Last Updated on November 20, 2025 by Ugurkan Demir
Sickle cell disease (SCD) is inherited and can affect people of any race or ethnicity, including Caucasians; while it is most prevalent among individuals with ancestry from sub‑Saharan Africa, it is also found in Hispanic populations from Central and South America, as well as people from the Middle East, India, Mediterranean regions, and parts of Asia. The misconception that only Black people develop SCD can delay diagnosis in others; newborn screening, family history review, and hemoglobin electrophoresis help confirm SCD or sickle cell trait in anyone, including a white person sickle cell scenario. Because SCD affects red blood cell shape and flow, timely preventive care (vaccinations, penicillin prophylaxis in children), pain crisis plans, hydroxyurea or newer disease‑modifying therapies, and evaluation for curative options like stem cell transplantation or gene therapy are important for all patients, regardless of background.
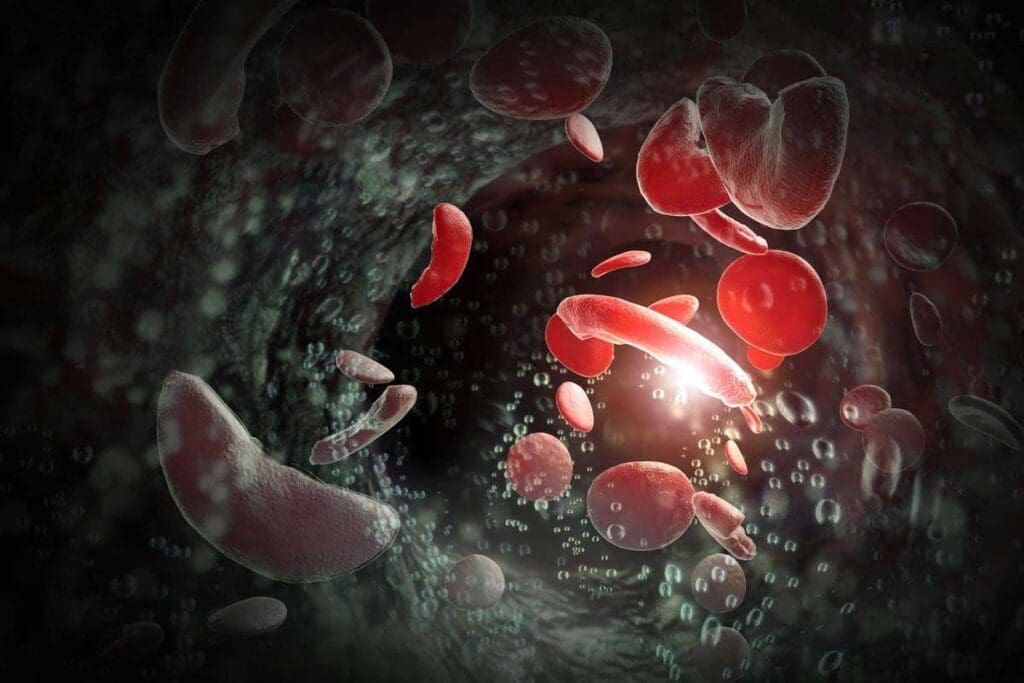
Learning about sickle cell anemia is key to understanding its effects. It’s a genetic disorder that changes the hemoglobin in red blood cells. This change makes the cells sickle-shaped, which hinders oxygen transport and can cause health problems.
Sickle cell anemia happens when someone gets two sickle cell genes, one from each parent. This condition leads to abnormal hemoglobin, called hemoglobin S. This abnormal hemoglobin makes red blood cells rigid and sickle-shaped under certain conditions.
The sickling of red blood cells can cause many health problems. These include anemia, pain crises, and a higher risk of infections. When sickled red blood cells break down, it leads to anemia. Also, these abnormal cells can block blood vessels, causing pain and potentially harming organs over time.
The genetic cause of sickle cell anemia is a mutation in the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. The mutation leads to hemoglobin S production. Having two copies of this mutated gene, one from each parent, results in sickle cell anemia. It’s not limited to any ethnic group, though its prevalence varies.
It’s important to know that sickle cell anemia can affect anyone, not just certain ethnic groups. Believing it only affects certain populations can cause late diagnosis and treatment in groups like Caucasians.

Sickle cell anemia is found in different parts of the world. It affects many ethnic groups and is a big health problem. In the United States, it impacts over 100,000 people. Globally, it affects about 20 million.
Sickle cell disease is common among people of African descent. But it also affects those from Mediterranean, Middle Eastern, and Indian backgrounds. The disease is linked to malaria, as the sickle cell trait protects against it.
