Last Updated on November 20, 2025 by Ugurkan Demir

Sickle Cell Disease (SCD) is not just found in African or African American people. About 1.8 percent of hospitalized SCD patients in the United States are White. This shows we need to know more about it in different groups.Discover key facts about can a white person have sickle cell disease, including symptoms and rarity.
New studies have given us key information about SCD in Caucasians. They tell us about its genetic causes and how it shows up in people. This article will share five important facts about SCD in White people. It’s based on top medical research and Liv Hospital’s focus on caring for patients.
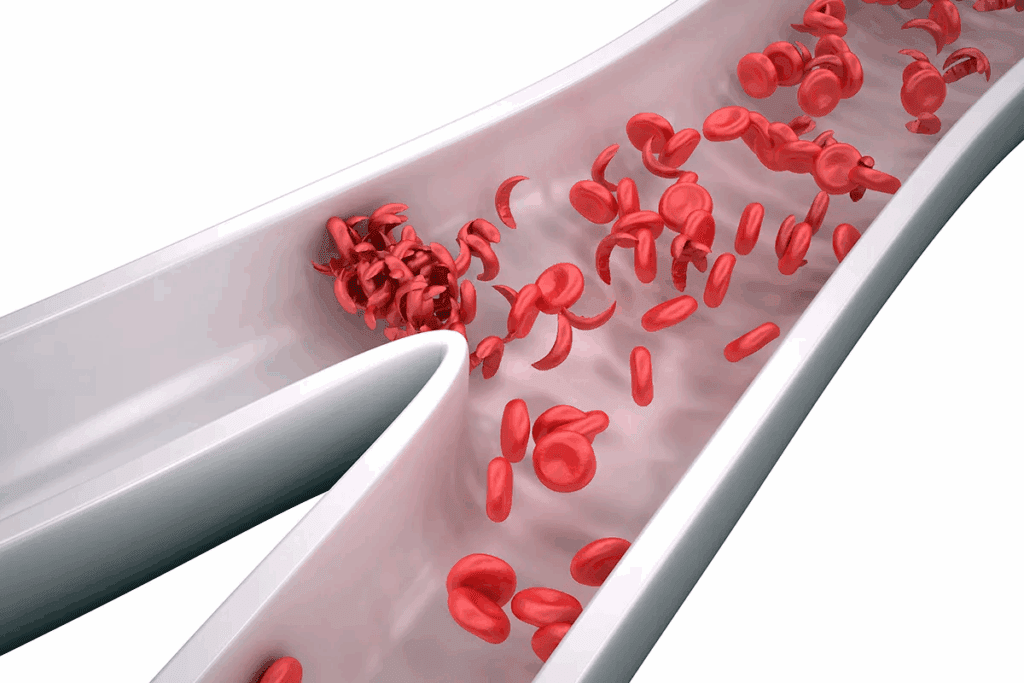
To understand Sickle Cell Disease, we need to know what it is. SCD is a group of inherited disorders that affect hemoglobin production. This makes red blood cells sickle-shaped and stiff.
Sickle Cell Disease is caused by abnormal hemoglobin, called sickle hemoglobin or hemoglobin S. This abnormality distorts red blood cells. They can get stuck in small blood vessels, reducing or blocking blood flow.
The condition is caused by a mutation in the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. It’s inherited in an autosomal recessive pattern. This means a person needs two defective copies of the gene to develop the condition.
Carriers have one copy of the mutated gene. They may not show symptoms but can pass the condition to their children.
The sickling of red blood cells can cause many health issues. These cells break down early, leading to anemia. They can also cause pain episodes, infections, and damage to organs like the spleen, kidneys, and liver.
Common complications of SCD include:
Many think Sickle Cell Disease only affects people of African descent. While it’s true it’s more common in certain regions, it can affect anyone. This includes Caucasians.
It’s important to know SCD is not limited to any ethnic group. The belief that “sickle cell disease is rare in white people” can lead to delayed diagnosis. In reality, while less common, SCD can occur in white populations, too.
Can white people have Sickle Cell Disease? The answer is yes. SCD is not just for certain races or ethnic groups. It can happen to anyone, regardless of their background.
