mri of shoulder impingement
Did you know that nearly 70% of people with shoulder pain might have shoulder impingement? This is when the tendons or bursae in the shoulder joint get inflamed or irritated.
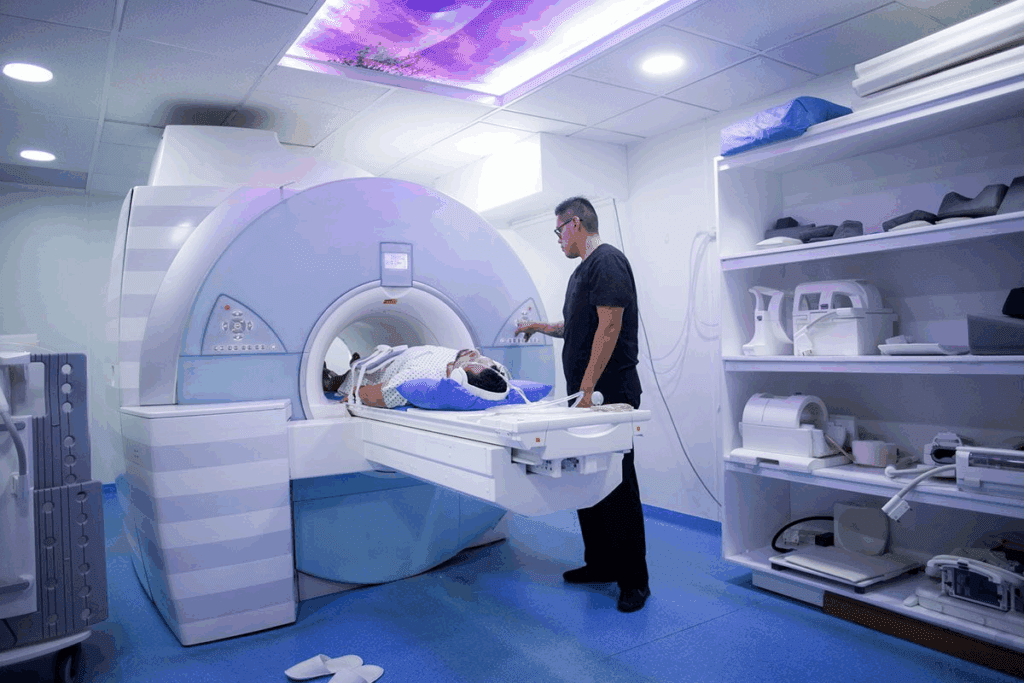
We use magnetic resonance imaging (MRI) to spot this issue. It helps us see how bad the impingement is. An MRI of the shoulder lets our team know exactly what to do next.
Key Takeaways
- MRI is a diagnostic tool used to visualize shoulder impingement.
- Shoulder impingement affects a significant portion of people with shoulder pain.
- A customized care plan can be developed based on MRI findings.
- Our team of specialists reviews MRI scans to diagnose shoulder impingement.
- Magnetic resonance imaging provides a clear understanding of the affected area.
Understanding Shoulder Impingement Syndrome

shoulder impingement syndrome
It’s important to understand shoulder impingement syndrome to diagnose and treat it. This condition happens when the shoulder blade presses on the tissues below, causing pain. It affects the shoulder joint and can lead to serious problems if not treated.
Definition and Pathophysiology
Shoulder impingement syndrome happens when the rotator cuff tendons get squished between the acromion and the humeral head. The pathophysiology involves a complex interplay of anatomical and biomechanical factors. It can be caused by inflammation, degeneration, and mechanical wear.
“The impingement syndrome is a painful condition that arises from the compression of rotator cuff tendons,” as noted by medical professionals. This compression can lead to tendonitis and, in severe cases, rotator cuff tears.
Common Causes and Risk Factors
Several factors contribute to shoulder impingement syndrome. These include repetitive overhead movements, anatomical variations, and conditions like osteoarthritis. Knowing these risk factors is key to preventing and managing the condition.
- Repetitive overhead activities
- Poor posture
- Muscle imbalances
- Anatomical variations
Understanding these causes helps in creating effective treatment plans. These plans can range from non-surgical methods to surgery.
Clinical Presentation of Shoulder Impingement
shoulder impingement symptoms
Knowing how shoulder impingement presents is key for right diagnosis and treatment. Shoulder impingement happens when the rotator cuff tendons rub against the joint. This causes pain and makes it hard to move the shoulder.
