Last Updated on November 20, 2025 by Ugurkan Demir

Getting a blood cancer diagnosis can feel scary. But knowing about the treatment can make things easier. Chemotherapy is a key treatment, helping up to 80% of acute leukemia patients get better.Understand chemotherapy for blood cancer, from diagnosis to recovery, including key stages and expected outcomes.
At Liv Hospital, we aim to give top-notch care and support. We help you understand the 7 main stages of chemotherapy. This way, you can face your treatment with confidence.
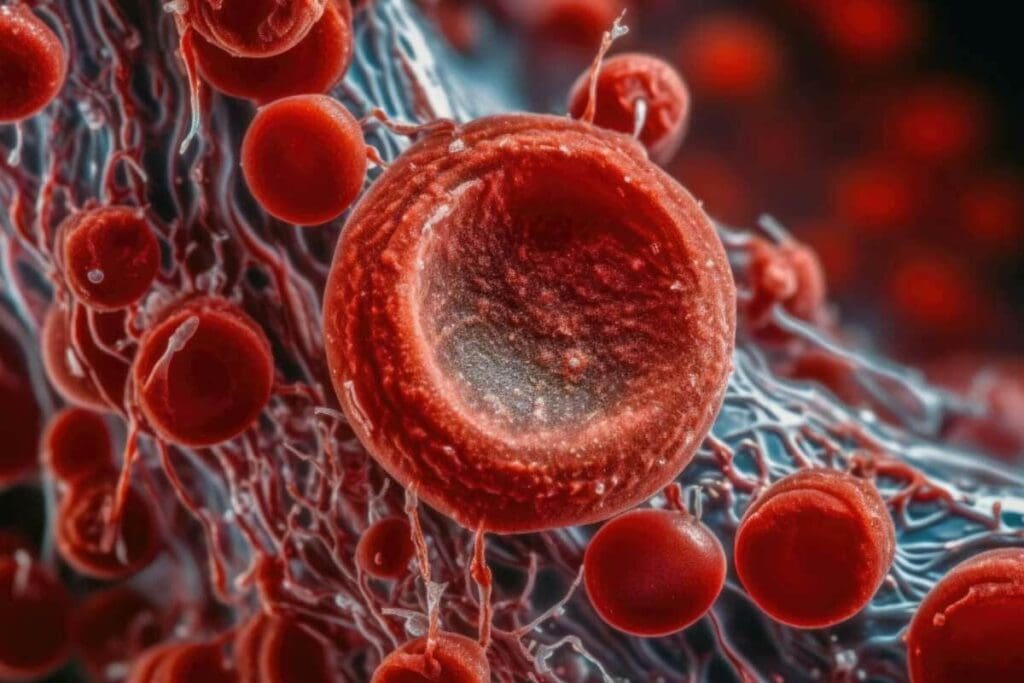
Blood cancer affects the blood, bone marrow, and lymph nodes. It disrupts the body’s ability to fight infections and regulate bleeding. This impacts overall health.
Blood cancers include leukemia, lymphoma, and myeloma. Leukemia causes abnormal white blood cells, leading to infections and anemia. Lymphoma forms tumors in the lymph nodes or lymphoid tissues. Myeloma grows malignant plasma cells in the bone marrow, causing bone damage and immune issues.
Each blood cancer type needs a specific treatment plan. Knowing these differences is key to effective management.
Chemotherapy is a mainstay in treating blood cancers, like leukemia. It uses drugs to kill or stop cancer cells from growing. Chemotherapy can be given orally or through an IV, based on the cancer type and stage.
For chemotherapy for leukemia, treatment plans are very personal. They consider the patient’s health, leukemia type, and genetic details.
Chemotherapy’s success in treating blood cancer depends on several factors. These include the cancer type, stage, and patient response. Remission rates have improved with better chemotherapy and supportive care.
Chemotherapy for leukemia has shown good results, with many patients going into complete remission. The term “define chemo” in leukemia treatment includes the drugs and the care to manage side effects and improve life quality.
Understanding blood cancer and chemotherapy helps patients and doctors create effective treatment plans. This leads to the best possible outcomes.

