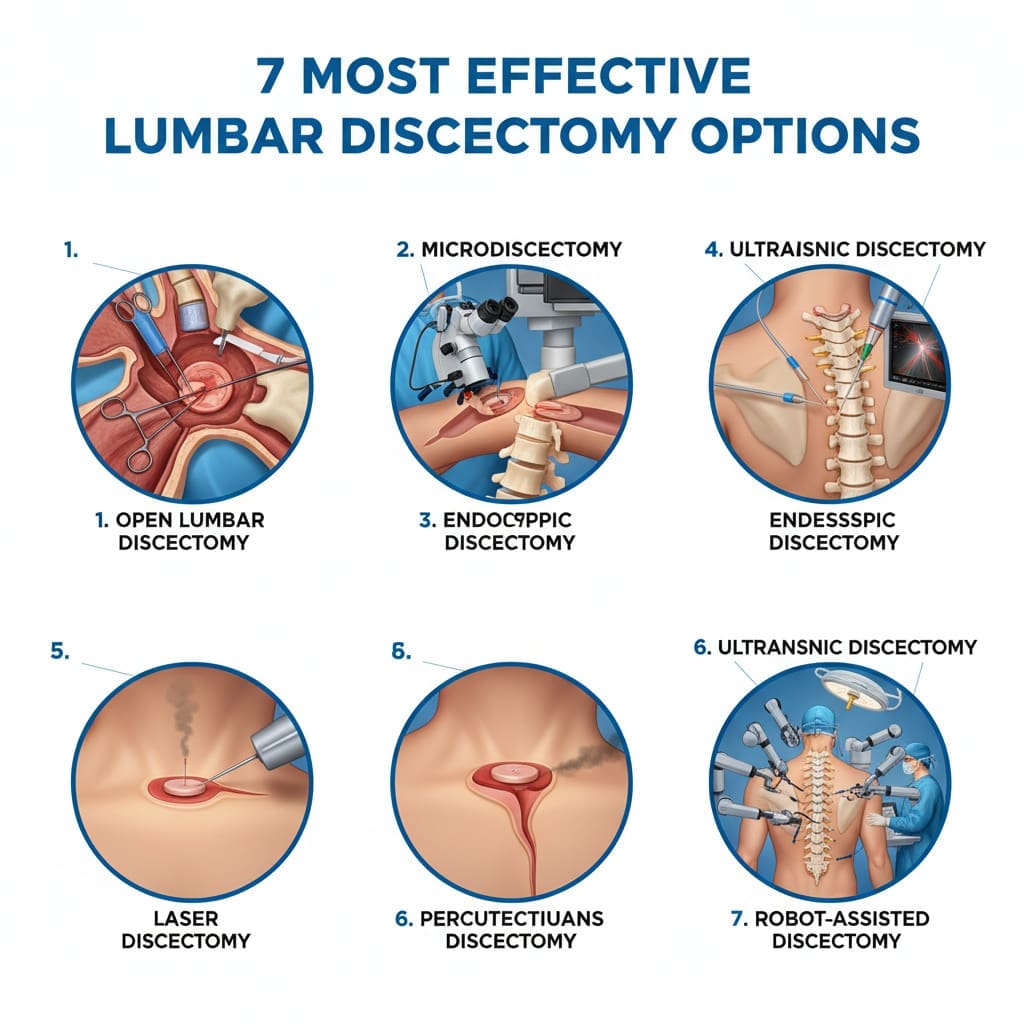
What are the different types of lumbar discectomy procedures?
There are many types of lumbar discectomy surgeries. These include traditional open discectomy, microscopic discectomy, and minimally invasive microdiscectomy. There’s also endoscopic discectomy and percutaneous discectomy. Each type has its own benefits and is right for different patients.
How do I know if I’m a candidate for lumbar discectomy surgery?
You might need lumbar discectomy if a herniated disc is pressing on your nerves and you’ve tried other treatments without relief. Tests like MRI or CT scans help decide if surgery is right for you.
What is the recovery time for lumbar discectomy?
Recovery time varies by the surgery type. Minimally invasive surgeries usually mean quicker recovery, often in a few weeks. Traditional open discectomy might take longer.
What are the benefits of minimally invasive lumbar discectomy?
Minimally invasive lumbar discectomy has many advantages. It causes less tissue damage, leads to less pain after surgery, and you might stay in the hospital less time. You also recover faster than with traditional surgery.
Are there any risks or complications associated with lumbar discectomy?
Like any surgery, lumbar discectomy has risks. These include infection, bleeding, nerve damage, or the disc could herniate again. But, these problems are rare, and most people see a big improvement in their symptoms.
Can I undergo lumbar discectomy if I have had previous back surgery?
You can have lumbar discectomy after previous back surgery, but it depends on your situation. The reason for the previous surgery and your spine’s current state are important. You should talk to a specialist to figure out the best option for you.
How effective is lumbar discectomy in relieving symptoms?
Lumbar discectomy is very effective for symptoms from herniated discs. Many people see a big improvement in pain, numbness, and weakness. How well it works can depend on the surgery and the person.
What is the role of physical therapy after lumbar discectomy?
Physical therapy is key after lumbar discectomy. It helps you regain strength, improve flexibility, and heal. A custom rehabilitation plan can greatly improve your outcome and lower the chance of future problems.
How do I choose the right surgeon for my lumbar discectomy?
Picking the right surgeon is important. Look at their experience with your procedure, success rates, patient feedback, and how well they communicate. Make sure they work at a reputable hospital that offers full support.
References
PubMed Central (NCBI): Spine Surgery for Failed Back Surgery Syndrome
PubMed Central (NCBI): Complications in Pediatric Spine Surgery









