Dislocations are a big deal in both medical and scientific fields, affecting millions globally. A dislocation happens when a joint is pushed out of its usual spot. This can lead to serious issues if not fixed quickly. We’ll look into the two main types of dislocations: anterior and posterior. We’ll also see how complete and partial dislocations differ. Discover the two main types of dislocations, their symptoms, and best treatments.
It’s key to know the details of these injuries to treat them right. Our talk will give you the lowdown on causes, signs, and how to fix different dislocations.
Key Takeaways
- Dislocations occur when a joint is forced out of its normal position.
- The two fundamental types are complete and partial dislocations.
- Dislocations can be classified as complete or partial.
- Understanding the type of dislocation is key for good treatment.
- Treatment options change based on how bad and what kind of dislocation it is.
Understanding Dislocations: Definition and Basic Concepts
A dislocation happens when bones in a joint move out of place. This can cause pain and make it hard to move. Knowing what a dislocation is and how it affects people is key. We’ll look at what happens during a dislocation and how it’s different from other joint problems.
What Happens During a Dislocation?
When a dislocation occurs, the bones in a joint move out of their usual spot. This can hurt the ligaments, tendons, and nerves around them. It can happen from accidents, falls, or sports injuries. The extent of the dislocation can vary, from a partial one to a complete one where the bones are fully out of place.
Key aspects of dislocations include:
- Displacement of bones from their normal alignment
- Potential damage to surrounding tissues
- Variability in severity, from partial to complete dislocation
Difference Between Dislocations and Other Joint Injuries
Dislocations are different from other joint injuries like sprains or strains. Sprains and strains hurt ligaments or muscles but don’t move bones. Knowing the difference helps doctors diagnose and treat correctly. For example, a subluxation is a partial bone move, while a complete dislocation means the bones are fully separated.
We need to remember these key differences:
- Dislocations involve bone displacement, unlike sprains or strains.
- Subluxations are partial dislocations, differing from complete dislocations.
- The severity and impact of dislocations can vary widely among individuals.
The Two Fundamental Types of Dislocations
Knowing the two main types of dislocations is key for proper treatment. Dislocations can happen from accidents, falls, or sports injuries. They are mainly split into two based on how much the joint is out of place.
Complete Dislocations: When Bones Fully Separate
A complete dislocation means the bones of a joint are completely out of place. This is a serious issue causing a lot of pain, swelling, and trouble moving. It often happens in high-impact sports or severe accidents and needs quick medical help.
Partial Dislocations (Subluxations): Partial Joint Displacement
Partial dislocations, or subluxations, mean the bones are only partially out of place. This can be as painful and limiting as a complete dislocation. Symptoms include feeling the joint is unstable or “off.”
It can be hard to spot partial dislocations on X-rays. A doctor must do a detailed check to diagnose them.
Key Differences in Symptoms and Treatment
The signs and treatments for complete and partial dislocations differ a lot. Complete dislocations have more severe symptoms like deformity and can’t move the joint. Partial dislocations might have milder symptoms but need medical check-up too.
Treatment depends on how bad and what type of dislocation it is. Some might just need to be put back in place and immobilized. Others might need surgery to fix the joint and any damaged tissues. Knowing these differences helps in giving the right care.
Every patient is different, so treatments are made to fit their needs. This ensures the best results for those with complete or partial dislocations.
Directional Classification of Types of Dislocations
Dislocations are classified by their direction to understand the injury better. This helps in choosing the right treatment. The direction of displacement is key to knowing the injury’s severity and how to manage it.
Anterior Dislocations: Causes and Characteristics
Anterior dislocations happen when a bone moves forward. They are common in the shoulder and hip. Anterior shoulder dislocations often come from falling onto an outstretched hand or a direct hit to the shoulder. The signs of anterior dislocations include:
- Visible deformity
- Pain and swelling
- Limitation of movement
These dislocations can be caused by injuries, like those in sports or car accidents. Knowing how the injury happened is important for diagnosis.