Chemotherapy, or “chemo,” uses drugs to fight cancer cells. It’s a key treatment for blood cancer. We’ll look at how it works and its role in treating blood cancer.
Chemotherapy uses drugs to kill or slow cancer cells. These drugs can be given in different ways, like through an IV or by mouth. The method depends on the cancer type and stage.
Chemotherapy affects the whole body. This is key for blood cancers, as they spread through the blood. Chemotherapy drugs target fast-growing cells, like cancer cells. But they can also harm other fast-growing cells, causing side effects.
Chemotherapy stops blood cancer cells from growing by damaging their DNA. Different drugs work in different ways:
Knowing how each drug works helps doctors create the best treatment plans for blood cancer patients.
Chemotherapy for blood cancer has changed a lot over time. New drugs and treatments have been developed. Targeted therapies aim to hit cancer cells without harming normal cells.
Supportive care has also improved, helping manage side effects. This makes treatment better for patients. Research is ongoing to find even better, less harmful treatments.
Getting ready for chemotherapy is a key step in treating blood cancer. It involves detailed checks and plans made just for you. This stage is vital for finding the best treatment plan for your specific needs and health.
Before starting chemotherapy, many tests are done to check your health and blood cancer details. These tests help find out if the cancer has spread. Knowing this is important for accurately staging the disease.
Common tests include:
After the initial tests, a treatment plan is made just for you. This plan lists the chemotherapy drugs, how much, and when to take them.
The treatment protocol is tailored to the individual’s:
| Factor | Consideration | Impact on Treatment |
| Type of Blood Cancer | Different types respond differently to chemotherapy | Choice of chemotherapy drugs |
| Stage of Cancer | Affects the intensity and duration of treatment | Dosage and frequency of chemotherapy |
| Patient’s Health | Influences tolerance to chemotherapy side effects | Adjustments in dosage or additional supportive care |
Getting ready for chemotherapy sessions is important. This includes making travel arrangements, having someone with you, and preparing for side effects.
Patients are advised to:
By preparing well for chemotherapy, patients can make the process easier. It’s a team effort between the patient, their healthcare team, and loved ones.
Induction therapy is the first step in treating leukemia with chemotherapy. It’s a key phase aimed at getting the patient into remission. This intense treatment usually lasts about a week.
The main goal of induction therapy is to kill leukemia cells in the blood and bone marrow. This leads to remission. It’s a short phase, lasting 7 to 10 days, with high doses of chemotherapy drugs.
This period can be tough, but it’s vital for recovery. The treatment plan is tailored to the patient’s leukemia type, health, and other factors.
During induction therapy, a mix of chemotherapy drugs is used. These include:
These drugs work together to effectively target and destroy leukemia cells.
After induction therapy, we check how well the treatment worked. This involves bone marrow biopsies and blood tests. Success is when there’s no detectable leukemia in the blood or bone marrow.
| Treatment Phase | Primary Goal | Typical Duration |
| Induction Therapy | Achieve Remission | 1-2 weeks |
| Consolidation Therapy | Eliminate Remaining Cancer Cells | Several Months |
Success rates for induction therapy vary. They depend on the patient’s age, health, and leukemia type. Our medical team closely watches the patient’s response to adjust the treatment plan as needed.
After induction therapy, patients move to consolidation therapy. This stage is key in getting rid of any cancer cells left behind. It’s a critical part of blood cancer treatment, aiming to kill cancer cells that tests can’t find.
Consolidation therapy starts after a patient has fully recovered from the first treatment. Its main goal is to lower the number of cancer cells in the body. This reduces the chance of the cancer coming back. A study on the National Center for Biotechnology Information shows it helps patients live longer with certain blood cancers.
The right time to start consolidation therapy is when the patient’s blood counts are back to normal. The exact timing depends on the treatment plan and the patient’s health.
High-dose chemotherapy is often used in consolidation therapy. The drugs chosen depend on the type of blood cancer. Common drugs include:
The treatment is customized for each patient, based on their cancer and health.
Patients are closely watched during consolidation therapy. Blood tests and bone marrow biopsies check how well the treatment is working. How well consolidation therapy works can predict long-term success.
