Last Updated on November 20, 2025 by Ugurkan Demir

Sickle cell anemia is often seen as a disease mainly found in people of African descent. But, it’s important to know that it can affect anyone, no matter their race. Sickle cell anemia is not exclusive to any particular race or ethnicity, and it has been found in Caucasians too.Learn about white person sickle cell anemia, its rarity, and whether Caucasians can develop the disease.
Recent data shows that about 1.8% of those hospitalized for sickle cell disease in the U.S. are white. The rate of sickle cell trait in white newborns is much lower, at 3 cases per 1,000 births. This shows why awareness and correct diagnosis are key for all ethnic groups.

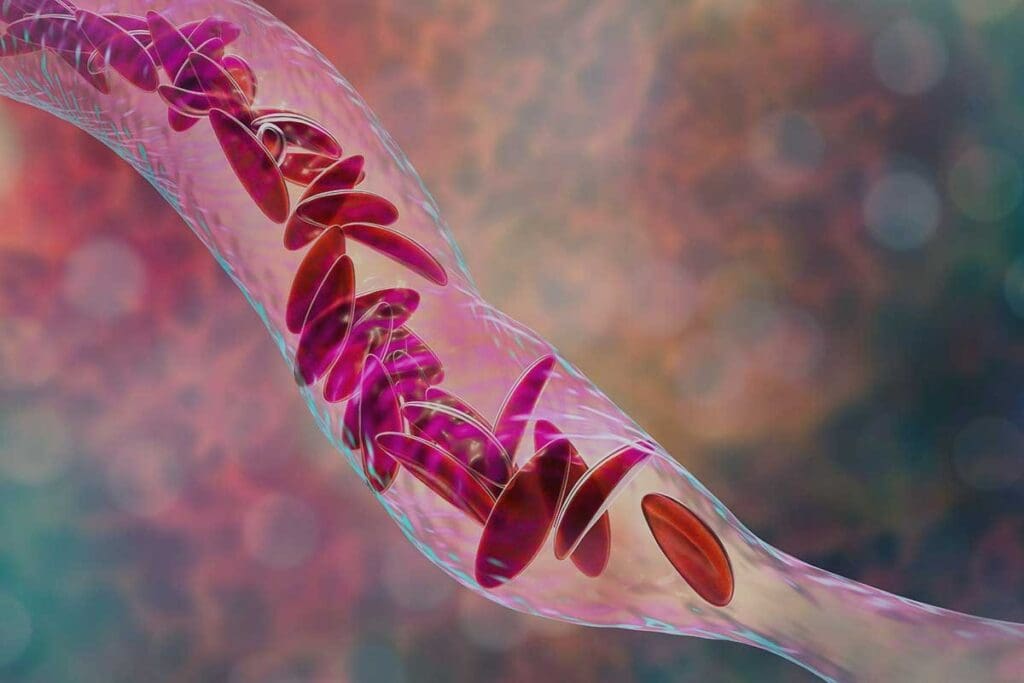
To understand sickle cell anemia, we must look at the genetic mutation. This mutation causes the production of abnormal hemoglobin. This leads to red blood cells that are sickle-shaped.
This genetic disorder comes from a change in the HBB gene. The mutation changes glutamic acid to valine at the sixth position of the beta-globin chain. This change results in sickle hemoglobin or HbS.
The genetic mutation affects hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen. Normally, red blood cells are flexible and disk-shaped, allowing them to move easily.
In sickle cell anemia, the abnormal hemoglobin makes red blood cells sickle-shaped and rigid. This makes it hard for them to pass through small blood vessels.
This rigidity and abnormal shape reduce the cells’ oxygen transport ability. It also increases their chance of getting stuck in smaller vessels. This causes various health problems.
Sickle-shaped red blood cells can significantly affect health. They can get stuck in small blood vessels, causing vaso-occlusive crises. These are episodes of severe pain due to lack of blood flow.
Also, the sickling of red blood cells leads to their premature destruction. This causes anemia.
Sickle cell disease follows an autosomal recessive pattern. This means a person needs two defective hemoglobin genes, one from each parent, to have the disease.