Posterior Dislocations: Mechanisms and Features
Posterior dislocations happen when a bone moves backward. They are less common but can be very serious. Posterior shoulder dislocations can be caused by seizures, electric shock, or direct trauma. The signs of posterior dislocations include:
- Prominent posterior aspect of the joint
- Shortening of the limb
- Significant pain and limited mobility
Posterior dislocations usually need a lot of force or trauma. A detailed check-up and imaging are needed for diagnosis.
Other Directional Types: Superior, Inferior, and Lateral
There are other types of dislocations, like superior, inferior, and lateral. These are less common but can happen in different joints.
Superior dislocations are rare and involve moving upward. They are often linked to severe trauma. Inferior dislocations move downward and can be seen in some shoulder or hip injuries. Lateral dislocations move sideways and can happen in the shoulder, hip, and knee.
Knowing about these different types is key for correct diagnosis and treatment. Each type has its own causes, signs, and treatment plans.
Causes and Mechanisms of Joint Dislocations
Looking into why joint dislocations happen helps us prevent and treat them. These injuries are complex and can come from many sources.
Traumatic Causes: Accidents, Falls, and Sports Injuries
Many joint dislocations come from accidents, falls, and sports injuries. These events apply a lot of force to the joint. For example, falling on an outstretched hand can dislocate the shoulder. A direct hit to the knee can dislocate the patella.
Sports injuries, and contact sports in particular, raise the risk of dislocations. Knowing how these injuries happen helps us find ways to prevent them.
| Traumatic Cause | Common Dislocation Type | Mechanism of Injury |
| Falls | Shoulder Dislocation | Fall onto outstretched hand |
| Sports Injuries | Knee Dislocation | Direct blow to the knee |
| Accidents | Multiple Types | Varies with the nature of the accident |
Non-Traumatic Causes: Joint Laxity and Medical Conditions
Not all dislocations are from accidents. Joint laxity and certain medical conditions can also cause them. Joint laxity means the joint is loose or unstable. It can be due to genetics or conditions like Ehlers-Danlos syndrome.
Medical issues like rheumatoid arthritis or neurological disorders can also increase the risk of dislocations. Knowing about these conditions is key to managing and preventing dislocations.
Congenital Factors Leading to Dislocations
Congenital factors can also cause joint dislocations. Conditions like developmental dysplasia of the hip (DDH) are present at birth. They can lead to joint instability and dislocation.
Early diagnosis and treatment are vital for managing congenital dislocations. This can greatly improve outcomes and lower the risk of long-term problems.
By understanding the causes and mechanisms of joint dislocations, we can create better prevention, diagnosis, and treatment plans. This will help improve patient outcomes.
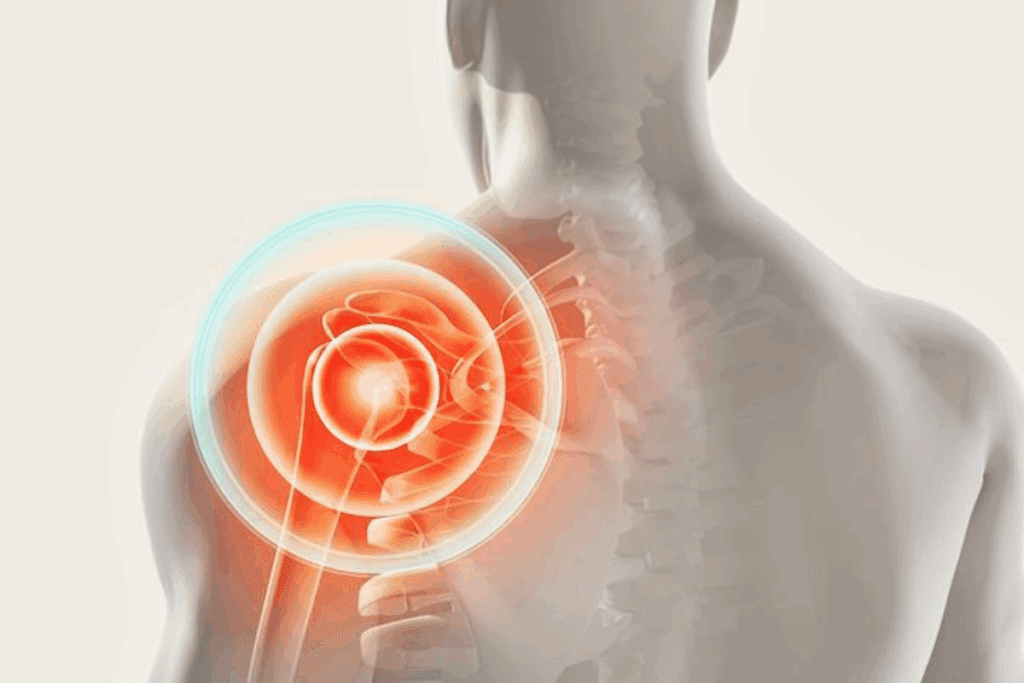
Shoulder Dislocations: The Most Common Type
Understanding shoulder dislocations is key for effective treatment and recovery. The shoulder joint is very mobile but also unstable. This makes it prone to dislocations.
