
Sickle cell disease is often perceived as affecting only Black or African American communities, yet it is a genetic condition that can appear in any population due to inherited hemoglobin variants; addressing “sickle cell in caucasian” helps correct this myth and promotes timely testing for everyone. While most U.S. cases occur in non‑Hispanic Black individuals, sickle cell is also found among people with Mediterranean, Middle Eastern, South Asian, and Hispanic ancestry—and in Caucasians through diverse family lineages. Universal newborn screening, hemoglobin electrophoresis, and genetic counseling support accurate diagnosis, risk awareness, and informed family planning. At LivHospital, the focus is on equitable, guideline‑based care—vaccinations, infection prevention, hydroxyurea and other disease‑modifying therapies, individualized pain‑crisis plans, and evaluation for curative options such as stem cell transplantation or gene therapy—so every patient receives compassionate, effective treatment regardless of background.
Key Takeaways
- Sickle cell disease is not exclusive to African Americans.
- The condition can occur in individuals of any ethnicity.
- Genetic factors play a critical role in sickle cell disease prevalence.
- Accurate diagnosis and cpropercare are key for all patients.
- LivHospital focuses on patient-centered care and high international standards.
What is Sickle Cell Disease?

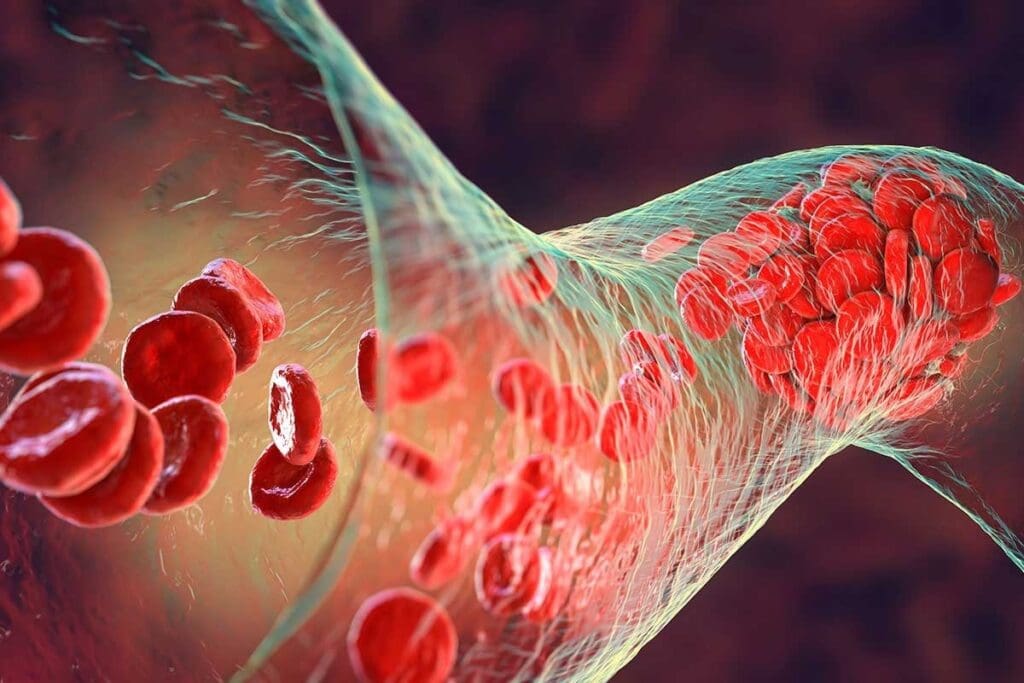
Sickle Cell Disease (SCD) is a genetic disorder that affects hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen. Our bodies need to function properly.
The Genetic Mutation Behind Sickle Cell Disease
SCD is caused by a specific genetic mutation in the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. The mutation leads to the production of abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
The mutation changes glutamic acid to valine at the sixth position of the beta-globin chain. This causes hemoglobin to aggregate under low oxygen conditions. It forms fibers that distort red blood cells into a sickle shape.