This pattern shows the disease is not linked to sex chromosomes. A single mutated gene is not enough to cause the condition. Carriers of sickle cell disease have one normal and one mutated gene. They usually don’t show symptoms but can pass the mutated gene to their kids.
The chance of inheriting sickle cell disease depends on the parents’ genes. If both parents are carriers, each child has a 25% chance of having the disease. There’s a 50% chance the child will be a carrier, and a 25% chance they won’t have the disease or be a carrier.
It’s important to know the difference between sickle cell trait and sickle cell disease. People with sickle cell trait are carriers with one normal and one sickle hemoglobin gene. They usually live normal lives without the severe symptoms of sickle cell disease. But, they might face some issues under extreme conditions.
Being a carrier of sickle cell disease affects not just the individual but also their family. Carriers are generally healthy but can pass the mutated gene to their children. When both parents are carriers, there’s a higher risk of having a child with sickle cell disease.
| Parental Genotypes | Risk of Sickle Cell Disease in Offspring | Risk of Being a Carrier |
| Both parents are carriers | 25% | 50% |
| One parent is a carrier, the other is not | 0% | 50% |
| One parent has sickle cell disease, the other is a carrier | 50% | 50% (for being a carrier if not having the disease) |
Understanding these genetic risks is key for individuals and families with sickle cell disease. Genetic counseling offers valuable insights. It helps in making informed decisions about family planning.
Sickle cell anemia spreads across the globe in a complex way. It’s shaped by history, genetics, and the environment. This disease isn’t limited to certain places or people, showing how it has traveled with different groups.
The disease started in areas where malaria was common. The sickle cell trait helped protect against malaria. Over time, it spread through migration, slave trade, and other events. Now, it’s found in Africa, the Mediterranean, the Middle East, and parts of Asia.
Sickle cell anemia affects different groups in different ways. In the U.S., it’s more common among African Americans. But it also impacts people from the Mediterranean, Middle East, and South Asia. It’s more common where malaria was once a big problem.
| Ethnic Group | Prevalence of Sickle Cell Trait | Prevalence of Sickle Cell Anemia |
| African American | 8-10% | 1 in 500 |
| Mediterranean | 5-7% | 1 in 1,000 |
| Middle Eastern | 4-6% | 1 in 1,500 |
| South Asian | 3-5% | 1 in 2,000 |
The sickle cell trait helps protect against malaria. This has helped the gene spread in malaria-prone areas. Knowing this helps us understand where sickle cell anemia is found.
Key Points: Sickle cell anemia’s spread is shaped by malaria, migration, and ethnicity. It’s more common in certain groups and places.
Many think Caucasians can’t get sickle cell anemia, but this is not true. Sickle cell anemia is a genetic disorder that can affect anyone, no matter their ethnicity.
The cause of sickle cell anemia is a mutation in the HBB gene. This gene is responsible for hemoglobin. This mutation can happen to anyone, not just based on race.
Many believe sickle cell anemia only affects people of African descent. While it’s true it’s more common in Africans, it also affects people from the Mediterranean, Middle East, and South Asia.
The genetic basis of sickle cell anemia is more important than race. The HBB gene mutation is the main cause, and it can happen to anyone.
Key factors to consider:
There are cases of Caucasian people with sickle cell anemia, mainly those from areas where malaria was common. These cases show the importance of looking at genetics, not just race.
For example, people of Mediterranean descent, like Italians and Greeks, have been diagnosed with sickle cell anemia. These cases remind us to be aware and test for the disease, not just in high-risk groups.
Research shows sickle cell anemia is more common in African Americans. But it’s also found in white Americans. It’s important to know how widespread it is in different groups.
A 2019 study in Michigan found 2.5% of newborns with sickle cell anemia were white. This shows the disease is less common but a big worry. The study also found 3 cases of sickle cell trait per 1,000 births in white babies.
Looking at hospital rates gives us more insight. While more African Americans are hospitalized, white patients also face a significant number of hospitalizations. This shows healthcare providers need to watch for it in all groups.
Comparing sickle cell anemia rates in different groups is key. The disease is more common in African Americans. But in white Americans, it’s also a big issue. This comparison helps in planning better healthcare for everyone.