Common Symptoms and Signs
People with shoulder impingement feel pain, weakness, and can’t move their shoulder as much. The pain gets worse when they move their arm up. Symptoms can get worse over time.
Common symptoms include:
- Pain or aching in the shoulder, worse with overhead movements
- Weakness in the shoulder or arm
- Limited range of motion or stiffness
- Clicking or catching sensation in the shoulder
Physical Examination Findings
A detailed physical exam is vital for diagnosing shoulder impingement. We use tests to check how well the shoulder works and if there’s impingement. Key findings include:
Positive impingement signs, like the Neer test or Hawkins-Kennedy test. These tests check for pain when moving the arm. We also look for signs of rotator cuff problems, like muscle weakness.
| Clinical Test | Description | Positive Finding |
| Neer Test | Passive forward flexion of the arm | Pain or discomfort |
| Hawkins-Kennedy Test | Passive internal rotation with the arm flexed | Pain or discomfort |
MRI of Shoulder Impingement: Principles and Techniques
MRI shoulder impingement diagnosis
MRI is a key tool for diagnosing shoulder impingement. It shows the shoulder’s complex anatomy in detail. This helps us diagnose and plan treatment accurately.
How MRI Visualizes Shoulder Structures
MRI gives clear images of bones and soft tissues. It lets us see the shoulder’s detailed structures. This includes the rotator cuff tendons and the acromion, key for diagnosing impingement.
It uses a strong magnetic field and radio waves for images. T1-weighted and T2-weighted images are used to see different parts of the shoulder. T1 images show detailed anatomy, while T2 images spot problems like tendonitis.
Optimal MRI Protocols for Impingement Diagnosis
For accurate shoulder impingement diagnosis, specific MRI protocols are used. These focus on the most important structures for impingement.
| Protocol | Description | Benefits |
| T1-weighted sequences | Provide detailed anatomy | Helpful in assessing bone morphology and tendon integrity |
| T2-weighted sequences | Highlight fluid and pathology | Useful for detecting tendonitis, bursitis, and other inflammatory changes |
| Fat-suppressed sequences | Enhance visibility of pathology | Particularly useful for identifying edema and inflammation |
By mixing these MRI sequences, we get a full view of the shoulder. This helps us accurately diagnose impingement syndrome. The right protocol depends on the specific case and suspected issues.
Shoulder Impingement Syndrome Diagram: Anatomical Considerations
shoulder impingement anatomy
Shoulder impingement syndrome is complex and best shown through detailed diagrams. Knowing these details is key for diagnosing and treating it well.
Critical Anatomical Relationships
The shoulder joint has bones, tendons, and ligaments. The acromion, coracoid process, and rotator cuff tendons play a big role in this syndrome. Diagrams show how these parts work together and how they can cause impingement.
- The acromion and the humeral head create a narrow space. This can press on the rotator cuff tendons.
- The coracoid process can also press on soft tissues, like the subscapularis tendon.
- The rotator cuff tendons, like the supraspinatus, often get caught between the acromion and the humeral head.
Impingement Mechanisms Visualized
Diagrams and illustrations are key for seeing how impingement happens. They help doctors and patients grasp how certain movements or body parts can cause soft tissue compression.
- Subacromial impingement happens when the supraspinatus tendon gets squished between the acromion and the humeral head.
- Subcoracoid impingement occurs when the subscapularis tendon gets pressed between the coracoid process and the humerus.
- Internal impingement is when the rotator cuff tendons rub against the glenoid rim, common in athletes who throw overhead.
By looking at these diagrams, healthcare experts can create better treatment plans. These plans are made to meet the specific needs of each patient.
Subacromial Impingement MRI Findings
subacromial impingement mri findings
Subacromial impingement is a common shoulder issue. Knowing what MRI scans show is key to treating it well. We’ll look at the main MRI signs of subacromial impingement, from the first signs to more serious damage.
Early Stage Imaging Characteristics
In the early stages, MRI scans might show small changes in the rotator cuff tendons and bursae. MRI can spot tendon swelling, increased signal, and a bit of bursitis. These early signs are important for quick diagnosis and treatment.