- The mutation is inherited in an autosomal recessive pattern. This means an individual must inherit two mutated copies (one from each parent) to express the disease.
- Individuals with one mutated gene and one normal gene are carriers of the sickle cell trait.
How Sickle Cell Trait Differs from Sickle Cell Disease
Sickle Cell Trait (SCT) occurs when an individual inherits one normal HBB gene and one mutated HBB gene. Unlike SCD, SCT typically does not cause significant health problems. It can have implications under certain conditions, such as intense physical exertion or high altitudes.
The key differences between SCD and SCT are:
- Disease Expression: SCD is characterized by recurring episodes of pain, anemia, and increased risk of infections. SCT is generally asymptomatic.
- Genetic Inheritance: SCD requires two mutated genes. SCT is the result of one mutated and one normal gene.
- Health Implications: Individuals with SCT are generally healthy. They can pass the mutated gene to their offspring.
In summary, understanding the genetic basis of Sickle Cell Disease and distinguishing it from Sickle Cell Trait is key. It’s vital for diagnosis, management, and genetic counseling.
The Evolutionary History of Sickle Cell Disease
Sickle cell disease (SCD) has a strong link to malaria in certain areas. It’s more common in places like sub-Saharan Africa and parts of the Mediterranean. This connection is not just a coincidence.
The genetic change that causes SCD helps protect against severe malaria. This protection has made the sickle cell trait more common in areas where malaria is common.
Malaria Resistance and Natural Selection
The sickle cell trait offers a survival edge against malaria. People with this trait are less likely to die from malaria. This means they are more likely to have children and pass on their genes.
“The sickle cell trait has been shown to confer protection against severe malaria, which has led to its increased prevalence in areas where malaria is endemic.”
This natural selection has shaped where SCD is found around the world. It’s more common in places where malaria has been a big problem.
Geographic Distribution and Historical Patterns
The spread of SCD mirrors the history of malaria. In sub-Saharan Africa, where malaria has been a big issue, SCD is most common.
| Region | Prevalence of SCD | Historical Malaria Prevalence |
| Sub-Saharan Africa | High | Very High |
| Mediterranean | Moderate | High |
| South Asia | Moderate | High |
The table shows how SCD and malaria have gone hand in hand. This highlights the role of malaria in SCD’s history.
In summary, SCD’s history is deeply connected to its role in fighting malaria. Knowing this helps us understand why SCD is found in certain places and how it affects different populations.
Global Distribution of Sickle Cell Disease
Sickle Cell Disease is found all over the world. Its spread is shaped by genetics and how people move. The disease is more common in some places than others.
Regions with High Prevalence
In some areas, like sub-Saharan Africa, the Mediterranean, and parts of Asia, SCD is very common. It’s linked to fighting off malaria.
In sub-Saharan Africa, SCD affects a lot of people. Countries like Nigeria, the Democratic Republic of Congo, and Uganda have high rates. It’s also found in the Mediterranean, like Greece and Turkey, and in India.
Impact of Migration Patterns
Migration has spread Sickle Cell Disease worldwide. People moving from high-prevalence areas bring the disease to new places. This has made SCD more common in Europe and North America.
| Region | Prevalence Rate | Estimated Affected Population |
| Sub-Saharan Africa | 2-3% | Approximately 2 million |
| Mediterranean Region | 1-2% | Around 500,000 |
| Parts of Asia | 1-3% | Nearly 1 million |
Knowing where Sickle Cell Disease is common is key to health care. It helps plan how to deal with the disease. This includes understanding where it’s most common and how it spreads through migration.
Sickle Cell Disease Demographics in the United States
It’s important to know how sickle cell disease affects different racial and ethnic groups in the U.S. This genetic disorder changes how red blood cells make hemoglobin, causing health issues.
In the U.S., SCD isn’t spread evenly. The Centers for Disease Control and Prevention (CDC) says over 90% of those with SCD are non-Hispanic Black or African American. But,it also affects Hispanic Americans and others.