In summary, the data on sickle cell anemia in white Americans is enlightening. It shows us the disease’s impact, hospital rates, and how it compares in different groups. Knowing this helps in planning better public health and ensuring everyone gets the care they need.
Ancestral risk factors are key in figuring out who might get sickle cell anemia among Caucasians. Even though sickle cell disease is common in people of African descent, others can also be affected. It’s important to know this.
The sickle cell gene isn’t found only in certain ethnic groups. Its spread is tied to history and where people lived. Caucasians with Mediterranean, Middle Eastern, and South Asian ancestry are at higher risk. This is because malaria was common in these areas long ago.
People from the Mediterranean, like Italians, Greeks, or Turks, are more likely to have the sickle cell trait. This is because malaria was once common there. Carrying the sickle cell gene helped people survive malaria.
Research shows the sickle cell gene is found in many Mediterranean populations. This makes genetic testing important for those with this ancestry. Knowing who can get sickle cell is key for early treatment.
Those with Middle Eastern and South Asian ancestry also face a higher risk of having the sickle cell gene. Malaria was once widespread in these areas, leading to more people carrying the gene.
Studies show the sickle cell trait is found in many ethnic groups in these regions. This highlights the need for genetic testing and awareness among these populations.
Migration has greatly influenced the spread of sickle cell anemia. As people moved and mixed, the sickle cell gene spread to new areas. This has made it a global issue.
The gene’s presence in different ethnic groups shows the complex history of human migration. Knowing this history helps us understand and manage the disease better.
Genetic testing for sickle cell anemia is important for more than just those at high risk. It’s also key for Caucasians with certain family or ancestral backgrounds. Even though sickle cell anemia is rare in Caucasians, it’s vital for those with a family history or ancestry from high-risk areas to get screened.
Screening for sickle cell anemia is advised for those with a family history or ancestry from high-risk areas. This includes the Mediterranean, Middle East, or South Asia. Early genetic testing can greatly improve management and treatment of the condition.
Genetic testing for sickle cell anemia analyzes a blood sample for the sickle cell gene. Several methods are available, including:
| Testing Method | Description | Use Case |
| Hemoglobin Electrophoresis | Separates and identifies different types of hemoglobin in the blood | Diagnosing sickle cell anemia and identifying carriers |
| High-Performance Liquid Chromatography (HPLC) | Quantifies different hemoglobin types | Accurate diagnosis and monitoring of sickle cell disease |
| Genetic Testing (DNA Analysis) | Directly examines the HBB gene for mutations | Identifying carriers, prenatal diagnosis, and confirming diagnosis |
It’s important to understand genetic testing results. They can show if someone is a carrier, has sickle cell anemia, or is unaffected.
Carrier Status: Carriers have one normal and one mutated HBB gene. They usually don’t show symptoms but can pass the mutated gene to their children.
Sickle Cell Anemia: Those with two mutated HBB genes have sickle cell anemia. They experience symptoms and complications of the disease.
Genetic counseling is often suggested for carriers or those with sickle cell anemia. It helps discuss the implications and risks to future offspring.
Sickle cell anemia is not just found in African descent. It also affects white patients, making diagnosis tricky. This is because it’s rare in this group, often leading to late diagnosis.
White patients with sickle cell anemia show symptoms like chronic pain, fatigue, and frequent infections. These come from red blood cells sickling. This can cause crises and anemia.
Common complications include:
A study in the Journal of Clinical Hematology found early diagnosis and treatment are key. They help improve patient outcomes (1).
| Complication | Symptoms | Management |
| Acute Chest Syndrome | Cough, chest pain, fever | Oxygen therapy, antibiotics, pain management |
| Stroke | Neurological deficits, headache | Immediate medical attention, transfusion therapy |
Diagnosing sickle cell anemia in white patients is hard because it’s rare. Doctors might not think of it first, causing delays in treatment.
“The diagnosis of sickle cell disease in individuals of European descent is often delayed due to its relative rarity, highlighting the need for increased awareness among healthcare providers.”
These delays can lead to more serious problems. So, doctors should always think of sickle cell anemia, even in white patients.
When diagnosing sickle cell anemia, doctors must look at other conditions too. These include other anemias, inflammatory disorders, and infections.
