Last Updated on November 20, 2025 by Ugurkan Demir

Polycythemia is a condition where there’s too many red blood cells. It’s measured by high hemoglobin and hematocrit levels. There are two main types: primary and secondary.Learn which of the following would not lead to polycythemia and factors that influence red blood cell disorders.
Primary polycythemia, or polycythemia vera, is a blood cancer. It makes the bone marrow produce too many blood cells.
Liv Hospital is known for its focus on patients. They explain what causes polycythemia. This helps patients understand their health better. Getting the right diagnosis and treatment is key for good care.
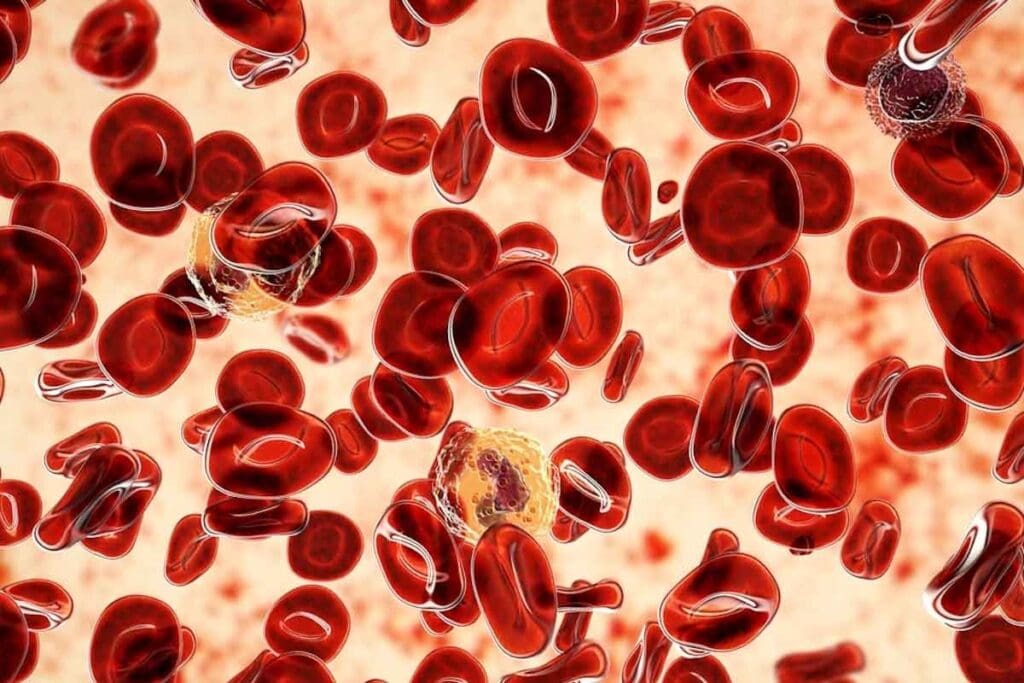
To understand polycythemia, we need to know its definition, how it’s diagnosed, and why it’s a concern. This condition makes the body produce too many red blood cells. This can cause serious health problems.
Polycythemia is when the body makes too many red blood cells. Doctors check for this by looking at hemoglobin and hematocrit levels. For polycythemia vera, a specific type, these levels are key.
Diagnostic markers like hemoglobin and hematocrit are important. Hemoglobin shows how much hemoglobin is in the blood. Hematocrit shows what part of the blood is red blood cells.
Directly measuring red blood cell mass is hard. So, doctors use hemoglobin and hematocrit levels instead. High levels of these can mean polycythemia.
Too many red blood cells can make blood thicker. This can lead to blood clots and heart problems. It’s important to understand this to manage polycythemia well.
Polycythemia can be primary, like in polycythemia vera, or secondary from things like low oxygen. Finding out why it happens is key to treating it right.
Polycythemia is divided into primary, secondary, and apparent types. Each type has its own cause and treatment. Knowing the differences is key for proper care.
