Recent studies show that nearly 1 in 5 adults over 65 get joint replacement surgery in their life.
The top surgeries for older adults are hip replacements and knee replacements. These are often needed because of age-related wear and tear or breaks.
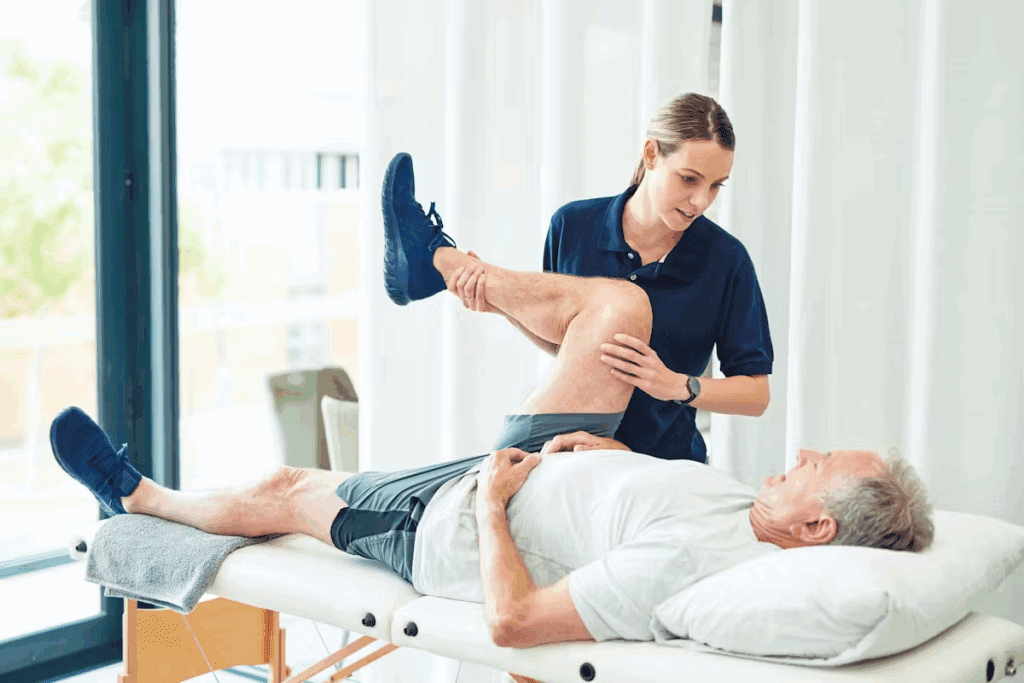
These surgeries are key to bettering the lives of older adults. They help with mobility issues and pain caused by musculoskeletal problems.
Key Takeaways
- Joint replacement surgeries are common among older adults.
- Hip and knee replacements are the most frequent orthopedic operations.
- Age-related degenerative changes often necessitate these surgeries.
- Orthopedic surgeries improve the quality of life for older adults.
- Understanding common orthopedic surgeries helps healthcare providers and patients make informed decisions.
The Landscape of Orthopedic Surgery for Seniors

As the world’s population gets older, more seniors need orthopedic surgery. This is because more people have musculoskeletal issues with age. Also, new surgical methods make these operations more available to older adults.
Current Statistics on Orthopedic Procedures in Older Adults
Recent studies show a big jump in orthopedic surgeries for the elderly. Hip replacements, knee replacements, and spinal surgeries are the most common. The numbers are expected to keep going up as more people get older.
| Orthopedic Procedure | Number Performed Annually | Projected Increase by 2030 |
| Hip Replacements | 300,000 | 50% |
| Knee Replacements | 650,000 | 60% |
| Spinal Surgeries | 200,000 | 40% |
Age-Related Musculoskeletal Changes Necessitating Surgery
As people get older, their bones and muscles change. This can lead to the need for surgery to fix problems and ease pain. Conditions like osteoporosis and degenerative joint diseases are common in seniors, making surgery a key part of their care.