A study emphasizes the need for careful monitoring. It says treatment might need to be adjusted based on how the patient responds.
“The goal of consolidation therapy is to achieve a deeper remission, improving long-term survival chances.”
| Aspect | Description | Importance |
| Purpose | Kill remaining cancer cells | High |
| Timing | After recovery from induction | High |
| Treatment Methods | High-dose chemotherapy | High |
| Monitoring | Regular blood tests and bone marrow biopsies | High |
Intensification therapy is a key part of treating blood cancer. It aims to make the patient’s response to chemotherapy stronger. This stage is for those who have reached a certain level of remission but need more treatment to lower the risk of cancer coming back.
Intensification therapy can seem complex and scary. It means giving higher doses of chemotherapy or using different drugs to kill more cancer cells.
Intensification therapy is for patients who have done well with initial treatments but are at high risk of cancer coming back. Doctors decide if intensification is needed based on the cancer type, stage, patient’s health, and how well they’ve handled previous treatments.
For example, those with high-risk features or not fully in remission after initial treatments might need intensification. Our team carefully looks at each patient to decide the best treatment plan.
| Factors Influencing Intensification Therapy | Description |
| Type and Stage of Blood Cancer | The specific characteristics of the patient’s blood cancer influence the need for intensification therapy. |
| Patient’s Overall Health | The patient’s general health and ability to tolerate aggressive treatment are key. |
| Response to Previous Treatments | How well the patient has done with initial treatments helps decide if intensification is needed. |
Consolidation and intensification therapies both aim to improve treatment results but in different ways. Consolidation uses similar drugs and doses to get rid of any cancer cells left after initial treatments. Intensification is more aggressive, using higher doses or different drugs to lower the relapse risk even more.
The main goal of intensification therapy is to get a deeper remission, which improves survival chances. Knowing what to expect helps patients prepare for this important treatment phase.
Some expected outcomes include:
We know intensive therapy is tough, both physically and emotionally. Our team is dedicated to supporting our patients through this challenging time, ensuring they get the care and guidance they need.
CNS prophylaxis is key in stopping leukemia from spreading to the brain and spinal cord. Leukemia cells can sneak into these areas, causing big problems. So, keeping the brain and spinal cord safe is a big part of treating blood cancer.
The brain and spinal cord are safe havens for leukemia cells. Some chemotherapy can’t reach these cells well when given by mouth or vein. That’s why CNS prophylaxis is vital to stop or treat CNS involvement.
Intrathecal chemotherapy means putting chemotherapy right into the cerebrospinal fluid around the brain and spinal cord. This way, leukemia cells in the CNS get hit hard, lowering the chance of CNS relapse.
Patients might get lumbar punctures (spinal taps) for intrathecal chemotherapy. We’ll tell you what to expect, like how to prepare and possible side effects.
If leukemia cells get to the brain or spinal cord, chemotherapy is given directly into the CSF. This is a key part of CNS prophylaxis.
| Method | Description | Purpose |
| Intrathecal Chemotherapy | Delivery of chemotherapy drugs directly into the CSF. | To target leukemia cells in the CNS. |
| Lumbar Puncture | A procedure to access the CSF for chemotherapy administration. | To facilitate intrathecal chemotherapy. |
Maintenance therapy is key in managing blood cancer for stages 5-7. It helps keep the cancer in remission after intense treatments.
The maintenance phase is a big part of treating blood cancer. It uses lower doses of chemotherapy or other treatments for a long time. This can last from months to years. The main goal is to keep cancer from coming back by killing any remaining cells.
Patients often take oral chemotherapy during this phase. This makes treatment easier and less disruptive to daily life. Oral chemotherapy, like chemo pills for leukemia, is very important in managing blood cancer.
Oral chemotherapy has changed long-term treatment for blood cancer. Pills or capsules taken daily can work as well as intravenous chemotherapy. Some common drugs include:
| Drug Name | Common Use | Administration |
| Capecitabine | Various cancers | Oral |
| Lenalidomide | Multiple myeloma, certain leukemias | Oral |
| Temozolomide | Brain tumors, certain other cancers | Oral |
A study in a top oncology journal shows oral chemotherapy improves patient compliance and quality of life.