Many think SCD only affects African Americans. But that’s not true. Research shows it can happen to people from many ethnic backgrounds, including Caucasians.
Studies have found SCD in white people, though it’s less common. For example, a U.S. study found about 1.8 percent of hospitalized SCD patients were White. This shows SCD isn’t limited to one race.
While SCD is less common in white Americans, it’s not unheard of. White individuals make up a small part of SCD cases in the U.S. But it’s important to recognize and treat it in this group too.
In summary, SCD can affect anyone, no matter their race or ethnicity. Healthcare providers need to keep this in mind when treating patients.
Understanding sickle cell disease’s genetic basis is key. It shows how people from different ethnic groups, including Whites, can get the condition. Sickle cell disease comes from a mutation in the HBB gene. This mutation makes abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
Sickle cell disease is an autosomal recessive disorder. This means a person needs two defective HBB genes, one from each parent, to have the disease. Those with one mutated gene have the sickle cell trait. The disease’s genetics involve many factors that affect its severity and how it presents.
The sickle cell trait is different from sickle cell disease. Yet, people with the trait can pass the mutated gene to their kids. When two carriers have children, there’s a 25% chance each pregnancy that the child will have sickle cell disease.
In Caucasian families, sickle cell disease follows the same autosomal recessive pattern as in other groups. But, because the sickle cell trait is less common in Whites, the disease is rarer in these communities. It’s important for families with sickle cell history to get genetic counseling to understand their risks.
Genetic counseling helps families understand their chances of passing on the sickle cell gene. This is vital for families of Mediterranean or Middle Eastern descent, where the trait is more common.
Sickle cell disease in Whites often comes from areas where it’s more common, like Southern Europe, the Mediterranean, and the Middle East. Migration and intermarriage have spread the sickle cell gene across different groups.
In the U.S., sickle cell disease in Whites might be more common in families from Greece, Italy, or the Middle East. This is because the trait offers protection against malaria.
Sickle Cell Disease is more common in Mediterranean populations. This is not just a coincidence. It’s tied to the region’s history and genetics.
In Southern Europe, the Sickle Cell Trait is found in many places. Countries like Greece, Italy, and Spain have seen cases of Sickle Cell Disease. Malaria’s past presence in these areas helped spread the Sickle Cell Trait.
“The sickle cell trait offered protection against malaria, which was common in Southern Europe,” researchers found.
The malaria protection theory says the Sickle Cell Trait helps people in malaria areas. This idea is backed by the Sickle Cell Trait’s commonness in malaria-hit places.
Today, people moving around has made populations more diverse. This includes the spread of the Sickle Cell Trait. When people move, they take their genes with them, possibly introducing the Sickle Cell Trait to new places.
Genetic diversity helps us understand Sickle Cell Disease’s spread. The mix of genes and environment has shaped where the disease is found.
| Region | Historical Malaria Prevalence | Sickle Cell Trait Frequency |
| Greece | High | Moderate |
| Italy | High | Moderate |
| Spain | Moderate | Low to Moderate |
It’s key to know how SCD shows up in white patients for the right diagnosis and care. Sickle Cell Disease is a genetic disorder that affects hemoglobin. It’s often linked to African descent but can also affect whites.
Symptoms of SCD differ among ethnic groups. In whites, the disease might show up with atypical symptoms. This makes it harder to diagnose. For example, whites might get acute chest syndrome more often or have different anemia levels than Africans.
Studies show that a patient’s genetic background affects SCD’s severity and how it shows up. Whites with SCD might face more complications because of other genes.
Diagnosing SCD in whites is tough because it’s rare in this group. Doctors might not think of SCD first, causing delays in treatment. Early diagnosis is critical to avoid serious problems and improve health outcomes.
Diagnosing is harder because whites don’t usually have the typical SCD risk factors. So, doctors need to be extra careful and aware of SCD in all groups.
Case studies show how SCD can be different in whites. For instance, a study found a white patient with SCD who had priapism often. Priapism is rare in SCD in whites.