Doctors usually suggest surgery when other treatments don’t work. It’s important for healthcare providers to understand these changes. This way, they can give the best care to seniors.
Hip Replacement: The Most Common Orthopedic Surgery Among Seniors

As more people get older, hip replacement surgery becomes a key treatment for severe hip arthritis and fractures. This surgery replaces the damaged hip joint with an artificial one. It helps reduce pain and improve movement.
Types of Hip Replacement Procedures
Hip replacement surgery comes in different forms, each suited to a patient’s needs. The main types are:
- Total Hip Arthroplasty (THA): This is the most common, where both the acetabulum and femoral head are replaced.
- Hemiarthroplasty: Only the femoral head is replaced, often for certain hip fractures.
- Minimally Invasive Hip Replacement: This method causes less tissue damage, leading to faster recovery.
Indications for Hip Replacement in Elderly Patients
Elderly patients often need hip replacement surgery for several reasons. These include:
- Severe osteoarthritis
- Rheumatoid arthritis
- Hip fractures
- Avascular necrosis
These conditions can greatly reduce a person’s quality of life. Surgery offers a way to relieve pain and restore function.
Technological Advances in Hip Arthroplasty
New technologies have greatly improved hip replacement surgery outcomes. Some key advancements are:
- Computer-Assisted Navigation: Makes implant placement more precise.
- Advanced Materials: New materials in implants last longer and work better.
- Minimally Invasive Techniques: Shorten recovery time and reduce scars.
These advancements have made hip replacement a more effective and appealing choice for older patients.
Knee Replacement Surgery: A Close Second
Knee replacement surgery is a common treatment for severe knee arthritis in seniors. It helps to reduce chronic pain and improve mobility. This is for those whose knees are badly damaged by arthritis or injury.
Partial vs. Total Knee Replacement
There are two types of knee replacement surgery: partial and total. Partial knee replacement only fixes the damaged part of the knee. It’s for patients with arthritis in just one part of the knee.
Total knee replacement replaces the whole knee joint. It’s for those with arthritis in many parts of the knee. This is more common in seniors because their arthritis often affects more of the knee.
When Knee Replacement is Recommended for Seniors
Knee replacement surgery is considered when other treatments don’t work. For seniors, it depends on their health, other medical conditions, and their ability to recover. They must be able to do the exercises needed after surgery.
Good candidates for surgery have a lot of pain and trouble doing everyday things. The surgery can greatly improve their life by reducing pain and making it easier to move.
Recovery Timeline for Elderly Knee Replacement Patients
The recovery time for elderly patients varies. It depends on their health, age, and how well they follow their recovery plan. Most can start moving around and doing daily tasks again in 6 to 12 weeks.
Right after surgery, they focus on managing pain, taking care of the wound, and starting to move. Physical therapy is key to getting back strength, flexibility, and range of motion. The therapy plan is made just for each patient’s needs and progress.
Hip Fracture Repair: Emergency Orthopedic Care for Seniors
Hip fractures in seniors are a big health problem. They often happen from falls and need quick surgery. As more seniors live longer, hip fractures and surgery needs are growing.
Types of Hip Fractures Common in Older Adults
Seniors can get different hip fractures. Femoral neck fractures happen just below the femur head. Intertrochanteric fractures occur between the trochanters of the femur. Knowing these types helps doctors choose the right surgery.
Surgical Approaches to Hip Fracture Repair
Choosing a surgery for hip fractures depends on several things. These include the fracture type, the patient’s health, and bone quality. Doctors might use internal fixation or arthroplasty.
Arthroplasty is often best for seniors, like those with femoral neck fractures. It fixes the fracture and helps with movement and pain.
Post-Surgical Outcomes in Elderly Patients
Results after hip surgery in seniors vary. They depend on health before surgery, the surgery type, and care after. Surgery aims to improve function, lessen pain, and help move early.
Good care after surgery includes managing pain, therapy, and watching for problems. With the right care, many seniors can get back to their old activities.
