
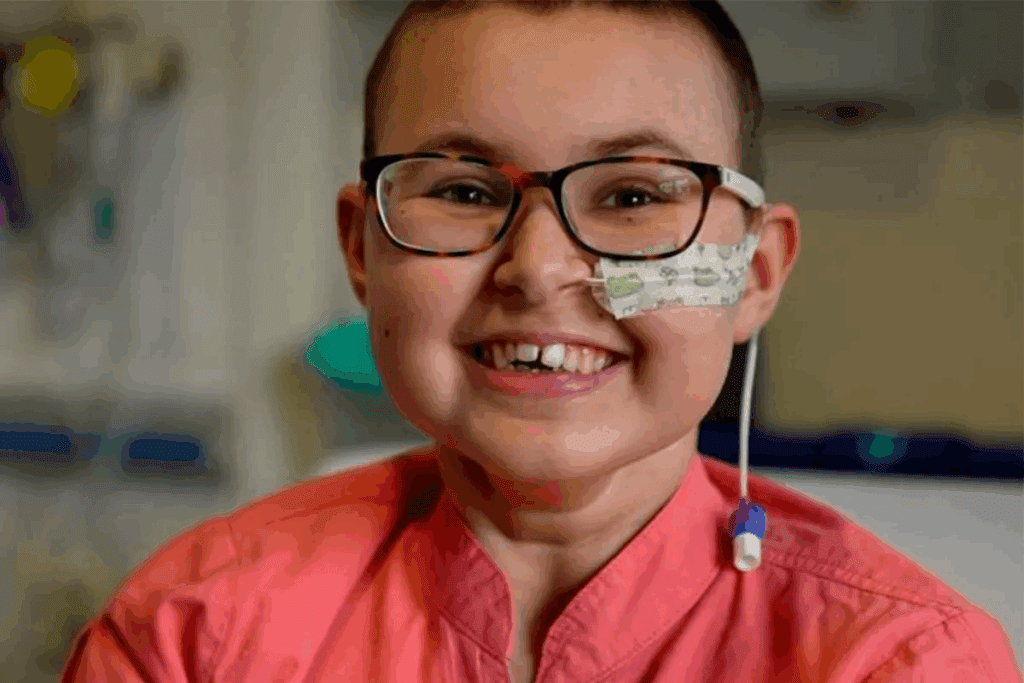
Kids beating cancer statistics
Nearly 80% of children with cancer are now beating the odds and surviving long-term. This is a big improvement from before, thanks to better medical treatments and care. More kids than ever are overcoming the disease.
Looking back, it’s clear that knowing about cancer survival in children is key for families and doctors. The childhood cancer prognosis has gotten much better. This brings hope to those affected.
Key Takeaways
- The overall 5-year survival rate for childhood cancer is approximately 80%.
- Advances in medical treatments have significantly improved childhood cancer survival rates.
- Understanding cancer survival statistics in children is vital for families and healthcare providers.
- The childhood cancer prognosis has improved, bringing new hope.
- Continued research and support are essential for bettering kids beating cancer statistics.
Understanding Pediatric Cancer Survival Rates
Knowing the survival rates for pediatric cancer is key for patients, families, and doctors. These rates show how well treatments work and what the future looks like for kids with cancer.
Survival rates are a way to see how many kids beat a certain cancer type over five years after being diagnosed.
Definition of Survival Rates
Survival rates in pediatric oncology show the percentage of kids who live for a certain time after being diagnosed. The most common rate is the 5-year survival rate. It shows how many kids are alive five years after their cancer diagnosis.
These rates come from big groups of kids with specific cancers. For example, in the U.S., between 2013 and 2019, the 5-year survival rates for kids with cancer changed with age:
| Age Group | 5-Year Survival Rate |
| Less than 1 year | 83.2% |
| 1-4 years | 87.8% |
| 5-9 years | 85.7% |
| 10-14 years | 85.5% |
| 15-19 years | 87.3% |
Importance of Survival Statistics
Survival stats are very important. They show how well treatments work and where we need to do better. They also help families and patients make good choices about their care.