Anterior vs. Posterior Shoulder Dislocations
Shoulder dislocations are mainly of two types: anterior and posterior. Anterior shoulder dislocations are more common, making up about 95% of cases. They happen when the arm is lifted, rotated outward, and extended.
Posterior shoulder dislocations are less common. They can occur from seizures, electric shock, or direct trauma to the front of the shoulder.
The symptoms and presentation vary between types. Anterior dislocations often have the arm in abduction and external rotation. Posterior dislocations have the arm in internal rotation and adduction.
Treatment Options for Dislocated Shoulders
The first step in treating a dislocated shoulder is reduction. This is when the humerus is put back into its normal position. There are several reduction techniques, like the Stimson, external rotation, and Milch methods. The choice depends on the patient’s condition and the doctor’s preference.
After reduction, immobilization is often needed. This allows the injured tissues to heal. The length of immobilization varies based on the dislocation’s severity and the patient’s health.
- Simple sling immobilization for comfort and support
- Pain management through medication
- Early mobilization and physical therapy to regain range of motion and strength
Recovery Timeline and Rehabilitation
The recovery timeline for shoulder dislocations varies. It depends on the injury’s severity, treatment success, and rehabilitation adherence. The recovery process has several phases:
- Immediate post-reduction phase (0-2 weeks): Focus on pain management and initial healing
- Early rehabilitation phase (2-6 weeks): Gradually introduce exercises to improve range of motion and strengthen the shoulder muscles
- Advanced strengthening phase (6-12 weeks): Progress to more intense strengthening exercises and functional activities
Rehabilitation is vital for recovery. It aims to restore function, prevent recurrence, and improve shoulder stability. A tailored rehabilitation program is essential for the best outcomes.
Hip Dislocation: A Serious Medical Emergency
A dislocated hip joint is a serious issue that needs quick and effective treatment. This is to avoid long-term problems. Hip dislocations happen when the femur head moves out of the acetabulum. This often occurs due to severe trauma, like in car accidents or falls.
Types of Hip Dislocations
Hip dislocations are divided into two main types: anterior and posterior. Each type is based on the direction of the dislocation.
- Posterior Hip Dislocations: These are the most common, making up 80-90% of cases. They happen when the knee hits the dashboard in a car crash, pushing the femur head backward.
- Anterior Hip Dislocations: Less common, these occur when the hip is flexed, abducted, and rotated outward. They are often seen in sports injuries.
As An orthopedic surgeon, notes,
“Prompt reduction of a dislocated hip is key to avoid complications like avascular necrosis of the femoral head.”
Associated Complications and Injuries
Hip dislocations can lead to several complications, including:
- Femoral head fractures
- Acetabular fractures
- Nerve injuries, like to the sciatic nerve
- Vascular injuries
These issues can greatly affect treatment and long-term results for the patient.
Treatment Protocols and Long-term Outcomes
The first step in treating a hip dislocation is to immediately reduce it. This is done to restore the hip’s normal shape. It’s usually done under sedation or anesthesia to reduce pain.