In places where malaria is common, more people carry the sickle cell trait. This includes parts of Africa, the Mediterranean, and some areas in the Middle East and India. But,thanks to migration and intermarriage, SCD is found worldwide, including Europe and the Americas.
People of African descent are at higher risk for SCD. In the United States, about 1 in 500 African Americans has SCD. Also, 1 in 12 African Americans carries the sickle cell trait. SCD is less common but can occur in Caucasians, mainly those of Mediterranean ancestry.
Can a white person get sickle cell anemia? Yes, but it’s less common. Many think SCD only affects African Americans, leading to late diagnosis in others. Healthcare providers should screen patients of all backgrounds, even if there’s no African American ancestry.
Knowing where SCD is common helps find at-risk groups. This info is key for better screening, care, and awareness about the disease.
Sickle cell anemia is not just found in certain ethnic groups. Caucasians can also be affected. It’s not about race, but about genetics.
Many think sickle cell anemia only hits people of African, Caribbean, or Middle Eastern descent. But it can happen to anyone with the right genes.
Genetic inheritance is key. If both parents carry the sickle cell trait, there’s a 25% chance their child will have it, race aside.
The sickle cell trait changes a lot between groups. In the U.S., 1 in 12 African Americans has it. Caucasians have much lower rates.
| Population Group | Estimated Prevalence of Sickle Cell Trait |
| African Americans | 1 in 12 |
| Hispanic Americans | 1 in 100 |
| Caucasian Americans | 1 in 2,500 to 1 in 4,000 |
Healthcare providers should always consider sickle cell anemia, no matter the patient’s race.
Knowing about genetic factors and prevalence helps in giving the right care to everyone, no matter their ethnicity.
Looking into sickle cell anemia in white people means checking hospital rates and the sickle cell trait. This genetic disorder messes with hemoglobin, making red blood cells break down. It’s not just a problem in certain groups; it can hit anyone.
Research shows sickle cell disease hits all races, including white Americans. About 1.8 percent of those hospitalized for it in the U.S. are white. This shows it’s a big health issue, even if it’s less common.
Let’s dive deeper into hospital rates:
| Ethnic Group | Hospitalization Rate for Sickle Cell Disease |
| White Americans | 1.8% |
| African Americans | 80-90% |
| Hispanic Americans | 5-10% |
The sickle cell trait means having one sickle cell gene and one normal one. It’s not the same as sickle cell anemia, which has two sickle cell genes. Knowing how common the trait is in white newborns helps us understand sickle cell disease.
About 3 per 1,000 white newborns have the sickle cell trait. This info is key for public health planning and understanding the disease’s genetics.
“The presence of sickle cell trait in white newborns highlights the need for universal screening for sickle cell disease.” – Hematologist
These numbers show we need to spread awareness and screen everyone, no matter their race or ethnicity. Knowing how sickle cell disease affects people helps doctors and families deal with it better.
Many think sickle cell anemia only affects people of African descent. But it has been found in people of many ethnic backgrounds, including Caucasians. This disease is a genetic disorder that can happen to anyone, nregardless ofrace or ethnicity. Its occurrence varies a lot among different groups.
Sickle cell anemia is rare in Caucasians because the sickle cell gene is less common in them. The gene is more common in places where malaria was once common. This is because the gene helps protect against malaria.
Genetic factors are key to who gets sickle cell disease. Caucasians are less likely to have the sickle cell gene. But it can happen. People with ancestry from places where malaria was common, like Southern Europe or the Middle East, might have it.
To grasp how rare sickle cell anemia is in Caucasians, we need to look at its prevalence in different groups. Here’s a table showing the sickle cell trait in various ethnic groups:
| Ethnic Group | Prevalence of Sickle Cell Trait |
| African American | 8-10% |
| Hispanic American | 2-3% |
| Caucasian American | 0.1-0.3% |
| South Asian | 2-4% |
| Mediterranean | 1-2% |
The table shows that while Caucasians have a lower rate of sickle cell trait, it’s not unheard of. Knowing these rates is important for diagnosing and treating the disease in different groups.
Genetic diseases like sickle cell anemia don’t respect ethnic boundaries. Even though it’s less common in Caucasians, awareness and proper diagnosis are vital for managing it in all populations.
Sickle cell anemia is not just linked to African heritage. It also shows up in people with Mediterranean and Southern European ancestry. This is due to historical genetic adaptations to malaria in these areas.
The Mediterranean has long battled malaria. This disease pushed for genetic traits that protect against it, like the sickle cell trait. So, sickle cell anemia is more common in these areas.