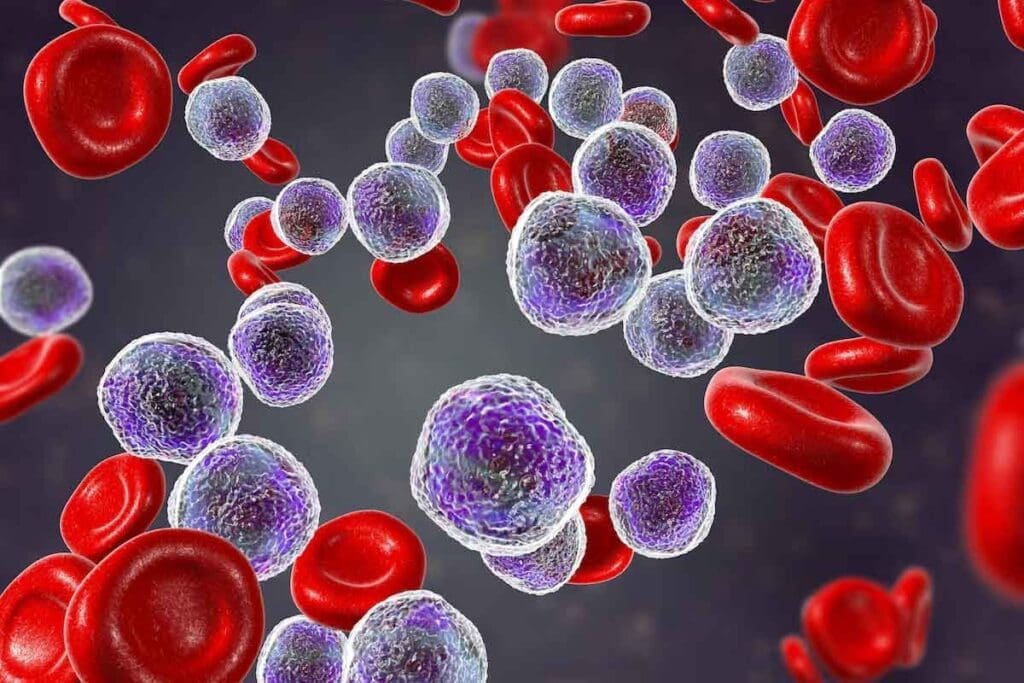
Primary polycythemia, or polycythemia vera (PV), is a blood disorder. It happens when too many red and white blood cells and platelets are made. Polycythemia vera often has a specific gene mutation. This mutation makes cells grow too much.
Secondary polycythemia is caused by external factors. It happens when the body doesn’t get enough oxygen. This can be due to lung diseases or living at high altitudes.
Other reasons include tumors that make too much of a hormone. This hormone helps make red blood cells. Erythropoietin therapy can also cause this.
Apparent polycythemia is when blood looks thicker than it is. This is because of less fluid in the blood, not more red blood cells. It’s important to tell the difference to avoid wrong treatments.
In summary, knowing the types of polycythemia is critical. It helps doctors give the right treatment. This leads to better health outcomes for patients.
It’s important to know the causes and how primary polycythemia works. This condition, also known as polycythemia vera (PV), makes too many red and white blood cells and platelets. This is because of a problem in how cells grow.
A key sign of polycythemia vera is a JAK2 gene mutation. This mutation changes the JAK2 protein, making it always active. This leads to more blood cells being made, even without the need for them.
This JAK2 V617F mutation is found in about 95% of PV patients. It’s a key marker for the disease. The amount of this mutation can affect how the disease acts and the risk of blood clots.
While the JAK2 V617F mutation is common, other genes also play a part. Genes like MPL and CALR are involved in some cases. These genes affect how blood cells are made, leading to more cells.
Polycythemia vera is caused by a problem with blood stem cells. These cells start to grow too much, making more mature blood cells. This is because of genetic changes, like the JAK2 V617F mutation.
This growth leads to more red blood cells, causing blood to be thicker. This can lead to blood clots, a big problem in PV. Knowing how this happens helps in finding new treatments.
Hypoxia-driven secondary polycythemia is when the body makes more red blood cells due to low oxygen. This is the body’s way to get more oxygen to tissues and organs. It helps them work right.
COPD is a lung disease that gets worse over time. It’s caused by smoking and other lung irritants. It makes it hard to breathe and lowers blood oxygen levels.