Advanced Stage Pathological Changes
As subacromial impingement gets worse, MRI scans show more. Advanced changes include serious tendon damage, partial tears, and a lot of bursitis. MRI also shows changes in the acromion and coracoacromial ligament, which add to the impingement.
Associated Rotator Cuff Pathology
Subacromial impingement often goes hand in hand with rotator cuff problems. MRI is great for seeing how bad the rotator cuff damage is. It can show full-thickness tears, tendinosis, and muscle wasting. Knowing how impingement and rotator cuff damage are linked is key for treating it right.
| Stage | Key MRI Findings | Clinical Implications |
| Early Stage | Tendon swelling, increased signal intensity, minimal bursitis | Prompt diagnosis and conservative management |
| Advanced Stage | Significant tendon degeneration, partial-thickness tears, marked bursitis | Consideration of surgical intervention |
| Associated Rotator Cuff Pathology | Full-thickness tears, tendinosis, muscle atrophy | Comprehensive treatment planning, including possible surgery |
Subcoracoid Impingement Syndrome on MRI
subcoracoid impingement syndrome MRI
Healthcare professionals can now accurately diagnose subcoracoid impingement syndrome with MRI. This is a distinct clinical entity that needs specific criteria for diagnosis.
Subcoracoid impingement syndrome happens when the subscapularis tendon or nearby structures get pinched. This pinching occurs between the coracoid process and the lesser tuberosity of the humerus. It can cause a lot of shoulder pain and make it hard to move the shoulder.
Diagnostic Criteria and Measurements
To diagnose subcoracoid impingement syndrome on MRI, several criteria and measurements are used. These include:
- Abnormal narrowing of the coracohumeral interval
- Signal changes in the subscapularis tendon showing tendinopathy or tear
- Presence of subcoracoid bursitis or other soft tissue issues
Measuring the coracohumeral interval is key in diagnosing this condition. A smaller interval suggests possible impingement.
| Diagnostic Criterion | Description | Significance |
| Coracohumeral Interval | Distance between coracoid process and humerus | Narrowing indicates possible impingement |
| Subscapularis Tendon Signal | Changes in MRI signal of the tendon | Shows tendinopathy or tear |
| Subcoracoid Bursitis | Inflammation of the bursa between coracoid and humerus | Linked to subcoracoid impingement |
Differentiating Features from Other Pathologies
It’s important to tell subcoracoid impingement syndrome apart from other shoulder problems. Key differences include:
- Specific location of pain and tenderness
- Imaging findings like the coracohumeral interval and subscapularis tendon issues
- Clinical tests that bring on symptoms
A leading orthopedic expert says, “Accurate diagnosis of subcoracoid impingement syndrome needs both clinical assessment and imaging, like MRI.”
“The role of MRI in diagnosing subcoracoid impingement syndrome cannot be overstated. It gives vital info on anatomy and pathology.”
— Orthopedic Surgeon
Understanding the diagnostic criteria and differences of subcoracoid impingement syndrome on MRI helps healthcare providers. They can then offer more focused and effective treatments for those with this condition.
Internal Impingement: MRI Characteristics
internal impingement MRI
MRI is key in spotting internal impingement, a shoulder issue. It affects the shoulder’s inner parts, causing pain, mainly in athletes. This is common in those who play overhead sports.
We’ll look at how MRI helps find internal impingement types. This includes posterior superior and anterior internal impingement patterns.
Posterior Superior Impingement Findings
Posterior superior impingement happens when rotator cuff tendons rub against the glenoid’s top back. MRI shows abnormal contact between the rotator cuff and the glenoid. This can damage tendons and cause pain.
Key MRI features include:
- Partial-thickness rotator cuff tears
- Superior labral lesions
- Bone marrow edema in the humeral head or glenoid
Anterior Internal Impingement Patterns
Anterior internal impingement affects the shoulder’s front parts. MRI helps see anatomical abnormalities like subscapularis tendon lesions and anterior labral tears.
The diagnostic accuracy of MRI in anterior internal impingement is high. It shows the extent of damage, helping doctors decide on treatment.
Comparing Shoulder Impingement X-Ray vs. MRI
Diagnosing shoulder impingement can be done through X-rays and MRI. Each method has its own benefits and drawbacks when it comes to shoulder impingement syndrome.