Prevalence Among Different Racial and Ethnic Groups
SCD hits hardest in African communities. It also affects people from the Mediterranean, the Middle East, and India, but less often. The CDC says SCD occurs in about 1 in 365 Black or African American births and 1 in 16,300 Hispanic births.
CDC Statistics on SCD Distribution
The CDC shares vital data on SCD’s spread among racial and ethnic groups. Here’s a table showing SCD’s prevalence in the U.S.:
| Racial/Ethnic Group | Prevalence of SCD |
| Non-Hispanic Black or African American | 1 in 365 births |
| Hispanic | 1 in 16,300 births |
| Other Racial/Ethnic Groups | Less frequent |
The data shows SCD’s big impact on some groups, pointing to the need for focused health efforts. Knowing who SCD affects helps healthcare and policymakers plan better. They can then target resources and initiatives to meet the needs of those affected.
The African American Connection to Sickle Cell Disease
Sickle cell disease is common among African Americans because of the transatlantic slave trade. This event and the genetic patterns that followed have made the disease widespread in this group.
Historical Context and Genetic Inheritance
Sickle cell disease comes from the genes of people from West Africa, where malaria was common. The slave trade brought enslaved Africans to the Americas. They brought their genes, which became a big health problem for their descendants.
Genetic inheritance patterns are key to SCD’s spread. The disease is passed down specially. A person needs two bad genes to have the disease. Carriers, with one good and one bad gene, are usually healthy but can pass the bad gene to their kids.
Current Prevalence in Black American Populations
Today, sickle cell disease is a big worry for African American health. The CDC says SCD affects about 1 in 365 African American babies.
| Ethnic Group | SCD Prevalence (per 1000 births) |
| African American | 2.73 |
| Hispanic | 0.58 |
| White | 0.04 |
This shows how much SCD affects African American communities. Knowing the history and genetics helps us find better ways to help those affected.
Sickle Cell in Caucasian Populations
To understand sickle cell disease in Caucasians, we need to look at data and genetics. Sickle cell disease is common in some groups but can happen to anyone, including Caucasians.
While it’s often linked to African descent, Caucasians can also have it. It’s caused by a genetic change that affects how red blood cells work.
Statistical Data on White Americans with SCD
Knowing how common sickle cell disease is in white Americans is key. The Centers for Disease Control and Prevention (CDC) says most cases are in African Americans. But a lot of cases are also in white Americans.
A study in the American Journal of Hematology showed Caucasians make up a small part of sickle cell disease cases in the U.S. This shows why genetic testing is important for all ethnic groups.
Genetic Pathways for SCD in White Individuals
The genetics behind sickle cell disease in whites are the same as in other groups. It’s an autosomal recessive disorder. This means you need two bad genes, one from each parent, to have the disease.
In Caucasians, the disease can come from mixed ancestry or from areas where malaria was common, like the Mediterranean. Knowing these genetics helps with genetic counseling and screening.
Key factors contributing to SCD in Caucasian populations include:
- Inheritance of sthe ickle cell trait from parents of mixed ethnicity
- Ancestry from regions with high malaria prevalence, such as the Mediterranean
- Genetic mutations that can occur in any population
By looking at data and genetics, doctors can better handle sickle cell disease in Caucasians. This ensures everyone gets the care they need, no matter their ethnicity.
Mediterranean, Middle Eastern, and Indian Variants of Sickle Cell Disease
Sickle Cell Disease affects more than just African Americans. It also impacts people from the Mediterranean, the Middle East, and India. This shows the genetic diversity and historical reasons behind SCD in these areas.
SCD in Mediterranean White Populations
In the Mediterranean, Sickle Cell Disease is found in places like Greece, Turkey, and Italy. It’s linked to specific genetic changes due to historical malaria exposure.
- Genetic Adaptations: SCD in Mediterranean populations is tied to genetic changes that helped fight malaria.
- Prevalence: Research shows SCD is more common in some Mediterranean countries. It’s linked to unique genetic markers different from African ones.