Malaria’s impact on Mediterranean countries’ genetics is clear. It forced the sickle cell trait to become more common as a defense against malaria.
The way sickle cell anemia is passed down in European populations is complex. It’s shaped by history and migration. These factors mix up the sickle cell gene in these groups.
Looking into the link between sickle cell anemia and Mediterranean or Southern European ancestry helps us understand its history and genetics. This knowledge is vital for managing the condition in these populations.
It’s important to know how sickle cell disease shows up differently in different racial groups. The main symptoms are the same, but how bad they are and the complications can vary.
Symptoms of sickle cell disease can change a lot between racial groups. People of African descent often have more severe anemia and face higher risks of certain problems. On the other hand, those from Mediterranean or Middle Eastern backgrounds might have different symptoms, like different levels of hemolysis.
Key differences in symptoms include:
It’s key to think about a patient’s ethnic background when diagnosing and treating sickle cell disease.
The severity of sickle cell disease and its complications also varies among different racial groups. For example, people of African descent often face more severe disease, with higher rates of acute chest syndrome and other serious problems.
| Racial Group | Common Complications | Severity Level |
| African Descent | Acute chest syndrome, severe anemia | High |
| Mediterranean Descent | Mild anemia, gallstones | Moderate |
| Caucasian | Vaso-occlusive crises, infections | Variable |
Knowing these differences helps healthcare providers make treatment plans that fit the needs of patients from different racial backgrounds.
Diagnosing sickle cell anemia in white people is tricky because it’s rare. This makes doctors less likely to think of it. As a result, white patients might get diagnosed later, which can hurt their treatment.
Many think sickle cell anemia only affects people of African descent. But this thinking can cause doctors to miss it in white patients. Doctors need to always think of sickle cell anemia, no matter the patient’s race.
Screening for sickle cell disease is not done everywhere. Even in places where it is, some white babies might not get tested. This can lead to late diagnosis and serious problems.
To diagnose sickle cell anemia, doctors use several methods. They check blood counts and use special tests like High-Performance Liquid Chromatography (HPLC). Genetic tests are also needed to confirm the diagnosis.
For white patients, a detailed check-up is key. This includes a full medical history, physical exam, and lab tests. Early diagnosis is key to avoiding serious issues and improving life quality.
Doctors should always consider sickle cell anemia, even in less common cases. This way, they can catch it early and treat it right, no matter the patient’s background.
Treating sickle cell anemia requires a mix of strategies to manage symptoms and prevent problems. This approach improves patients’ lives and lowers the risk of serious issues.
For sickle cell anemia, doctors use several treatments. Hydroxyurea is a key drug that helps lessen painful episodes and might cut down on blood transfusions. Blood transfusions are also vital, as they lower the risk of serious problems by reducing sickled red blood cells.
| Treatment | Purpose | Benefits |
| Hydroxyurea | Reduce frequency of painful crises | Decreases painful episodes, reduces the need for blood transfusions |
| Blood Transfusions | Reduce risk of complications | Decreases the number of red blood cells that can sickle, reducingthe risk of stroke. |
| Pain Management | Manage acute and chronic pain | Improves quality of life, reduces hospitalizations |
A study in a top medical journal showed hydroxyurea’s big impact. It has cut down on painful episodes and hospital stays for patients.
“Hydroxyurea has become a cornerstone in the treatment of sickle cell disease, improving patient outcomes and quality of life.”
Personalized medicine is key in treating sickle cell anemia. Genetic testing and other tools help make treatment plans fit each patient’s needs. For example, those at high stroke risk might need more aggressive treatment, like regular blood transfusions.
Every patient reacts differently to treatment. So, it’s important to keep an eye on how they’re doing and adjust their care as needed. This tailored approach makes sure patients get the best care for their unique situation.