Shoulder Replacement Surgery in the Elderly Population
The elderly are now getting more benefits from shoulder replacement surgery. This surgery helps with severe shoulder arthritis and fractures. It greatly improves their quality of life.
Shoulder replacement surgery, or shoulder arthroplasty, replaces the damaged or arthritic shoulder joint with an artificial one.
Indications for Shoulder Arthroplasty in Seniors
Seniors are often considered for shoulder replacement surgery if they have severe shoulder pain. This pain doesn’t go away with conservative treatments. Common reasons include:
- Severe osteoarthritis or rheumatoid arthritis
- Comminuted fractures of the proximal humerus
- Avascular necrosis of the humeral head
- Failed previous shoulder surgery
These conditions make daily activities hard. Shoulder arthroplasty can help a lot with pain and improve how well they can move.
Types of Shoulder Replacement Procedures
There are different shoulder replacement procedures for different needs:
- Total Shoulder Arthroplasty (TSA): Replaces both the humeral head and the glenoid surface with prosthetics.
- Reverse Shoulder Arthroplasty (RSA): Reverses the ball and socket for those with rotator cuff issues.
- Hemi-Arthroplasty: Replaces only the humeral head, used for some fractures or when the glenoid is okay.
Each procedure has its own use and benefits. The right one depends on the patient’s condition and the surgeon’s choice.
Recovery Considerations for Older Adults
Recovering from shoulder replacement surgery needs a good rehabilitation plan. Older adults should focus on:
- Managing pain after surgery
- Moving early to avoid stiffness
- Physical therapy to build strength and mobility
- Dealing with possible complications like infection or dislocation
Older adults might need extra help during recovery. This includes help with daily tasks and making their home safer.
Spine Surgery Options for Seniors
Spine surgery for seniors has grown, with many options to ease pain and boost life quality. As more people age, spinal problems needing surgery rise. Knowing the surgery choices is key for doctors and patients to make smart decisions.
Lumbar Decompression and Fusion
Lumbar decompression and fusion are top spine surgeries for seniors. Lumbar decompression eases nerve pressure, while fusion joins vertebrae for stability. These are often for issues like lumbar stenosis and degenerative disc disease.
The perks of these surgeries include:
- Pain relief
- Improved mobility
- Enhanced quality of life
Cervical Spine Procedures in Older Adults
Cervical spine surgeries tackle problems like cervical stenosis and myelopathy. These can cause a lot of pain and neurological issues in older adults. Options include anterior cervical discectomy and fusion (ACDF) or cervical laminectomy.
These surgeries bring many benefits, such as:
- Relief from pain and discomfort
- Improvement in neurological function
- Enhanced overall well-being
Minimally Invasive Spine Surgery Benefits for Elderly Patients
Minimally invasive spine surgery (MISS) is popular among the elderly. It offers smaller cuts, less tissue damage, and quicker healing. MISS can be used for many spinal surgeries, making it a gentler option than traditional surgery.
| Procedure | Benefits | Typical Recovery Time |
| Lumbar Decompression | Pain relief, improved mobility | 2-4 weeks |
| Cervical Spine Surgery | Relief from pain, improved neurological function | 4-6 weeks |
| Minimally Invasive Spine Surgery | Less tissue disruption, quicker recovery | 1-3 weeks |
In summary, spine surgery for seniors offers many options tailored to their needs. By knowing these procedures and their benefits, doctors can give personalized care. This improves outcomes and life quality for elderly patients.
Orthopedic Surgery Seniors: Special Considerations and Risks
Orthopedic surgery for seniors needs a detailed plan, taking into account their health and risks. As more older adults have surgery, it’s important to understand the unique challenges they face.
Pre-Existing Conditions Affecting Surgical Decisions
Older adults often have several health issues that can affect surgery and recovery. For example, diabetes can slow down wound healing, and heart disease may lead to complications during surgery.