These cases remind us to think of SCD in whites with symptoms, even if they don’t fit the usual risk profile. Looking at these cases helps doctors understand SCD’s many faces.
The reality of SCD in white populations is more complex than we thought. SCD is not just a disease of African ancestry. Data from various sources show it affects other groups too.
In the US, about 1.8% of SCD patients in hospitals are white. This fact challenges the idea that SCD mainly affects people of African descent.
European studies have found SCD in white populations. In Southern Europe, the history of malaria has led to more cases of the sickle cell trait.
| Country | Prevalence Rate |
| Greece | 1 in 500 |
| Italy | 1 in 1,000 |
| Spain | 1 in 2,000 |
Incidence rates of SCD vary among white populations. For example, people of Mediterranean descent have a higher rate. This is because malaria was more common in these areas.
Key Findings:
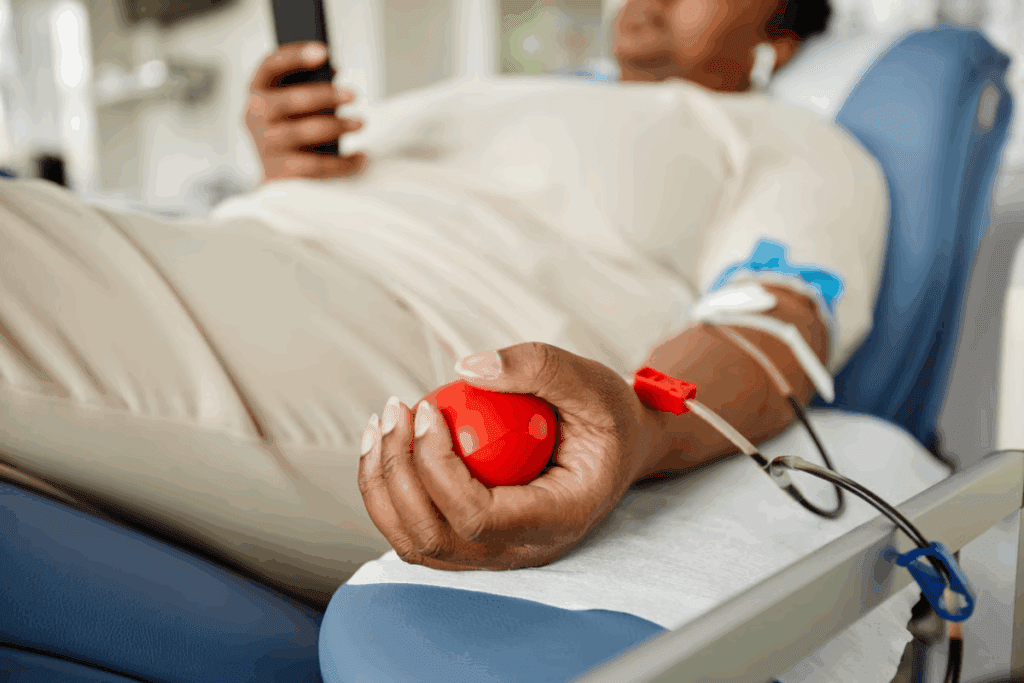
White families worried about sickle cell disease can get valuable insights from genetic testing and counseling. Sickle cell disease is not just for people of African descent. It can affect anyone. So, knowing your genetic risks is key.
White people should think about sickle cell screening if they have a family history of it. Or if they are from Mediterranean, Middle Eastern, or Indian backgrounds. Genetic testing can find sickle cell gene carriers. This is important for planning families and understanding health risks.
Being a carrier means having one normal and one sickle cell gene. Carriers are usually healthy but can pass the sickle cell gene to their kids. Knowing your carrier status is key for planning families. If both parents are carriers, there’s a 25% chance their child will have sickle cell disease.
| Carrier Status of Parents | Risk of SCD in Offspring |
| Both parents are carriers | 25% |
| One parent is a carrier | 0% (but 50% chance of being a carrier) |
There are many genetic tests to find sickle cell carriers and diagnose the disease. These include:
Understanding test results needs a professional. A genetic counselor can explain risks and what test results mean.
By knowing their genetic risks and testing options, White families can make smart health and family planning choices.