Middle Eastern and South Asian Prevalence
In the Middle East and South Asia, Sickle Cell Disease is also common. Countries like Saudi Arabia, Iran, and India have high rates. The disease here comes from various genetic mutations, affecting severity differently.
- The β-thalassemia trait, when combined with SCD, leads to HbS/β-thalassemia. It’s as severe as homozygous SCD.
- Studies in these areas stress the importance of newborn screening and genetic counseling for disease management.
It’s key to understand Sickle Cell Disease variants in Mediterranean, Middle Eastern, and Indian populations. This helps in creating specific public health plans and proper care for those affected.
Genetic Inheritance Patterns of Sickle Cell Disease
The way Sickle Cell Disease is passed down is key to understanding risks, mainly for those with mixed ancestry. It’s caused by a change in the HBB gene, which affects hemoglobin. This change leads to sickle hemoglobin, or HbS.
Autosomal Recessive Inheritance Explained
Sickle Cell Disease follows an autosomal recessive pattern. This means a person needs two mutated HBB genes, one from each parent, to have the disease. Those who carry one mutated gene, known as Sickle Cell Trait (SCT), usually don’t have symptoms but can pass the gene to their kids.
Key aspects of autosomal recessive inheritance include:
- The disease can affect both males and females equally.
- An individual must inherit two copies of the mutated gene (one from each parent) to express the disease.
- Carriers have a 25% chance of having a child with SCD with each pregnancy if the other parent is also a carrier.
Mixed Ancestry and SCD Risk Assessment
People with mixed ancestry face a complex risk of getting SCD. Knowing the genetic contribution of each parent is key. If both parents carry the mutated HBB gene, their kids are at high risk of getting SCD, no matter their ancestry.
Risk assessment for individuals of mixed ancestry should consider:
- The ethnic background of both parents and their likelihood of being carriers.
- Genetic testing to determine carrier status.
- Family history of SCD or SCT.
A geneticist,says, “Knowing the genetic risks of Sickle Cell Disease is vital for families, even those with mixed ancestry. Genetic counseling offers insights into risks and aids in making informed choices.”
“Genetic counseling is essential for individuals of mixed ancestry who are at risk of having a child with Sickle Cell Disease. It provides them with the information needed to understand their risks and make informed reproductive choices.”
Understanding Sickle Cell Disease’s genetic patterns helps individuals and families assess risks. This knowledge aids in making decisions about genetic testing and family planning.
Diagnosis and Screening Across Racial Groups
Understanding sickle cell disease (SCD) in different racial groups is complex. It involves genetics, demographics, and clinical factors. SCD is common in some groups but also found in others, making a detailed approach to diagnosis necessary.
Current Screening Programs and Guidelines
Screening for SCD focuses on high-risk groups. In many places, like the United States, newborns are screened. This has helped catch the disease early. Bu, screening and diagnosis rules can change based on where you are and the local SCD rates.
Universal newborn screening is keyton finding SCD early. This allows for quick treatment. For those not screened at birth, finding out they have SCD often happens when they show symptoms.
Challenges in Diagnosis for Non-Black Patients
Diagnosing SCD in people from groups with lower rates is hard. The symptoms can be similar to other diseases, making it harder to suspect SCD in non-Black patients. Doctors might also be less likely to think of SCD in these groups, leading to late diagnosis.Doctors need to bee aware of SCD in all groups. Training them on SCD’s genetics and its presence in various populations can help solve these problems.
Treatment Approaches and Research Developments
Treatment for Sickle Cell Disease includes many options, from standard care to new therapies. Managing SCD has gotten better thanks to new research and a better understanding of the disease.
Standard Treatment Protocols
Standard treatment for SCD includes preventive steps, relief for symptoms, and ways to lessen crisis severity. Hydroxyurea is a key drug that helps reduce crisis pain and may lower blood transfusion needs.