This low oxygen can make the body produce more red blood cells. People with COPD are at risk of getting secondary polycythemia.
Sleep apnea is a sleep disorder that causes breathing pauses. This can lead to nocturnal oxygen desaturation. Low oxygen levels during sleep can make the body produce more red blood cells.
This can lead to secondary polycythemia. Treating sleep apnea can help prevent this.
Congenital heart defects, like cyanotic heart disease, can’t oxygenate blood well. This causes chronic low blood oxygen. The body tries to fix this by making more red blood cells.
This can lead to secondary polycythemia.
Being at high altitudes means less oxygen in the air. The body tries to get more oxygen to tissues by making more red blood cells. This is a temporary fix.
But staying at high altitudes for a long time can cause lasting secondary polycythemia.
Kidney disorders are a big reason for secondary polycythemia. The kidneys help control red blood cell production by making erythropoietin. This hormone tells the bone marrow to make more red blood cells. But, some kidney problems can mess with this process, causing too many red blood cells.
Renal cell carcinoma is a kidney cancer that can make erythropoietin. This leads to too many red blood cells. When someone with this cancer has polycythemia, it shows the tumor is making erythropoietin on its own.
Polycystic kidney disease (PKD) is a genetic disorder with many cysts in the kidneys. It’s known for leading to kidney failure, but it can also cause polycythemia. The cysts might make erythropoietin or other things that help make red blood cells.
Renal artery stenosis is when the arteries to the kidneys get narrow. This causes less oxygen to the kidneys, which makes them make more erythropoietin. This increase in red blood cells can cause polycythemia.
Post-renal transplant erythrocytosis (PTE) happens when there are too many red blood cells after a kidney transplant. The reasons for PTE are complex. They include some drugs used after the transplant and kidney disease before the transplant.
Endocrine disorders and some medicines can change how our body makes red blood cells. This can lead to polycythemia, where we have too many red blood cells. This happens because of hormonal changes or the effects of certain drugs.
Androgens and anabolic steroids can make our body make more red blood cells. This can cause polycythemia. Research shows that people who use these substances to get better at sports or for health reasons are more likely to get polycythemia.
Erythropoietin (EPO) helps control how many red blood cells we make. It’s used to treat anemia in people with kidney disease. But, using EPO for sports can lead to too many red blood cells. This can improve sports performance but also risks our health.
“The use of erythropoietin-stimulating agents has been a contentious issue in professional sports, with numerous cases of doping highlighted in recent years.”
— Sports Medicine Journal
Cushing’s syndrome, caused by too much cortisol, can affect how we make red blood cells. Corticosteroids, used in medicine, can also change red blood cell production. The impact of these conditions and treatments on polycythemia is complex and needs careful management.
| Condition/Treatment | Effect on Erythropoiesis | Risk of Polycythemia |
| Androgen/Anabolic Steroid Use | Increased red blood cell production | High |
| Erythropoietin Therapy/Abuse | Enhanced erythropoiesis | High |
| Cushing’s Syndrome/Corticosteroids | Variable effects on red blood cell production | Moderate |
Other hormones can also affect how we make red blood cells. For example, thyroid problems and some pituitary gland issues can change red blood cell production. Understanding these hormonal effects is key to diagnosing and treating polycythemia well.
It’s important to know which conditions don’t cause polycythemia. Polycythemia is when you have too many red blood cells. But, some conditions don’t lead to this problem.
Normal pregnancy doesn’t usually cause polycythemia. Instead, it often leads to hemodilution. This means your blood gets more diluted because of extra plasma. This dilution stops any increase in red blood cells, making polycythemia unlikely.
Iron deficiency anemia doesn’t cause polycythemia. It actually hinders the production of red blood cells. Iron deficiency stops the body from making enough hemoglobin, leading to anemia, not polycythemia.
Some autoimmune diseases can slow down bone marrow. This means fewer red blood cells are made, not more. For example, systemic lupus erythematosus can slow down bone marrow, making polycythemia unlikely.
Liver cirrhosis, often with portal hypertension, doesn’t usually cause polycythemia. While cirrhosis can cause many blood problems, it doesn’t increase red blood cells. Instead, it can lead to variceal bleeding due to high blood pressure in the portal vein.