What X-Rays Can and Cannot Show
X-rays are often the first choice for shoulder problems, like impingement syndrome. They’re great for seeing bones, finding calcifications, and checking the space between the acromion and humerus. But, they can’t show soft tissues like tendons, ligaments, or the rotator cuff, which are key in impingement syndrome.
X-rays might show signs of impingement indirectly, such as:
- Sclerosis or cystic changes in the humeral head
- Acromial spurs
- Reduced acromiohumeral distance
Even with these abilities, X-rays can’t show the soft tissue damage often seen in impingement syndrome.
When to Progress from X-Ray to MRI
We usually move from X-rays to MRI when:
- Symptoms don’t get better with treatment
- X-rays don’t show anything clear, even with bad symptoms
- There’s a strong belief in soft tissue or rotator cuff damage
MRI gives a detailed look at both bones and soft tissues. It offers a fuller view of the shoulder’s anatomy and problems.
Complementary Value of Both Modalities
X-rays and MRI work together in diagnosing. They each have their own strengths:
| Diagnostic Feature | X-Ray | MRI |
| Bone Structures | Excellent for detecting fractures, calcifications, and bone spurs | Good for assessing bone marrow edema and occult fractures |
| Soft Tissue | Limited, cannot visualize tendons, ligaments, or rotator cuff directly | Excellent for evaluating tendons, ligaments, and rotator cuff pathology |
| Impingement Diagnosis | Indirect signs, such as acromial spurs and reduced acromiohumeral distance | Direct visualization of impingement and associated soft tissue pathology |
Knowing what X-rays and MRI can do helps doctors choose the best imaging for shoulder impingement syndrome.
Shoulder Impingement Imaging: Ultrasound and CT Alternatives
MRI is key for diagnosing shoulder impingement. But, ultrasound and CT arthrography also give valuable insights. They can show things MRI might miss, helping doctors make better diagnoses.
Dynamic Ultrasound Assessment
Dynamic ultrasound is great for checking shoulder impingement. It lets us see the shoulder and its parts moving in real time. This is useful for spotting impingement that happens only when moving a certain way.
Key benefits of dynamic ultrasound assessment include:
- Real-time visualization of shoulder movement
- Ability to assess impingement during dynamic movements
- Non-invasive and relatively low-cost compared to other imaging modalities
We use dynamic ultrasound to watch the subacromial space and check for impingement as the arm moves. It’s very helpful for diagnosing subacromial impingement syndrome.
CT Arthrography Applications
CT arthrography is also a top tool for diagnosing shoulder impingement. It involves putting contrast material in the shoulder joint before scanning. This method gives clear images of the joint and can spot small issues.
Advantages of CT arthrography include:
| Feature | Benefit |
| High-resolution images | Detailed visualization of joint structures |
| Contrast material | Enhances visibility of abnormalities |
| Ability to detect subtle lesions | Helps in early diagnosis and treatment planning |
We turn to CT arthrography for detailed shoulder joint checks. This is when MRI isn’t an option or when we need clear images of bones.
How to Diagnose Shoulder Impingement with MRI
Understanding MRI scans is key to diagnosing shoulder impingement. We’ll show you how to do it right. You’ll learn about important signs and measurements for a correct diagnosis.
Systematic Approach to Image Interpretation
When we look at MRI scans for shoulder impingement, we follow a set plan. This includes:
- Looking at the patient’s history and symptoms.
- Searching for signs of impingement like tendonitis or bursitis on the MRI.
- Measuring the subacromial space to see if it’s too narrow.
A top orthopedic expert says, “A detailed MRI analysis is vital for diagnosing shoulder impingement and treatment planning.”
“MRI has changed how we diagnose shoulder impingement by showing us soft tissue problems clearly.”
Key Diagnostic Features and Measurements
Important signs on MRI include:
| Feature | Description | Significance |
| Tendon Thickening | Tendons get thicker due to long-term inflammation. | Shows tendonitis, a common shoulder impingement issue. |
| Subacromial Space Narrowing | The space between the acromion and humeral head gets smaller. | Points to impingement from mechanical pressure. |
| Bursitis | The bursa gets inflamed, seen as fluid on MRI. | Linked to impingement syndrome. |
Grading Systems for Impingement Severity
There are grading systems to measure how severe shoulder impingement is on MRI. These systems help standardize diagnosis and guide treatment.
Grading System Example:
- Grade 1: Mild impingement with little tendon damage.