Other common practices are:
- Regular blood transfusions to lower stroke risk and other issues
- Managing pain with drugs and other support
- Preventing infections, mainly in kids, with vaccines and antibiotics
| Treatment Approach | Description | Benefits |
| Hydroxyurea Therapy | Medication to reduce the frequency of painful crises | Reduces crises, decreases need for transfusions |
| Blood Transfusions | Regular transfusions to reduce the risk of stroke | Reduces stroke risk, improves oxygen delivery |
Emerging Therapies and Gene Editing
New treatments for SCD are coming, like gene editing. CRISPR/Cas9 gene editing is being tested in early trials. It might fix the genetic problem causing SCD.
Other new methods include:
- Gene therapy to add a healthy HBB gene to stem cells
- Small molecule therapies to fight sickling and improve hemoglobin
- Immunotherapy to tackle SCD-related complications
- These new treatments are in clinical trials. Early results look promising for better SCD outcomes.
Conclusion: Understanding Sickle Cell Disease Beyond Racial Categories
Sickle Cell Disease is a complex genetic disorder found worldwide. It affects many different people, not just those from certain racial groups.
Looking at SCD beyond racial categories is key. It’s found in many ethnic and racial groups, including Caucasians. This shows the genetic complexity and the need for a wide range of treatments.
Good care for SCD patients means understanding its global reach and genetic roots. Healthcare providers need to see SCD in all demographics. This approach helps improve care and outcomes for everyone affected.
FAQ
What is sickle cell disease, and how is it related to race?
Sickle cell disease (SCD) is a genetic disorder that affects how red blood cells carry oxygen. It makes red blood cells misshapen. While it’s more common in certain racial groups, like those of African descent, it’s not exclusive to any race.
Can a white person have sickle cell disease?
Yes, white individuals can have SCD, though it’s less common. The disease can affect anyone, regardless of race or ethnicity.
What are the genetic factors that contribute to SCD in Caucasian populations?
In Caucasian populations, SCD can come from inheriting the sickle cell gene from parents. This can happen if one or both parents carry the gene.
How does the genetic mutation underlying SCD affect hemoglobin production?
The genetic mutation in SCD affects hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen. The mutation leads to abnormal hemoglobin, causing red blood cells to become misshapen.
What is the difference between SCD and sickle cell trait?
SCD means having two sickle cell genes, one from each parent, and showing symptoms. Sickle cell trait means having one sickle cell gene and usually not showing symptoms.
How has natural selection influenced the prevalence of SCD in different populations?
Natural selection has influenced SCD prevalence, mainly in areas where malaria is common. The sickle cell gene offers some protection against malaria.
What are the demographics of SCD in the United States?
The CDC says SCD affects many racial and ethnic groups in the U.S. African Americans are most affected. But it also occurs in Hispanic, Mediterranean, and Middle Eastern individuals.
How do migration patterns affect the genetic spread of SCD?
Migration has spread SCD to new areas. People carrying the sickle cell gene move to different parts of the world.
What are the challenges in diagnosing SCD in non-Black patients?
Diagnosing SCD in non-Black patients is hard. This is because the disease is less common in these groups, leading to delayed or missed diagnoses.
What are the current treatment approaches for SCD?
Treatments for SCD include pain management and blood transfusions. New therapies like gene editing also show promise for better treatment outcomes.
How does the autosomal recessive inheritance pattern of SCD affect individuals of mixed ancestry?
Mixed ancestry individuals may inherit SCD if their parents are carriers. The risk depends on the genetic makeup of both parents.
What is the prevalence of SCD in Mediterranean, Middle Eastern, and Indian populations?
SCD is present in Mediterranean, Middle Eastern, and Indian populations. Different genetic traits and historical contexts contribute to its prevalence in these regions.
Reference
Campbell, A. D., Wilkinson, D. J., Thomas, A. N., & Telfer, P. (2020). An analysis of racial and ethnic backgrounds within the European sickle cell disease population. British Journal of Haematology, National Center for Biotechnology Information. https://pmc.ncbi.nlm.nih.gov/articles/PMC7669607/