Here’s a list of conditions that don’t lead to polycythemia:
It’s important to tell true polycythemia apart from conditions that look like it. This is key for the right treatment. Several conditions can look like polycythemia, leading to wrong diagnoses if not correctly identified.
Dehydration can make it seem like there are more red blood cells. This is because there’s less plasma. It can trick lab tests into thinking there’s more red blood cells than there really is.
Key factors to consider:
Stress polycythemia, or Gaisböck Syndrome, is linked to high blood pressure and stress. It shows high hematocrit levels but doesn’t mean there’s more red blood cells.
Characteristics:
Lab mistakes can cause spurious polycythemia. These errors can happen during blood sampling or in lab measurements.
| Cause | Effect | Prevention |
| Improper venipuncture technique | Erroneous elevation of hematocrit | Proper training for phlebotomists |
| Laboratory measurement error | Inaccurate red blood cell count | Regular calibration and quality control |
Problems with plasma volume can also confuse polycythemia diagnosis. If plasma volume goes down, it can seem like there are more red blood cells.
To get a correct diagnosis, you need a full check-up. This includes lab tests and a doctor’s assessment. It’s the only way to tell true polycythemia from look-alike conditions.
Knowing the symptoms of polycythemia is key for early treatment. This condition, with too many red blood cells, can cause serious problems if not treated. It affects a person’s quality of life in many ways.
People with polycythemia might feel headaches, dizziness, and itchiness, often after warm baths. These issues come from blood being too thick, which reduces blood flow to organs. The body’s efforts to cope with too many red blood cells play a big role in these symptoms.
The high number of red blood cells in polycythemia makes blood too thick. This can lead to symptoms like decreased blood flow and oxygen to tissues. Hyperviscosity is a key feature of polycythemia, causing these symptoms.
Thrombotic complications are a big worry in polycythemia because of blood’s thickness. This can increase the chance of blood clots, like deep vein thrombosis or stroke. People with primary polycythemia are at even higher risk because of blood cell production issues.
| Symptom/Complication | Primary Polycythemia | Secondary Polycythemia |
| Thrombosis Risk | High | Variable |
| Hyperviscosity Symptoms | Common | Common |
| Headache and Dizziness | Frequent | Frequent |
Primary and secondary polycythemia show different symptoms. Primary polycythemia often leads to symptoms from blood thickness and clotting risks. Secondary polycythemia, caused by things like low oxygen, may show symptoms related to the cause.
For example, people with secondary polycythemia from COPD might also have breathing problems. These symptoms are in addition to those from the high red blood cell count.
If you have symptoms like severe headache, dizziness, or clot signs, see a doctor. Early treatment can greatly reduce risks of serious problems.
It’s important to know the symptoms and not delay seeing a doctor if you have them. This can lead to better health outcomes.
Identifying polycythemia accurately needs a detailed strategy. This condition, marked by more red blood cells, can be primary, secondary, or apparent. A multi-faceted approach is necessary for diagnosis.
Lab tests are the first step in diagnosing polycythemia. They check red blood cell count, hemoglobin, and hematocrit levels. A complete blood count (CBC) is key, giving a full view of blood cell counts.
Measuring erythropoietin levels helps tell if polycythemia is primary or secondary. Also, checking serum ferritin and vitamin B12 levels is important. These can affect how red blood cells are made. Testing kidney function is also essential, as kidneys help make erythropoietin.
After initial tests show polycythemia, more tests are needed to classify it. This includes molecular testing for genetic mutations, like the JAK2 V617F mutation. This is common in polycythemia vera. Other genetic tests may be needed for less common mutations.
Further tests check oxygen saturation levels and look for hypoxia or other causes of secondary polycythemia. Imaging, like ultrasound or CT scans, may look for causes like renal tumors.
Molecular and genetic tests are key in diagnosing and subclassifying polycythemia. Specific mutations, like JAK2 exon 12 mutations or MPL mutations, confirm polycythemia vera or other myeloproliferative neoplasms.
These tests help tell if polycythemia is primary or secondary. They guide treatment and assess the risk of blood clots.