After the reduction, care includes:
- Immobilization to help the healing process
- Pain management
- Physical therapy to improve strength and mobility
- Follow-up imaging to check for complications like avascular necrosis
Long-term results depend on the injury’s severity and any complications. With the right treatment, many patients can recover well. But, some may face long-term problems like post-traumatic arthritis.
Knee Dislocations: Complex and Dangerous
Knee dislocations are complex and can lead to serious complications. They often happen due to high-energy accidents or sports injuries. These injuries can cause damage to blood vessels and nerves, making quick and proper treatment key.
Types of Knee Dislocations and Their Severity
Knee dislocations are classified based on the direction and severity of the injury. The most common classification is by the tibial displacement relative to the femur. Knowing the type and severity helps doctors choose the right treatment.
The severity of knee dislocations can vary. They range from partial dislocations to complete dislocations. Doctors use classification systems to guide treatment and predict outcomes.
Vascular and Nerve Complications
Knee dislocations pose a high risk of vascular and nerve damage. The popliteal artery is at risk due to its fixed position near the knee. Vascular injuries can cause limb ischemia, needing immediate treatment.
Nerve injuries, like those to the peroneal nerve, are common. These injuries can lead to loss of motor function and sensation. Quick evaluation and treatment are vital for the best outcomes.
Surgical and Non-surgical Management
The treatment for knee dislocations depends on the injury’s severity and complications. Initial steps include reducing the dislocation and immobilizing the knee. Then, doctors check for vascular and nerve damage.
Surgery is needed for complex dislocations, like those with fractures or soft tissue injuries. Surgery may involve ligament reconstruction, vascular repair, and nerve management.
For less severe dislocations or those without complications, non-surgical treatment is considered. This includes immobilization followed by rehabilitation to improve knee function and strength.
Other Common Joint Dislocations
Dislocations can happen in many joints like the elbow, wrist, ankle, and jaw. These injuries need quick and right treatment to avoid lasting harm and get function back.
Elbow Dislocation Types and Management
Elbow dislocations are common and can be split into several types. Posterior dislocations are the most common. They often happen when you fall onto an outstretched hand.
Managing elbow dislocations starts with reduction, then immobilization and rehab. We also check for fractures or nerve damage, which can make treatment harder.
Wrist and Finger Dislocations
Wrist and finger dislocations can really affect hand use. Wrist dislocations often come from big traumas, like falling from a height or a car crash.
Finger dislocations, like at the PIP joint, are common in sports. Getting the finger back in place is easy, but keeping it there and dealing with other injuries is key.
Ankle and Foot Dislocations
Ankle and foot dislocations can be tricky and often come with fractures. Ankle dislocations usually happen from big injuries, like in sports or car accidents.
Foot dislocations, like in the midfoot or toes, need quick fixing to avoid problems like compartment syndrome.
Jaw (Temporomandibular Joint) Dislocations
Jaw dislocations, or TMJ dislocations, can be sudden or keep happening. They often happen from yawning, laughing, or during dental work.
Fixing jaw dislocations involves special techniques, like the Nelson maneuver. Then, eating soft foods and taking steps to stop it from happening again is important.
Diagnosis of Different Dislocation Types
Healthcare professionals use many methods to diagnose dislocations. They start with physical exams and then use advanced imaging. Knowing the type and severity of a dislocation helps choose the right treatment.
Physical Examination Techniques
A detailed physical exam is the first step. We look for signs of injury like deformity, swelling, and bruising. We also check how well the joint moves and how much pain it causes.
Special tests are done to see if the joint is stable. For example, we might do an anterior apprehension test for shoulder dislocations. This test checks if the shoulder might slip out again.
Imaging Methods: X-rays, CT Scans, and MRIs
Imaging studies are key to confirming a dislocation diagnosis. X-rays are often the first choice because they quickly show if a dislocation is present. Computed Tomography (CT) scans give more detailed images, which are helpful for complex cases.
Magnetic Resonance Imaging (MRI) is great for soft tissue injuries like sprains or tendon ruptures. It can also spot fractures that X-rays miss.