There are many ways to treat Sickle Cell Disease. These include standard medical care and new therapies. Each approach helps manage different parts of the disease.
Standard treatments for SCD are key to managing symptoms and preventing problems. These include:
A leading hematologist says, “Early treatment with proven therapies can greatly improve SCD patients’ lives.”
“The cornerstone of SCD management is a personalized care plan tailored to the individual patient’s needs.”
Centers like Liv Hospital have advanced treatment plans for SCD patients. These plans often include:
| Protocol | Description | Benefits |
| Comprehensive Care Plans | Personalized treatment plans addressing the unique needs of each patient | Improved patient outcomes, enhanced quality of life |
| Multidisciplinary Teams | Teams of specialists including hematologists, nurses, and other healthcare professionals | Better coordination of care, more effective management of complications |
| Access to Clinical Trials | Opportunities for patients to participate in cutting-edge research studies | Potential access to new, innovative treatments |
The treatment for SCD is changing fast. New therapies and clinical trials are showing promise. These include:
As research keeps moving forward, the future for SCD treatment looks bright. New and better therapies are on the way.
It’s important to hear from people with Sickle Cell Disease, including those who are White. Their stories help us understand the disease better and support them better.
White people with Sickle Cell Disease face special challenges. They are less common in their group. A study shows they might get misdiagnosed or face delays because of their race.
A young White woman was diagnosed with SCD later in life. She felt shocked and confused. She also struggled to find doctors who knew about her condition.
Getting help from doctors can be hard for SCD patients, even more so for those who are White. Doctors might not know as much about SCD in White people. This can lead to wrong diagnoses or not getting the right care.
Patients need to speak up for themselves. They should look for specialized centers that know about SCD. These places offer important help and support.
Patients with SCD, no matter their race, can find many resources. There are support groups, educational materials, and online communities. Groups focused on SCD awareness and research also help a lot.
By using these resources and sharing their stories, we can improve care for all SCD patients. This includes those from different ethnic backgrounds.
Raising awareness about Sickle Cell Disease (SCD) is key to better care. Many think SCD only affects people of African descent. This belief has caused delays in diagnosis and poor care for White patients.
To clear up myths about SCD, we need to understand its genetics and clinical aspects well. Recognizing that SCD can affect anyone helps healthcare providers give better care. This care is more inclusive and effective.
Teaching healthcare workers and the public about SCD’s presence in different ethnic groups is important. This education can lead to quicker diagnoses and better management of SCD. It improves patients’ lives significantly.
We must keep researching and educating to ensure SCD is recognized and treated in all groups. This effort will help create a fair healthcare system. A system that gives the best care to every patient, no matter their background.
Yes, Caucasians can get sickle cell anemia. It’s more common in African and African American populations, though.
No, sickle cell disease isn’t just for people of African descent. It can happen in people of many ethnic backgrounds, including White people. This is true, even for those from Mediterranean regions.
White people can inherit sickle cell trait if they have a family history of it. It can also happen if they come from areas where the sickle cell gene is common, like Southern Europe.
Symptoms in White patients with sickle cell disease can vary. They might include pain episodes, anemia, infections, and other complications. These symptoms are similar to those in patients of other ethnicities.
Some White populations, like those from Mediterranean regions, have higher rates of sickle cell disease. This is due to historical genetic factors and the presence of the sickle cell trait in their ancestry. Malaria’s prevalence in these areas also played a role.
Sickle cell disease is less common in White people than in some other ethnic groups. But, it does occur in them. Different studies and populations report varying prevalence rates.
Yes, a White person can have sickle cell disease. It’s important for healthcare providers to consider this diagnosis in patients of all ethnic backgrounds.
Yes, White people can get sickle cell anemia. It’s important to be aware of this possibility for timely diagnosis and proper management.
Genetic testing is key for White families at risk of SCD. It helps identify carriers of the sickle cell trait. It also assesses the risk of passing the disease to their offspring.
While treatment for SCD is generally the same across ethnic groups, healthcare providers may need to consider specific factors. They should also be aware of any variations in disease presentation in White patients with SCD.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!