It’s vital to assess these conditions before surgery. This might mean adjusting medications, making lifestyle changes, or even delaying the surgery to improve the patient’s health.
| Pre-Existing Condition | Potential Impact on Surgery | Management Strategy |
| Diabetes | Impaired wound healing, increased infection risk | Optimize blood glucose control, monitor post-operative wound healing |
| Heart Disease | Increased risk of cardiovascular complications | Cardiac evaluation, adjust medications as necessary |
| COPD | Respiratory complications during and after surgery | Pulmonary function tests, optimize respiratory therapy |
Anesthesia Considerations for Geriatric Patients
Anesthesia for older adults needs careful thought due to age-related changes and health issues. The right anesthetic can greatly affect the outcome. Older patients may react differently to anesthetics, so doses need to be adjusted and monitored closely.
Using regional anesthesia, like epidurals or nerve blocks, can be beneficial. It may reduce the need for general anesthesia and lower the risk of cognitive problems after surgery.
Risk Assessment and Mitigation Strategies
Assessing and reducing risks is key for seniors having orthopedic surgery. A team of healthcare professionals, including surgeons and anesthesiologists, is essential.
Strategies to lower risks include:
- Comprehensive preoperative evaluation
- Optimization of pre-existing conditions
- Careful selection of surgical and anesthetic techniques
- Postoperative monitoring and care in appropriate settings (e.g., intensive care unit, step-down unit)
- Early mobilization and rehabilitation
By understanding and addressing the special needs and risks of seniors in orthopedic surgery, healthcare providers can improve outcomes and quality of life for this growing group.
Osteoporosis-Related Orthopedic Surgeries
As more people get older, surgeries for osteoporosis are becoming more common. Osteoporosis weakens bones, making them more likely to break. For older adults, these breaks can really hurt their quality of life. That’s why surgery is often needed.
Vertebral Compression Fracture Treatments
Vertebral compression fractures are a big problem for people with osteoporosis. Doctors use vertebroplasty and kyphoplasty to fix these fractures. These are small surgeries that help stabilize the vertebra and ease pain.
Wrist Fracture Repair in Osteoporotic Bone
Fixing wrist fractures in people with osteoporosis is tough because their bones are weak. Doctors use specialized techniques and special implants to fix the wrist. This helps it heal and stay stable.
Surgical Considerations for Fragile Bone
When surgery is needed for osteoporotic bone, doctors have to be very careful. They might use reinforced implants, bone cement, and other methods. This helps ensure the bone heals well and reduces the chance of problems.
It’s important for healthcare providers to understand these surgical needs. This way, they can give the best care to elderly patients with osteoporosis.
Arthroscopic Procedures for Seniors
Arthroscopic surgery is changing how we treat joint problems in seniors. It’s a less invasive way to diagnose and treat issues. As more seniors live longer, we need better and quicker treatments.
Common Arthroscopic Surgeries in Older Adults
Seniors often get arthroscopic surgery for common joint problems. Some common surgeries include:
- Meniscal tear repairs
- Rotator cuff repairs
- Synovectomy for rheumatoid arthritis
- Loose body removal
These surgeries help reduce pain, improve function, and enhance quality of life for seniors.
Benefits of Minimally Invasive Approaches
Arthroscopic surgery offers many benefits for seniors:
- Reduced Recovery Time: It causes less damage, leading to faster healing.
- Less Post-Operative Pain: Smaller cuts mean less pain after surgery.
- Lower Risk of Complications: It’s less likely to cause infections or other problems.
A study in a Journal found it greatly helps seniors. It improves their function and reduces the need for bigger surgeries.
“Arthroscopic surgery is key for elderly patients. It’s less invasive, which means less recovery time and fewer complications.” – An Orthopedic Surgeon
Appropriate Patient Selection Criteria
Choosing the right patients for arthroscopic surgery is important. Consider:
- The patient’s overall health status
- The severity of the orthopedic condition
- Previous treatments and their outcomes
- Patient expectations and lifestyle
Healthcare providers must carefully evaluate these factors. This ensures arthroscopic surgery is the best choice for seniors.
Preparing for Orthopedic Surgery as an Older Adult
Older adults going through orthopedic surgery must prepare well. This ensures a smooth recovery. It’s important to reduce risks and get the best results from geriatric orthopedic surgery.