- Grade 2: Moderate impingement with more tendon issues.
- Grade 3: Severe impingement with big tendon damage or rupture.
By using a systematic MRI approach and grading systems, we improve diagnosis accuracy. This leads to better treatment plans for shoulder impingement.
MRI Shoulder Impingement Diagnosis: Accuracy and Limitations
MRI is a key tool for diagnosing shoulder impingement. It gives detailed insights into the condition. But, it’s important to know its limits.
Sensitivity and Specificity Statistics
Research shows MRI is very good at spotting shoulder impingement. It can detect rotator cuff tears with 80% to 90% accuracy. Its specificity is also high, usually over 90%. But, results can change based on the MRI method and the radiologist’s skill.
“MRI has greatly helped us diagnose shoulder impingement better,” says a top orthopedic expert. “But, it’s key to match imaging with what the patient feels.”
Common Diagnostic Pitfalls
Even with its strengths, MRI has its challenges in diagnosing shoulder impingement. Some common issues include:
- Misreading normal body variations as problems
- Missing small signs of impingement
- Not considering the patient’s symptoms
To avoid these problems, it’s vital to interpret images carefully. We must look at both the images and the patient’s symptoms.
When MRI May Miss Impingement
There are times when MRI might not catch shoulder impingement or related issues. These include:
- Early stages of impingement where changes are not yet seen on MRI
- Dynamic impingement that happens only during specific movements not shown by static MRI
- Technical problems like bad MRI sequences or artifacts
In these cases, other imaging methods like dynamic ultrasound or checking the patient’s symptoms might be needed to confirm the diagnosis.
In summary, MRI is a powerful tool for diagnosing shoulder impingement. But, knowing its strengths and weaknesses is key for the best care of patients.
Correlating Clinical Findings with MRI Results
It’s key to link clinical findings with MRI results for shoulder impingement syndrome management. We need to look at both the symptoms and the MRI findings. This helps us give our patients the best care.
Importance of Clinical Context
Knowing the clinical context is vital when we look at MRI results. This includes the patient’s symptoms, medical history, and physical exam results. With this info, we can understand MRI findings better and make accurate diagnoses.
For example, a patient with shoulder pain and limited movement might show impingement on MRI. But, if they’ve had trauma or repetitive strain, their history might point to something else.
Key Factors in Clinical Context:
- Patient symptoms and history
- Physical examination findings
- Previous treatments or interventions
Managing Discrepancies Between Symptoms and Imaging
There can be times when symptoms don’t match MRI findings. For instance, a patient might have a lot of shoulder pain but little impingement on MRI. We then need to look at other possible reasons for their pain, like referred pain or other conditions.
Handling these differences needs a detailed approach. This includes more clinical checks, extra imaging if needed, and exploring other treatment options.
| Clinical Finding | MRI Finding | Potential Action |
| Significant shoulder pain | Minimal evidence of impingement | Further clinical evaluation, consider other causes of pain |
| Limited mobility | Evidence of rotator cuff tear | Surgical consultation, physical therapy |
A leading orthopedic specialist says, “The key to managing shoulder impingement syndrome is linking clinical findings with MRI results. We must also consider the broader clinical context.”
“Correlation between clinical assessment and imaging is key for accurate diagnosis and effective treatment planning.”
Orthopedic Specialist
Treatment Planning Based on MRI Findings
When treating shoulder impingement, MRI findings are key. They help us see how bad the impingement is and if there are other problems like rotator cuff tears or tendonitis.
Conservative Management Indicators
For many, the first step is conservative management. MRI helps us see who will do well with this approach. Indicators for conservative management include:
- Mild to moderate impingement
- Minimal rotator cuff involvement
- Absence of significant tendon degeneration
Conservative management includes physical therapy, anti-inflammatory meds, and lifestyle changes. The goal is to lessen symptoms and improve function without surgery.
Surgical Decision-Making
If conservative methods don’t work or the impingement is severe, surgery might be needed. MRI findings are key in deciding if surgery is right. They help us:
- Check how bad the rotator cuff damage is
- See if there are other problems that need fixing
- Plan the best surgery
Surgical options include arthroscopic decompression, rotator cuff repair, or other procedures to fix the impingement and damaged tissues.