“Oral chemotherapy has become a cornerstone in the management of various cancers, making treatment more manageable for patients.”
Leading Oncology Journal
The length of maintenance therapy depends on the cancer type, patient response, and other factors. Regular check-ups with healthcare providers are key to track treatment success and manage side effects.
During maintenance, patients have regular blood tests, bone marrow biopsies, and other tests. These ensure the cancer stays in remission. Treatment plans may change based on patient response and side effects.
In conclusion, maintenance therapy is essential for blood cancer patients. It requires careful management and ongoing support.
It’s key to know how chemotherapy is given to treat blood cancers. There are many ways to give chemotherapy, each with its own benefits and things to think about.
IV chemotherapy is often used for blood cancers like leukemia. It involves putting chemotherapy drugs directly into a vein. IV chemotherapy lets us give high doses of medicine quickly and well. We choose this for many because it lets us watch and change treatment as needed.
Oral chemotherapy pills are a handy option for some. These pills have chemotherapy drugs that the body absorbs. Patients must stick to a strict schedule for oral chemotherapy to work. We teach our patients about the importance of following their treatment plan and watching for side effects.
Chemotherapy shots or injections are another way to give drugs. They can be given under the skin or into a muscle. This method is not as common for blood cancer, but it might be used in some cases or for certain drugs.
For those needing many chemotherapy sessions, a central line or port might be suggested. These are implanted under the skin for easy access. Central lines and ports cut down on the need for repeated needle sticks and make treatment easier. We talk with our patients about the pros and cons of these devices to see if they’re right for them.
Understanding chemotherapy for blood cancer is key for patients. Blood cancer treatment has grown a lot, giving new hope to those affected.
We’ve talked about the seven main stages of chemotherapy. This includes everything from starting treatment to keeping it going. There are different ways to get chemotherapy, like through an IV or pills you swallow. Kimo treatment, or chemotherapy, is important for fighting blood cancer cells and getting into remission.
Thanks to new ways of treating blood cancer, more people are living with the disease and getting better. We urge patients to team up with their healthcare team. This way, they can understand their treatment better and make smart choices about their care.
Knowing about treatment options and what to expect helps patients deal with blood cancer treatment. We aim to give full support and top-notch healthcare to patients from around the world. They are looking for the best medical treatments.
Chemotherapy for blood cancer uses medicines to kill cancer cells. It targets cells that grow fast, like cancer cells, and stops them from growing.
Chemotherapy for blood cancer has several stages. These include induction, consolidation, intensification, CNS prophylaxis, and maintenance. Each stage has its own goals and treatment methods.
Induction therapy is the first step in chemotherapy. It aims to get rid of cancer cells. Its main goals are to reduce cancer cells to undetectable levels and help blood cells produce normally again.
CNS prophylaxis protects the brain and spinal cord from leukemia cells. It’s needed because leukemia cells can hide in these areas. This treatment helps prevent cancer from coming back.
Chemotherapy can be given in several ways. These include IV infusions, oral pills, shots, and through central lines or ports. The method chosen depends on the cancer type, treatment plan, and patient needs.
Maintenance therapy is the last stage of chemotherapy. It aims to keep cancer away and prevent it from coming back. How long it lasts varies based on the cancer type and treatment plan. It can last from months to years.
Side effects of chemotherapy for blood cancer include fatigue, hair loss, nausea, vomiting, and a higher risk of infections. Our team will help manage these side effects and provide support.
Success is measured by looking at response rates, remission rates, and survival rates. Regular tests and assessments will check how well the treatment is working.
Chemotherapy can cure some blood cancers, often when used with other treatments. Our team will talk about your chances and treatment options with you.
Chemotherapy is key in treating leukemia. It kills cancer cells and helps achieve remission. It’s often used with other treatments, like targeted therapy or bone marrow transplants.
Chemotherapy shots, or injections, deliver medications directly into the body. They’re used to treat blood cancer, mainly when other methods like oral or IV aren’t suitable.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!