Pre-Surgical Assessments and Testing
Before surgery, older adults get many tests. These tests check for health risks. They make sure the patient is ready for surgery.
- Comprehensive Medical History: A detailed look at the patient’s health history.
- Physical Examination: A check-up to see how healthy the patient is.
- Laboratory Tests: Blood tests to check the patient’s health.
- Imaging Studies: X-rays and MRIs to see the bones and joints.
Medication Management Before Surgery
Managing medications before surgery is very important. Some medicines might need to be changed or stopped.
Key Considerations:
- Blood thinners might need to be stopped to avoid bleeding during surgery.
- Diabetes medicines might need to be adjusted based on the surgery time.
- Some medicines, like steroids, might need to be kept or changed with doctor advice.
Home Preparation for Post-Surgical Recovery
Getting the home ready is key for a good recovery. Older adults should think about these steps:
- Arrange for Support: Make sure someone can help during the first recovery days.
- Modify the Home Environment: Remove dangers, put in grab bars, and make things easy to reach.
- Prepare Meals in Advance: Cook and freeze meals for easy reheating during recovery.
- Set Up a Recovery Area: Make a comfy area with pillows, blankets, and medicines.
By preparing well, older adults can have better surgery results and recovery.
Recovery and Rehabilitation After Orthopedic Surgery
Orthopedic surgery is just the start for seniors. They need a full recovery and rehabilitation to get the best results. This process includes immediate care, physical therapy, and knowing what to expect in the long run.
Immediate Post-Operative Care
The first days after surgery are key for a good recovery. Effective pain management is very important. It lets patients start moving and doing exercises early.
Doctors use many ways to control pain, like medicine and ice. They also teach patients to watch for signs of problems and when to get help fast.
Physical Therapy Protocols for Seniors
Physical therapy is very important for seniors. It helps them get stronger, move better, and function well. The therapy plans are made just for each patient, based on their surgery and health.
Seniors might do exercises to move better, get stronger, and balance better. The goal is to help them do everyday things again and stay independent.
| Phase | Goals | Interventions |
| Immediate Post-Op | Pain management, wound care | Medication, dressing changes |
| Early Rehabilitation | Restore range of motion, strength | Physical therapy exercises |
| Late Rehabilitation | Improve function, mobility | Advanced physical therapy, gait training |
Long-Term Recovery Expectations
Knowing what to expect in the long run is important. The time it takes to recover can vary a lot. It depends on the surgery, the patient’s age and health, and how well they follow the therapy plan.
Seniors usually see big improvements in the first few months. They keep getting better over time. Recovery can take from 3 to 12 months, based on the surgery and the patient.
With the right care, including immediate needs, physical therapy, and understanding long-term recovery, seniors can do well after surgery.
The Role of Orthopedic Specialists in Senior Care
As more people get older, the need for orthopedic specialists grows. These experts help older adults with bone and joint problems. These issues can really affect their quality of life.
Finding the Right Orthopedic Surgeon for Elderly Patients
Finding the right orthopedic surgeon is very important for seniors. Look for someone with experience in geriatric orthopedic surgery. They should also care about the patient’s needs.
The best surgeon will know how to handle older adult bone surgery. They should understand how to manage other health issues too.
The Multidisciplinary Approach to Geriatric Orthopedics
Geriatric orthopedic care works best when everyone works together. This means doctors, nurses, and physical therapists all play a part. They make sure the patient gets the best care.
- Preoperative assessment and optimization of the patient’s medical condition
- Postoperative care and rehabilitation planning
- Management of chronic conditions that may impact surgical outcomes
This team effort makes sure the patient’s health is fully considered. It leads to better care for orthopedic care elderly patients.
Communication Between Healthcare Providers
Good communication is key for caring for older adults with orthopedic surgery. It’s important to share patient information and treatment plans clearly.
Clear and consistent communication helps avoid mistakes. It makes sure everyone is on the same page. This improves patient safety and results.