These stats are also key for research. By looking at survival rates over time, researchers can find the best treatments and where to focus more research.
Understanding pediatric cancer survival rates is complex. It involves looking at many statistics and trends. By studying these rates, we can see how well treatments work and what challenges we face in fighting childhood cancer.
Types of Pediatric Cancers

Childhood cancer is not just one disease. It’s a group of different cancers, each with its own traits. We know that pediatric cancers are varied and complex. They need a detailed approach for diagnosis and treatment.
Common Types and Their Statistics
Between 2016 and 2020, the most common cancers in kids and teens were leukemias and brain tumors. Lymphomas, soft tissue tumors, and bone tumors were also common. Leukemia was the most common, making up a big part of pediatric cancer cases.
Recent stats show leukemia makes up about 30% of childhood cancers. Brain and CNS tumors account for 26%. Lymphomas and other cancers make up the rest. Knowing these numbers helps us tailor treatments for the most common cancers.
Rare Cancers and Unique Challenges
Rare pediatric cancers are less common but bring their own challenges. They need special care and new treatment ideas. We face the complexity of rare cancers and the need for more research to help.
Cancers like neuroblastoma and Wilms tumor are rare but important. They need exact diagnosis and treatment plans. This often involves a team of specialists.
We know that pediatric cancers come in many forms. This means we need a flexible and quick treatment plan. By focusing on both common and rare cancers, we aim to improve survival rates and quality of life for all kids with cancer.
Historical Trends in Survival Rates
Pediatric cancer survival rates have greatly improved over time. This is thanks to ongoing medical research and new treatments. We’ve seen a big change in how we treat childhood cancer, leading to better survival rates.
Changes Over the Decades
The five-year survival rate for kids with cancer has dramatically increased. For example, treatments for Acute Lymphoblastic Leukemia (ALL) improved a lot. This raised the five-year survival rate for ALL from 57% in 1975 to 92.3% in 2014–2020.
This big step forward shows how far pediatric oncology has come. It’s a result of hard work and dedication in the field.
Impact of Research and Treatment Advances
The rise in pediatric cancer survival rates is thanks to research and new treatments. New therapies, better chemotherapy, and improved radiation have all helped. These advancements have greatly improved survival chances.
Key factors contributing to the improvement include:
- Advances in genetic understanding and molecular diagnostics
- Development of more effective and less toxic treatments
- Increased participation in clinical trials
- Better supportive care for patients
Together, these factors have led to better survival rates and quality of life for kids with cancer.
Current Survival Rates for Pediatric Cancer
Pediatric Cancer Survival Rates
The current state of pediatric cancer survival rates is both hopeful and challenging. We see promising numbers but also areas that need more work. This shows that while we’ve made big strides in treating childhood cancers, there’s more to discover and achieve.
Overview of Overall Survival Rates
Survival rates for pediatric cancer have been rising over the years. The latest figures show that over 85% of children with cancer now survive for five years. This progress is thanks to better treatments and teamwork from healthcare experts around the world.
Notably, survival rates differ based on the cancer type and the child’s age. For example, lymphoid leukemias, like acute lymphoblastic leukemia (ALL), have a 96% 5-year survival rate for kids aged 1–4. This rate drops to 86% for those aged 10–14, from 2013 to 2019.
Breakdown by Cancer Type
Looking at survival rates by cancer type, we see big differences. Leukemias, the most common pediatric cancer, have seen big jumps in survival rates. ALL, in particular, is very treatable.
On the other hand, brain and central nervous system tumors have lower survival rates. But, survival chances vary based on the tumor type and location. This highlights the need for more research into effective treatments for each cancer type.
Factors Influencing Survival Rates
Understanding what affects pediatric cancer survival rates is key to better outcomes. Several elements play a big role in how well children with cancer do.