Differential Diagnosis Considerations
When diagnosing dislocations, we must think of other possible causes. This includes fractures, sprains, or soft tissue injuries. A detailed differential diagnosis ensures the right treatment is started.
We also look for injuries like nerve or vascular damage. These can change the treatment plan and outcome. A full assessment, including exams and imaging, is needed to find these injuries.
Emergency Management and Reduction Procedures
When a dislocation happens, acting fast is key. The right emergency care can help avoid more harm and aid in healing.
First Aid Approaches for Various Dislocations
First aid for dislocations means keeping the joint steady, using ice to lessen swelling, and getting medical help right away. For shoulder dislocations, it’s important to use a sling to support the arm. Hip dislocations need careful handling to prevent more damage, often requiring quick transport to a hospital.
For elbows, wrists, or ankles, using a splint or bandage can prevent more injury. It’s also vital to watch for signs of nerve or blood vessel problems, like numbness or tingling.
Medical Reduction Techniques
Medical methods to fix dislocations vary based on the type and how bad it is. For simple cases, closed reduction might be used, where the bones are gently moved back into place without surgery. This is usually done while the patient is sedated or under anesthesia to reduce pain.
For more serious cases, open reduction might be needed, which is a surgery to align and stabilize the bones. The choice between these methods depends on the dislocation’s details and the patient’s health.
| Dislocation Type | Common Reduction Technique | Key Considerations |
| Shoulder Dislocation | Closed reduction | Often requires sedation; post-reduction X-rays are essential |
| Hip Dislocation | Closed or open reduction | Urgent reduction is necessary to prevent complications like avascular necrosis |
| Elbow Dislocation | Closed reduction | Careful assessment for associated fractures or neurovascular injury |
Post-Reduction Care and Monitoring
After fixing the dislocation, keeping the joint steady is vital for healing. How long the joint needs to be immobilized depends on the joint and the dislocation’s severity. Managing pain is also important, often through medication and physical therapy.
It’s critical to watch for any complications, like nerve or blood vessel damage. Regular check-ups with healthcare providers are needed to track healing and address any issues.
Comprehensive care after the reduction is essential for the best recovery and to avoid long-term problems.
Treatment Options Based on Dislocation Severity
Knowing how severe a dislocation is is key to picking the right treatment. The severity helps doctors decide between non-surgical methods, surgery, and pain relief plans.
Conservative Management for Simple Dislocations
For mild dislocations, doctors often choose non-surgical treatment. This method involves manually moving the bones back into place without surgery.
Key components of conservative management include:
- Immobilization to allow healing
- Pain management through medication
- Physical therapy to regain strength and mobility
- Follow-up care to monitor recovery
Surgical Interventions for Complex Dislocations
For severe dislocations, surgery is often needed. Surgery aims to fix the joint, repair damaged tissues, and keep the joint stable.
Surgical techniques may include:
- Open reduction to directly visualize and repair the joint
- Internal fixation using pins, screws, or plates to stabilize bones
- Soft tissue repair or reconstruction
| Treatment Aspect | Conservative Management | Surgical Intervention |
| Simple Dislocations | Preferred for simple cases | Reserved for complex cases |
| Complex Dislocations | May not be sufficient | Necessary for restoring joint anatomy |
| Recovery Time | Typically shorter | Generally longer due to surgical recovery |
Pain Management Strategies
Managing pain is vital in treating dislocations, whether with or without surgery. Pain relief plans may include medicines, physical therapy, and other treatments.
Pain management options include:
- Oral analgesics for pain relief
- Physical therapy to improve joint mobility and strength
- Modalities such as ice, heat, or electrical stimulation
The Healing Process and Recovery Timeline
Recovering from a dislocation takes time and involves different stages. Each stage has its own challenges and goals. Knowing these stages helps patients recover better.
Immediate Post-Reduction Phase (0-2 weeks)
Right after a dislocation is fixed, the main goal is to manage pain and keep the joint stable. Patients are told to rest and might get pain meds.
It’s important to watch for any signs of trouble, like more pain, swelling, or numbness. Always follow up with your doctor as they suggest.