Decision-Making Process for Orthopedic Surgery in Seniors
Deciding on orthopedic surgery is a big deal for seniors. It’s about checking their health, how bad their condition is, and the surgery’s pros and cons.
Balancing Risks and Benefits
Seniors and doctors must think hard about surgery. They look at how well it might work, possible problems, and how it could change their life.
Key factors to consider:
- The severity of the orthopedic condition
- The patient’s overall health and comorbidities
- The chance for better function and less pain
- The risks of surgery and anesthesia
Family Involvement in Surgical Decisions
Family members are key in deciding on surgery for seniors. They share insights on what the patient wants and needs.
Family involvement can help in:
- Understanding the patient’s wishes and priorities
- Assessing the patient’s support system at home
- Helping talk to healthcare providers
Shared Decision-Making Models
Shared decision-making means working together. It includes doctors, patients, and families to make informed choices about surgery. This way, the patient’s wishes are respected.
| Components of Shared Decision-Making | Description |
| Patient Education | Providing patients with accurate and understandable information about their condition and treatment options. |
| Patient Preferences | Understanding the patient’s values, goals, and priorities. |
| Healthcare Provider Expertise | Utilizing the healthcare provider’s knowledge and experience to inform decision-making. |
Using shared decision-making, seniors and their families can make better choices about surgery. They balance risks and benefits for the best results.
Quality of Life Improvements After Orthopedic Surgery
Orthopedic surgery does more than just fix bones. It changes daily life for older adults in big ways. These surgeries help seniors live better, keeping them independent and happy.
Functional Outcomes in Daily Activities
Orthopedic surgery helps seniors do everyday things easier. It fixes muscle and bone problems, making daily tasks simpler. This means they can take care of themselves and enjoy hobbies and social events.
For example, hip surgery lets seniors walk without pain. Knee surgery helps them climb stairs and stand longer. These changes can make a big difference, keeping them independent at home.
| Activity | Pre-Surgery Difficulty | Post-Surgery Improvement |
| Walking | Significant pain | Able to walk further without pain |
| Climbing Stairs | Difficulty climbing | Able to climb with greater ease |
| Standing | Limited standing time | Able to stand for longer periods |
Pain Reduction and Mobility Gains
Orthopedic surgery also reduces pain and boosts mobility. It fixes problems that cause pain and limit movement. This lets seniors live more active lives, improving their health and happiness.
“The biggest improvement I’ve seen in my patients after orthopedic surgery is not just the reduction in pain, but the regain in their independence and confidence.” – An Orthopedic Surgeon
For instance, shoulder surgery helps seniors move their shoulders again. They can play golf or garden. Back surgery relieves pain, so they can move without discomfort.
Psychological Benefits of Restored Function
The mental benefits of orthopedic surgery are huge. Feeling better physically boosts mental health. It reduces anxiety and depression, making seniors happier and more confident.
Being able to do things they love also boosts self-esteem. This makes life more fulfilling, as they can keep doing what they enjoy.
Healthcare providers should talk about these benefits. This helps older adults make informed choices about their care.
Emerging Trends in Geriatric Orthopedic Surgery
Recent years have brought big changes in geriatric orthopedic surgery. These changes are making care for older adults better. They make surgeries more precise and improve seniors’ quality of life.
Robotic-Assisted Surgery for Seniors
Robotic-assisted surgery is getting more common in geriatric orthopedic surgery. It brings enhanced precision for better implant placement and fewer complications. Research shows it leads to better functional outcomes and quicker recovery for the elderly.
- Improved accuracy in implant placement
- Reduced risk of surgical complications
- Faster recovery times
Biologics and Regenerative Medicine Applications
Biologics and regenerative medicine are new trends in geriatric orthopedic surgery. They use the body’s healing powers to fix damaged tissues and grow bone. Biologics like platelet-rich plasma (PRP) therapy help heal orthopedic injuries and improve surgery results.