A bone marrow biopsy and aspiration check the bone marrow’s cell count and shape. This is key in diagnosing polycythemia vera and other myeloproliferative neoplasms. It shows changes like hypercellularity and trilineage proliferation.
The bone marrow findings also help rule out other conditions that might look like polycythemia, like myelodysplastic syndromes.
Effective management of polycythemia requires evidence-based treatment strategies. The approach depends on whether it’s primary or secondary. It often combines medical treatments and lifestyle changes.
Primary polycythemia, or polycythemia vera (PV), is a disorder where too many red blood cells are made. Treatment aims to lower the risk of blood clots and ease symptoms.
Phlebotomy is key in treating PV. It helps reduce red blood cell count and keeps hematocrit levels in check. Regular phlebotomy lowers the risk of blood clots and improves health outcomes.
Secondary polycythemia is caused by factors like chronic low oxygen levels. Treatment aims to fix the root cause.
For secondary polycythemia caused by COPD or sleep apnea, oxygen therapy is used. It helps improve oxygen levels and lower erythropoietin production.
| Cause | Treatment Approach |
| COPD | Oxygen therapy, smoking cessation |
| Sleep Apnea | CPAP therapy, lifestyle modifications |
Lifestyle changes are vital in managing polycythemia. Patients should drink plenty of water, quit smoking, and keep a healthy weight.
Hydration is key. Dehydration can worsen blood thickening and increase blood clot risks.
Regular checks are essential for managing polycythemia. This includes blood tests, symptom checks, and adjusting treatments as needed.
Long-term follow-up helps catch complications early. It allows for timely adjustments in treatment plans.
Liv Hospital follows international standards and focuses on the patient. This ensures patients get the best care tailored to them.
Liv Hospital sticks to internationally recognized standards for diagnosing blood diseases like polycythemia. They use the latest diagnostic tools for accurate results.
The hospital’s treatment plans are patient-centered. They consider each patient’s unique situation. This ensures care is tailored for the best results.
Liv Hospital offers innovative therapies and joins clinical research. They test new treatments for polycythemia.
The care team at Liv Hospital is multidisciplinary. It includes experts in hematology, oncology, and internal medicine. They work together for complete care.
| Specialist | Role |
| Hematologist | Diagnosis and treatment of blood disorders |
| Oncologist | Management of possible cancers |
| Internal Medicine Specialist | Managing overall patient health |
Getting the right diagnosis and treatment for polycythemia is key to better health. We’ve looked at what polycythemia is, how it’s classified, and what causes it. We also talked about how it shows up in patients.
Liv Hospital takes a team approach to treating polycythemia. They make sure each patient gets care that fits their needs. This includes using the latest in blood disease diagnosis and treatments.
Understanding the causes of polycythemia is important for treatment. Doctors can then create plans that really help patients. This way, patients can get better faster.
To wrap it up, polycythemia is a serious condition that needs the right care. Thanks to Liv Hospital’s expertise, patients get top-notch treatment. This leads to better health for everyone.
Normal pregnancy is not a cause of polycythemia. In fact, pregnancy often dilutes the blood. This can hide polycythemia.
Polycythemia means too many red blood cells. Doctors check red blood cell mass, hemoglobin, and hematocrit levels to diagnose it.
There are primary, secondary, and apparent polycythemia. Primary polycythemia is often linked to polycythemia vera, caused by a JAK2 gene mutation.
Yes, some medications and endocrine disorders can cause polycythemia. This includes androgens, erythropoietin therapy, and Cushing’s syndrome.
Secondary polycythemia happens when the body doesn’t get enough oxygen. This can be due to COPD, sleep apnea, or heart defects.
Kidney issues like renal cell carcinoma, polycystic kidney disease, and post-renal transplant erythrocytosis can cause polycythemia.
Treatment for polycythemia includes managing the condition and making lifestyle changes. Liv Hospital follows international standards and focuses on patient care.
No, iron deficiency anemia actually hinders the production of red blood cells. It does not cause polycythemia.
Dehydration, stress polycythemia, and plasma volume changes can look like polycythemia. This makes diagnosis tricky.
If you have symptoms like blood clots, thick blood, or other signs of polycythemia, see a doctor.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!