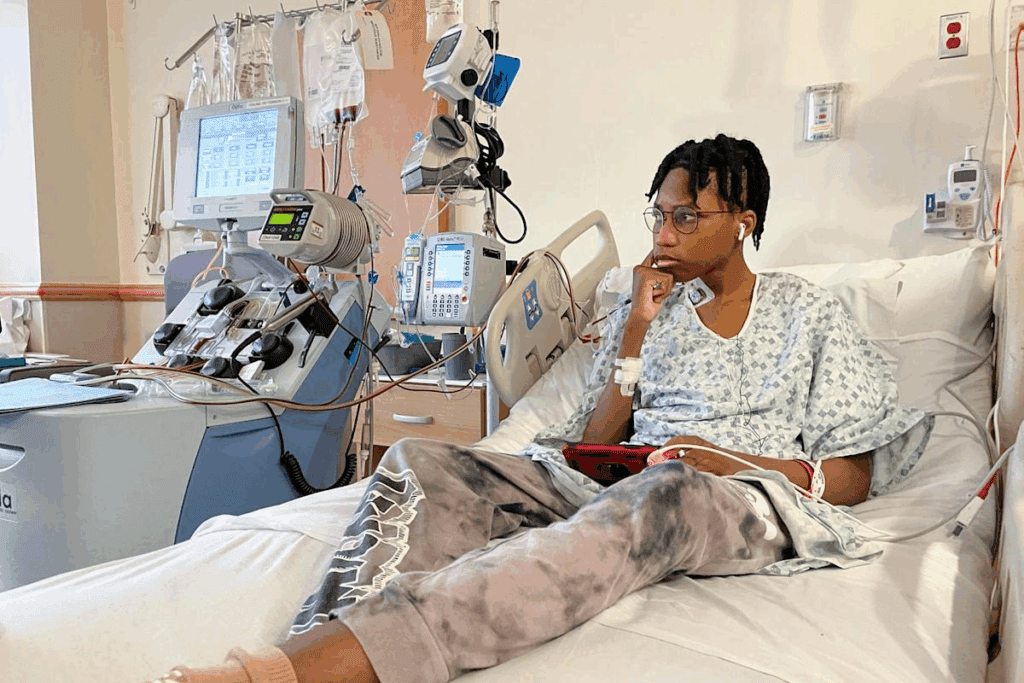
Living with sickle cell anemia is tough, no matter your background. It’s more common in some groups, but Caucasians face unique challenges. They often get a late diagnosis and struggle with treatment.
Caucasian patients face a complex journey with sickle cell anemia. It’s rare in their group, which can cause delays in finding out they have it. This misunderstanding can make things harder.
Studies show how Caucasian patients deal with sickle cell anemia. For example, a study in a medical journal told about a Caucasian man who was diagnosed later in life. It shows how important it is to think about the disease in everyone, not just certain groups.
These stories show how different people’s experiences can be. Getting diagnosed early, managing symptoms well, and having good support are key to doing well.
Having support and resources is essential for those with sickle cell anemia. These can include doctors who know about the disease, support groups, and educational materials.
For Caucasians, finding others who understand can be really helpful. Support groups, online or in person, are great for sharing experiences and advice.
Also, places like the Sickle Cell Disease Association of America offer a lot of help. They provide information on managing the disease, finding care, and navigating the healthcare system.
Key resources include:
By using these resources and support, people with sickle cell anemia, including Caucasians, can manage their condition better. This can improve their quality.
We’ve looked into sickle cell anemia, a condition that affects many, including white people and Caucasians. It’s important to understand its genetic roots for diagnosis and treatment.
While sickle cell anemia is rare in white people, it does happen. It shows us that everyone needs the same care, no matter their background.
Healthcare providers can give better care by knowing that sickle cell disease affects everyone. It’s key to recognize it in all groups for proper treatment.
As we learn more about medicine, we must see the big picture. Sickle cell anemia needs a careful approach that considers everyone’s background.
Yes, Caucasians can get sickle cell anemia. It’s just not as common in this group as in others.
No, sickle cell anemia isn’t limited to any ethnic group. It can happen to anyone, though it’s more common in some groups.
Sickle cell anemia comes from a gene mutation in the HBB gene. This mutation makes abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
It makes red blood cells misshapen, and they break down. This leads to anemia, pain crises, and other issues.
Yes, white people can get sickle cell anemia if they inherit the mutated HBB gene from their parents.
Sickle cell anemia is rare in white populations. But it can happen.
Yes, a white person can have sickle cell trait if they have one copy of the mutated HBB gene.
Sickle cell disease can show up differently in different racial groups. Symptoms, severity, and complications can vary.
Caucasian patients are diagnosed with sickle cell anemia the same way as others. Blood tests and genetic analysis are used.
Yes, diagnosing sickle cell anemia in white people can be tricky. It’s rare in this group, which can lead to missed or delayed diagnoses.
Treatment for sickle cell patients includes pain management, hydration, and blood transfusions. Personalized medicine is also considered.
Yes, white people with sickle cell anemia can get the same support as others. This includes medical care, counseling, and support groups.
The sickle cell trait is rare in white newborns compared to other ethnic groups.
Yes, history and genetics play a role in sickle cell anemia in Mediterranean or Southern European populations. This includes genetic patterns and exposure to malaria.
Ashorobi, D., Lubega, C., & Osuji, J. (2024). Sickle Cell Trait. StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK537130/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!