Age at Diagnosis
The age a child is when they get diagnosed matters a lot. For example, teens and young adults with Acute Lymphoblastic Leukemia (ALL) might do better with pediatric treatments. This is because cancer in kids and adults is different.
Age-specific treatment approaches are becoming more important. This shows we need treatments that fit the unique needs of kids with cancer.
Access to Treatment and Resources
Getting to the right treatments and resources is also key. Not having access to good care can hurt survival chances. Kids in areas with less access often face big challenges.
Working together and improving access to care can help. Making sure all kids get the best treatments is vital for better survival rates.
By tackling these issues and making care more accessible, we can keep improving survival rates for kids with cancer.
Role of Treatment Modalities
Understanding the role of different treatment modalities is key to knowing how pediatric cancer is treated. The treatment of pediatric cancer is complex. It involves a team of healthcare professionals working together.
Surgery
Surgery is often the first treatment for many pediatric cancers, like solid tumors. The goal of surgery is to remove the tumor completely. This can cure the cancer if it’s only in one place.
We look at several things before deciding on surgery. These include the cancer type and stage, and the child’s health.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It’s a common treatment in pediatric cancer. This is because it can reach cancer cells that have spread.
Chemotherapy regimens are tailored to the specific type of cancer. They often use a mix of drugs to work best.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells or slow their growth. We use it carefully in children because of possible long-term side effects.
The decision to use radiation therapy depends on the cancer type, its location, and the child’s age and health.
| Treatment Modality | Primary Use | Considerations |
| Surgery | Removing solid tumors | Type and stage of cancer, child’s health |
| Chemotherapy | Treating systemic disease | Type of cancer, combination regimens |
| Radiation Therapy | Killing cancer cells with radiation | Potential long-term side effects, age, and health status |
Psychosocial Aspects of Survival
The journey doesn’t end with treatment. Survivors of pediatric cancer face unique challenges. It’s key to address their psychological and social needs as survival rates improve.
Psychological Impact on Survivors
Survivors may deal with anxiety, depression, and PTSD. The trauma of cancer treatment can affect their mental health for a long time.
The impact can vary a lot. Age at diagnosis, cancer type, and treatment can influence it. Early intervention and ongoing support are key to help.
Support Systems and Resources
A strong support system is vital for survivors. This includes family, peer networks, and counseling. Organizations that help childhood cancer survivors are very important.
We need a care approach that covers medical, psychological, and social aspects. This way, we can improve their quality of life.
| Support System | Description | Benefits |
| Family Support | Emotional and practical support from family members | Enhanced emotional well-being, improved coping mechanisms |
| Peer Networks | Connecting with other survivors and families | Reduced feelings of isolation, shared experiences and advice |
| Professional Counseling | Trained therapists providing psychological support | Addressing anxiety, depression, and PTSD, improved mental health |
Understanding and supporting the psychosocial aspects of pediatric cancer survival can greatly improve lives. This includes survivors and their families.
Long-term Outcomes for Survivors
The journey doesn’t end with treatment completion. For childhood cancer survivors, the focus shifts to long-term health and well-being. As survival rates improve, it’s key to tackle the challenges survivors face post-treatment.
Quality of Life Post-Treatment
Survivors of pediatric cancer often face physical, emotional, and social challenges. These can affect their quality of life. Research shows that two-thirds of childhood cancer survivors face at least one chronic health condition.
Also, one-quarter face a late-effect from treatment that is classified as severe or life-threatening. These challenges can make education, employment, and personal relationships tough. This highlights the need for strong support systems.
Late Effects of Treatment
The late effects of pediatric cancer treatment can be far-reaching. They can affect various aspects of a survivor’s health. These effects can include organ damage, secondary cancers, and psychological issues like anxiety and depression.
Understanding these effects is key for providing the right follow-up care. Healthcare providers are working on personalized care plans. These plans consider the treatments received and the individual needs of each survivor.
This approach helps in early detection and management of late effects. It improves the overall quality of life for survivors.