Intermediate Recovery (2-6 weeks)
Once the pain starts to go away, patients start a rehab program. This helps them get their strength, flexibility, and movement back. It’s a key time to avoid stiffness and get the joint working right again.
Physical therapy is a big part of this phase. They do exercises that match the joint and the type of dislocation.
Long-term Rehabilitation (6+ weeks)
The final phase is about getting back to full activity, like sports or hard work. Patients keep doing strengthening exercises and might need to change how they do things to avoid dislocations again.
It’s vital to keep seeing your healthcare team. They check on your healing and help with any issues or worries.
| Recovery Phase | Timeline | Key Activities |
| Immediate Post-Reduction | 0-2 weeks | Pain management, immobilization |
| Intermediate Recovery | 2-6 weeks | Rehabilitation, physical therapy |
| Long-term Rehabilitation | 6+ weeks | Strengthening, return to activity |
Complications Associated with Different Dislocation Types
Dislocations can lead to many complications that affect the joint and tissues around it. It’s important to know about these issues to manage and prevent them effectively.
Nerve and Vascular Damage
Nerve and vascular damage are serious problems right after a dislocation. The nerves and blood vessels near the joint can get stretched or torn. This can cause a lot of pain and problems.
For example, a posterior shoulder dislocation can hurt the axillary nerve. Knee dislocations often damage the popliteal artery. It’s critical to treat these problems quickly to avoid lasting harm.
| Dislocation Type | Nerve/Vascular Damage Risk | Common Complications |
| Posterior Shoulder Dislocation | Axillary nerve damage | Numbness, weakness in deltoid muscle |
| Knee Dislocation | Popliteal artery injury | Ischemia, limb loss if untreated |
| Hip Dislocation | Sciatic nerve damage | Numbness, weakness in lower limb |
Recurrent Dislocations and Joint Instability
Dislocations can also make joints more likely to dislocate again. This is because the structures that keep the joint stable can get damaged.
Shoulder dislocations often lead to more problems because of a Bankart lesion. Surgery is often needed to fix this and prevent more dislocations.
Arthritis and Long-term Joint Degeneration
Dislocations can also cause long-term damage to joints, leading to arthritis. The injury from a dislocation can start a chain of problems in the joint.
Hip dislocations can cause the femoral head to die, leading to severe arthritis. Knowing these risks helps us manage patient care and rehabilitation better.
When treating dislocations, we must think about these complications. This way, we can give our patients the best care and help them avoid long-term problems.
Prevention Strategies for High-Risk Individuals
People who take part in risky activities, like the EBC Trek, can lower their dislocation risk. We suggest a mix of protective gear, joint exercises, and changing how they do activities.
Protective Equipment for Athletes
Athletes in contact sports or risky activities can cut their dislocation risk with the right gear. This includes:
- Knee and elbow pads for sports like football, hockey, or skateboarding
- Shoulder pads for American football players
- Helmets for cycling, motorcycling, or other high-speed activities
Wearing the right gear can help absorb shock and lessen joint stress, lowering dislocation risk.
Joint Stabilization Exercises
Strengthening muscles around a joint can add stability and lower dislocation risk. We suggest exercises that target the muscles around the joint. For example:
- For shoulder stability, exercises like shoulder rotations and scapular squeezes can be beneficial
- For knee stability, squats, lunges, and leg press exercises can strengthen the surrounding muscles
It’s key to work with a healthcare pro or physical therapist to create a tailored exercise plan.
Activity Modifications and Technique Training
Changing how you do activities or learning new techniques can also help prevent dislocations. This includes:
- Learning proper falling techniques to reduce the impact on joints
- Avoiding activities that involve heavy lifting or bending
- Using proper body mechanics during sports or physical activities
Learning safe movement techniques can help reduce dislocation risk.
By using these prevention strategies, high-risk individuals can lower their dislocation risk. We advise talking to healthcare experts to create a personalized prevention plan.
Special Population Considerations
Caring for dislocations in special groups like children, older adults, and those with connective tissue disorders needs special care. Each group faces unique challenges because of their health and how their bodies work.