Prognostic Value of MRI Findings
MRI findings help us decide on treatment and predict outcomes. They show how bad the impingement and other problems are. This lets us tailor our treatment plans better.
The value of MRI findings is huge for patient counseling. It helps set realistic recovery goals and guides the rehab process.
Advanced MRI Techniques for Shoulder Impingement Radiology
Advanced MRI techniques are changing how we look at shoulder impingement. These new tools help us diagnose and treat shoulder impingement better.
Dynamic and Functional MRI Applications
Dynamic and functional MRI are becoming key in shoulder impingement checks. They show how the shoulder moves, giving us a clearer picture of the problem.
Benefits of Dynamic MRI:
- Improved visualization of impingement in different arm positions
- Better assessment of dynamic instability
- Enhanced evaluation of rotator cuff function
Artificial Intelligence in Impingement Detection
Artificial intelligence (AI) is now part of MRI for shoulder impingement. AI helps spot small issues and measure how bad the impingement is.
| AI Application | Description | Benefit |
| Automated Detection | AI algorithms detect impingement and related pathologies | Improved diagnostic accuracy |
| Quantitative Analysis | AI quantifies the severity of impingement | Enhanced treatment planning |
| Image Enhancement | AI enhances image quality for better visualization | Better assessment of shoulder anatomy |
Using these advanced MRI methods, we can better diagnose and treat shoulder impingement. This leads to better care for our patients.
Conclusion
We’ve looked into how MRI helps diagnose shoulder impingement syndrome. This is a common issue in the shoulder joint. MRI lets doctors see the shoulder’s structures clearly, helping them find the cause of the problem.
MRI images are key in diagnosing shoulder impingement. They help doctors see the shoulder’s details. This information helps them make the right treatment plans for patients.
In short, MRI is a key tool for diagnosing shoulder impingement. It gives doctors a detailed look at the shoulder. This helps them create better treatment plans, improving patients’ lives.
FAQ
What is shoulder impingement syndrome?
Shoulder impingement syndrome is a condition where the tendons or bursae in the shoulder joint become inflamed or irritated. This causes pain and limited mobility.
How is shoulder impingement diagnosed using MRI?
MRI is a key tool for diagnosing shoulder impingement. It gives detailed images of the shoulder joint and surrounding tissues. Our team reviews the MRI scan to create a personalized care plan.
What are the common symptoms of shoulder impingement?
Symptoms include pain, weakness, and limited mobility in the shoulder joint.
Can X-rays diagnose shoulder impingement?
X-rays can be used first to check for shoulder impingement. But MRI is more accurate for diagnosing it.
What is the difference between subacromial and subcoracoid impingement?
Subacromial impingement happens when the tendons or bursae get inflamed under the acromion. Subcoracoid impingement occurs under the coracoid process.
How does MRI help in diagnosing subcoracoid impingement syndrome?
MRI shows detailed images of the shoulder joint and surrounding tissues. It helps see diagnostic criteria and measurements for subcoracoid impingement syndrome.
What is internal impingement, and how is it diagnosed using MRI?
Internal impingement is a complex condition where the tendons or labrum get inflamed or irritated inside the shoulder joint. MRI can spot this by showing posterior superior impingement findings and anterior internal impingement patterns.
What are the advantages of using MRI over other imaging modalities for shoulder impingement?
MRI gives detailed images of the shoulder joint and surrounding tissues. It’s great for seeing soft tissue structures and spotting subtle abnormalities.
Can MRI detect all types of shoulder impingement?
MRI is very useful for diagnosing shoulder impingement. But it might not catch all types. It’s important to consider the clinical context and symptoms for accurate diagnosis.
How do MRI findings influence treatment planning for shoulder impingement?
MRI findings are key in planning treatment for shoulder impingement. Our team uses MRI findings to create a customized care plan. This might include conservative management or surgery.
What are the emerging trends in MRI technology for diagnosing shoulder impingement?
New MRI techniques, like dynamic and functional MRI, and artificial intelligence, are becoming important tools. They help in diagnosing and managing shoulder impingement.
Reference:
Sadeghian, H. (2018). Pitting Oedema in a Patient with Lumbar Disc Herniation. PMC.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5766305
Dydyk, A. M., et al. (2023). Disk Herniation – StatPearls. PMC.




