Ongoing Research and Future Projections
The field of pediatric oncology is changing fast. New research is leading to better treatments. We’re seeing big changes in how we treat childhood cancers thanks to new tech and a better understanding of cancer.
New Treatments on the Horizon
New treatments for childhood cancer are coming quickly. Some exciting areas include:
- Immunotherapy: Using the immune system to fight cancer.
- Targeted Therapy: Drugs that target specific cancer-causing genes.
- Precision Medicine: Treatments based on a patient’s unique genetic profile.
These new methods are showing great promise in trials. They offer hope to families dealing with pediatric cancer.
Clinical Trials and Innovations
Clinical trials are key for moving forward in pediatric oncology. They help us learn about new treatments’ safety and effectiveness. We’re seeing more teamwork between research places, hospitals, and drug companies to speed up new therapy development.
“The future of pediatric cancer treatment is not just about treating the disease, but about improving the quality of life for survivors.”
Some big changes in trials include:
- Adaptive trial designs that can change based on new data.
- Using biomarkers to find the right treatment for each patient.
- Focusing more on how treatments affect patients’ lives and long-term survival.
But, only 4% of the federal cancer research budget goes to pediatric cancers. We need to push for more funding to keep research going and improve survival rates.
Looking ahead, combining new treatments and trial innovations will be key in pediatric oncology’s future. We’re dedicated to supporting research that helps kids with cancer get better outcomes.
How Families Can Navigate Pediatric Cancer
Families dealing with pediatric cancer often feel lost and unsure. They need reliable resources and a clear understanding of the condition to navigate it.
Support and Resources
Groups like the Children’s Oncology Group (COG) offer important help. They provide info on treatments, support networks, and how to deal with the emotional side of a diagnosis.
Advocacy and Awareness
It’s key to raise awareness about pediatric cancer. This helps improve survival rates for kids with cancer. Families can join efforts through organizations focused on pediatric cancer.
With the right support and resources, families can face pediatric cancer’s challenges. Our aim is to ensure every child gets top-notch care. We also want to support their families every step of the way.
FAQ
What are the current survival rates for pediatric cancer?
Survival rates for kids with cancer have greatly improved. In many countries, over 85% of children survive. But, rates vary by cancer type, age, and other factors.
How are pediatric cancer survival rates calculated?
Survival rates are based on kids who live five years after being diagnosed. They come from big datasets and stats.
What are the most common types of pediatric cancers?
Common cancers in kids include leukemia, brain tumors, lymphoma, and neuroblastoma. Each has its own treatment.
How do treatment modalities impact pediatric cancer survival rates?
Treatments like surgery, chemo, and radiation are key to survival. The right treatment depends on the cancer and the child’s health.
What are the long-term effects of pediatric cancer treatment?
Kids who survive cancer may face long-term challenges. These include physical, emotional, and brain issues. Ongoing care is vital for their well-being.
What resources are available to families navigating pediatric cancer?
Families can find many resources. This includes counseling, support groups, and advocacy groups. These help with the emotional and practical sides of cancer.
How can families advocate for pediatric cancer awareness and research?
Families can help by fundraising, sharing their stories, and supporting research. This raises awareness and helps improve treatments.
What is the significance of clinical trials in pediatric oncology?
Clinical trials are vital in finding new and better treatments. They help improve survival rates and quality of life for kids with cancer.
How do age and access to treatment impact pediatric cancer survival rates?
Age and access to care are big factors. Younger kids and those with less access to care often face tougher challenges.
What are the current trends in pediatric cancer research?
Research is focused on targeted therapies, better immunotherapy, and more precise treatments. These advances aim to improve survival and reduce side effects.
References
- National Cancer Institute. (2024). Cancer in children and adolescents. (NIH Publication No. 24-5213). https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
- World Health Organization. (2025). Childhood cancer. https://www.who.int/news-room/fact-sheets/detail/cancer-in-children




