Pediatric Dislocations and Growth Plate Concerns
Dislocations in kids are a big worry because of their growth plates. These areas are key for bone growth, and injuries can cause lasting problems if not treated right.
Key Considerations for Pediatric Dislocations:
- Accurate diagnosis to identify growth plate injuries
- Gentle reduction techniques to avoid further damage
- Monitoring for growth disturbances
Dislocations in Elderly Patients with Osteoporosis
Elderly people, and those with osteoporosis, are more likely to have dislocations. This is because their bones are weaker and more fragile. Treating dislocations in this group needs careful thought about their bone health.
| Challenge | Management Strategy |
| Osteoporotic bones | Use of gentle reduction techniques, avoidance of heavy immobilization |
| Comorbid conditions | Coordination with other healthcare providers to manage overall health |
| Rehabilitation challenges | Tailored physical therapy programs to accommodate physical limitations |
Managing Dislocations in Patients with Connective Tissue Disorders
People with connective tissue disorders, like Ehlers-Danlos syndrome, face special challenges. Their joints are loose and tissues are fragile. Treatment plans need to be made just for them.
Key management strategies include:
- Personalized treatment plans considering the specific connective tissue disorder
- Use of supportive devices to enhance joint stability
- Physical therapy focused on improving muscle strength around the affected joint
Conclusion: Understanding and Managing Dislocations
Managing dislocations well is key to fixing joint problems and easing pain. Knowing about dislocations is the first step. This article has covered the different kinds, why they happen, how to find out, and how to treat them.
Dislocations can happen in many joints, each with its own issues. Shoulder dislocations are the most common. Hip dislocations are emergencies. Knee dislocations are complex and can be dangerous.
Handling dislocations right means quick diagnosis and the right treatment. Knowing how injuries happen and what each dislocation is like helps doctors plan better. This includes non-surgical and surgical options.
The success of managing dislocations depends on really understanding them. With this knowledge, doctors can help patients more and lower the chance of future problems.
FAQ
What is a dislocation?
A dislocation happens when a bone moves out of its joint. This causes pain, swelling, and makes it hard to move.
What are the two fundamental types of dislocations?
There are two main types of dislocations. Complete dislocations mean the bones are fully apart. Partial dislocations, or subluxations, mean the bones are only slightly out of place.
What is the difference between a dislocation and a subluxation?
A dislocation means a bone is completely out of its joint. A subluxation means it’s only partially out.
What are the causes of dislocations?
Dislocations can come from accidents, falls, and sports injuries. They can also happen due to loose joints or certain health conditions.
How are dislocations diagnosed?
Doctors use physical exams and imaging like X-rays and MRIs to find dislocations. They also look at other possible causes.
What is the treatment for a dislocated shoulder?
Treatment for a dislocated shoulder includes putting the bone back in place and using casts. It also includes managing pain and helping the shoulder get strong again.
How are hip dislocations treated?
Hip dislocations need quick treatment. This might include putting the bone back in place or surgery. Afterward, doctors help manage any complications.
What are the possible complications of knee dislocations?
Knee dislocations can harm blood vessels and nerves. They can also cause long-term problems with the joint if not treated right.
How can dislocations be prevented?
To prevent dislocations, wear protective gear and do exercises to strengthen joints. Changing how you do activities can also help avoid injuries.
What are the special considerations for managing dislocations in pediatric patients?
Kids need special care because their bones are growing. Doctors must be careful to avoid harming their developing bones and joints.
How do connective tissue disorders affect dislocation management?
People with connective tissue disorders might get dislocations more easily. They need special treatment plans to manage their condition.
What is the recovery timeline for dislocations?
Recovery time for dislocations varies. It starts with immediate care, then moves to recovery and rehabilitation. It depends on the dislocation’s severity and location.
Can dislocations lead to long-term joint degeneration?
Yes, dislocations can lead to joint damage over time. This is more likely if the dislocation is not managed well or happens again.
Reference
- MedlinePlus. (2024, June 17). Dislocation. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000014.htm