Differential diagnoses to consider:
Genetic testing and hemoglobin electrophoresis are key to confirming sickle cell anemia. Knowing how to diagnose it helps doctors improve patient care.
Managing sickle cell anemia requires a mix of medical care and lifestyle changes. The aim is to lessen pain episodes, prevent serious issues, and enhance life quality for those affected.
Medical treatments are key in managing sickle cell anemia. Hydroxyurea is a main drug that cuts down on pain episodes and might reduce blood transfusion needs. Other drugs include pain relievers, antibiotics to ward off infections, and meds to lower risk of complications.
Hydroxyurea Therapy boosts fetal hemoglobin production, which lessens red blood cell sickling. Blood transfusions are also vital for some, lowering stroke and other complication risks by reducing sickle-prone red blood cells.
Pain control is critical in treating sickle cell anemia. Pain episodes, or crises, can be intense and need quick action. Treatment plans include pain relievers, from over-the-counter to stronger opioids for severe pain. Patient-controlled analgesia (PCA) is used in hospitals for severe pain.
Effective pain management also means tackling pain causes like infections or dehydration. Healthcare teams work with patients to craft tailored pain management plans, adjusting as needed based on pain severity and frequency.
New treatments for sickle cell anemia are on the horizon, with gene editing like CRISPR/Cas9 showing great promise. Other new treatments aim to reduce pain episodes and boost overall health.
| Therapy | Description | Potential Benefits |
| Gene Editing (CRISPR/Cas9) | Corrects the genetic mutation causing sickle cell anemia | Potential cure, elimination of disease symptoms |
| New Medications | Reduces frequency of pain crises | Improved quality of life, reduced healthcare utilization |
Changing your lifestyle is key in managing sickle cell anemia. Stay hydrated, avoid extreme temperatures, and manage stress. Regular health check-ups are vital for monitoring the disease and adjusting treatment plans.
Preventive care includes getting vaccinated against infections and regular eye exams to catch complications like retinopathy early. Teaching patients to recognize signs of complications and when to seek medical help is also essential.
Sickle cell anemia is a genetic disorder found worldwide. It doesn’t just affect certain ethnic groups. This shows we need to spread awareness and understanding everywhere.
This disease can happen to anyone with the mutated gene. It’s a big health issue. As we’ve seen, it’s not just for certain groups. People of all backgrounds can get it, like Caucasians with specific ancestry.
Managing sickle cell anemia well is key. This includes genetic testing, early diagnosis, and good treatments. By seeing it as a global issue, healthcare can offer fair care to everyone, no matter their background.
Seeing sickle cell anemia as a global issue helps make healthcare more inclusive. It also helps us create better plans to improve life for those affected.
Yes, Caucasians can get sickle cell anemia. It’s just not as common in this group.
No, sickle cell anemia isn’t just for certain groups. It can happen to anyone, no matter their ethnicity.
Sickle cell anemia comes from a genetic mutation. It affects how hemoglobin is made, causing red blood cells to be sickle-shaped.
Yes, white people can carry sickle cell trait. This means they can pass the disease to their kids.
Sickle cell disease is inherited in a specific way. A person needs two defective genes to have the disease.
Sickle cell trait means carrying the disease. Sickle cell disease is when the disease is fully expressed.
Yes, a white person can have sickle cell anemia. It happens if they inherit the right genetic mutations.
Yes, Caucasians with certain backgrounds are at higher risk. This includes those from Mediterranean, Middle Eastern, or South Asian ancestry.
Sickle cell anemia is less common in white Americans than in other groups. But it can happen, mainly in those with specific backgrounds.
White patients with sickle cell anemia face similar symptoms. These include pain crises, infections, and anemia.
Doctors diagnose sickle cell anemia with genetic and blood tests. Treatment includes various medical steps, pain management, and lifestyle changes.
Yes, whites can get sickle cell anemia. It’s important to consider this in diagnosis, regardless of ethnicity.
Yes, white people can get sickle cell anemia. It’s key to be aware of this for early diagnosis and treatment.
Yes, a Caucasian person can get sickle cell anemia. It happens if they have the right genetic mutations.
While exact numbers vary, it’s known that white people can have sickle cell anemia. There’s data on its prevalence among white Americans.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!