“The integration of biologics and regenerative medicine into orthopedic surgery represents a significant shift towards more holistic and patient-centered care.” – An Orthopedic Surgeon
Personalized Implant Technology
Personalized implant technology is changing geriatric orthopedic surgery. It uses advanced imaging and 3D printing to make customized implants for each patient. This approach can lead to improved implant longevity and better results for elderly patients.
| Trend | Benefits |
| Robotic-Assisted Surgery | Enhanced precision, reduced complications, faster recovery |
| Biologics and Regenerative Medicine | Promotes natural healing, improves surgical outcomes |
| Personalized Implant Technology | Customized implants, improved longevity, better outcomes |
Conclusion: Making Informed Decisions About Orthopedic Surgery in Later Life
Orthopedic surgery can change a senior’s life, easing pain and boosting mobility. This article has covered many procedures, like hip and knee replacements, and spine surgery for seniors. Making the right choice is key, weighing risks, benefits, and personal wishes.
Understanding orthopedic surgery helps seniors and doctors make better decisions. They look at health conditions, surgery’s benefits, and how recovery works. Good communication between patients, families, and doctors is vital.
Geriatric orthopedic surgery focuses on the unique needs of older adults. This approach helps seniors make informed choices. It leads to better health and a better life.
FAQ
What are the most common orthopedic surgeries performed on older adults?
Older adults often get hip and knee replacements, and spinal surgeries. These are needed because of age-related wear and tear, fractures, or conditions that make it hard to move and hurt.
What are the different types of hip replacement procedures available for seniors?
Seniors have several hip replacement options. These include total hip arthroplasty and hemiarthroplasty. New technologies like minimally invasive surgery and computer-assisted navigation help make recovery faster and better.
When is knee replacement surgery recommended for seniors?
Knee replacement is suggested for seniors when other treatments don’t help with severe arthritis. It can greatly reduce pain and improve how well the knee works.
What are the common types of hip fractures in older adults?
Older adults often get femoral neck fractures and intertrochanteric fractures. Doctors use surgery like internal fixation or arthroplasty, depending on the fracture and the patient’s health.
What are the indications for shoulder arthroplasty in seniors?
Shoulder arthroplasty is for seniors with severe pain and loss of function that can’t be fixed with other treatments. There are different types of shoulder replacements, like total shoulder arthroplasty and reverse shoulder arthroplasty.
What are the benefits of minimally invasive spine surgery for elderly patients?
Minimally invasive spine surgery is good for elderly patients. It leads to quicker recovery and less damage to tissues. It’s a great option for treating lumbar stenosis and degenerative disc disease.
How do pre-existing medical conditions affect orthopedic surgery in seniors?
Conditions like diabetes, heart disease, and COPD can change how surgery is planned and how it goes. Doctors need to think carefully and manage these conditions well.
What are the surgical considerations for osteoporotic bone?
When dealing with osteoporotic bone, special implants and techniques are used. This is important for fixing vertebral compression fractures and wrist fractures.
How can older adults prepare for orthopedic surgery?
Getting ready for surgery means doing tests and assessments before, managing medications, and preparing your home for recovery. It’s also important to have support and make your home safe.
What is the role of physical therapy in recovery after orthopedic surgery?
Physical therapy is tailored to each patient. It helps get them moving and functioning again. It’s a key part of getting better after surgery.
How do orthopedic specialists contribute to the care of older adults?
Orthopedic specialists help with both surgery and non-surgery options for musculoskeletal problems. They work with other doctors to give the best care for older adults.
What are the emerging trends in geriatric orthopedic surgery?
New trends include robotic surgery, biologics, and regenerative medicine. There’s also personalized implant technology. These advancements make surgeries more precise and effective.
References
- Schmitt, J., & Smith, A. B. (2024). Trends in orthopedic surgery on patients 90 years old and older: A decade review. Geriatric Orthopaedic Surgery & Rehabilitation, 15, 2151459324123456. https://pmc.ncbi.nlm.nih.gov/articles/PMC11938363/




































