Last Updated on November 20, 2025 by Ugurkan Demir

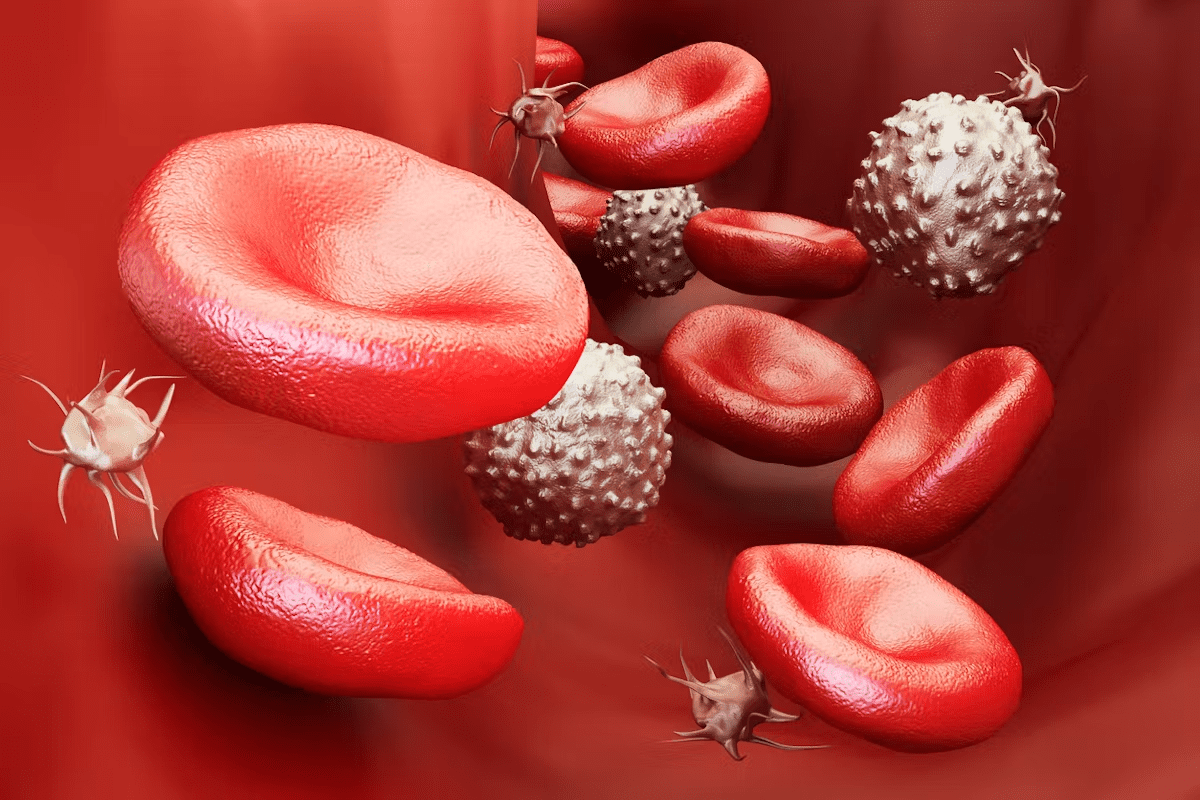
Polycythemia vera (PV) is a myeloproliferative neoplasm. It causes too many red blood cells, platelets, and neutrophils. Getting the diagnosis right is key to managing it well.
The JAK2 V617F mutation is found in about 97% of PV cases. This makes JAK2 testing very important for diagnosing PV. Understanding polycythemia diagnosis and the importance of JAK2 testing is vital for doctors.
Key Takeaways
- Polycythemia vera is a myeloproliferative neoplasm with excessive blood cell production.
- The JAK2 V617F mutation is a key diagnostic marker for PV.
- Accurate diagnosis is critical for effective management.
- JAK2 testing is essential in the diagnostic process.
- Understanding diagnostic criteria is vital for healthcare providers.
What is Polycythemia Vera: Definition and Clinical Significance
Polycythemia vera is a chronic disease where the body makes too many red blood cells. This leads to thicker blood and can cause serious health problems.
Polycythemia Vera Meaning and Classification
It falls under the category of myeloproliferative neoplasms (MPNs), which are diseases of abnormal blood cell growth. The World Health Organization (WHO) helps diagnose and classify these diseases, including polycythemia vera. This condition is often linked to a specific gene mutation, JAK2 V617F.
To classify polycythemia vera, doctors look at several key points:
- Elevated hemoglobin or hematocrit levels
- Presence of JAK2 mutations
- Bone marrow hypercellularity
- Subnormal serum erythropoietin levels
Epidemiology and Clinical Importance
It affects about 1-3 people per 100,000 each year. It’s more common in people over 60. The condition can lead to serious problems like blood clots, bleeding, and even cancer.
Polycythemia vera can greatly affect a person’s health. Without treatment, it can cause severe issues, including:
- Thrombotic events, such as stroke or myocardial infarction
- Hemorrhagic events due to abnormal platelet function
- Progression to myelofibrosis or acute myeloid leukemia
Knowing about polycythemia vera is key for early treatment. Doctors can then use specific treatments to help patients live better lives.
The Pathophysiology of Polycythemia Vera

To understand polycythemia vera, we must look at the genetic changes that cause it. This disorder makes too many red and white blood cells and platelets. It starts with a problem in the stem cells that grow into these blood cells.
Clonal Proliferation of Hematopoietic Stem Cells
At the heart of polycythemia vera is the growth of stem cells. These cells get a genetic change that helps them grow more than usual. The most common change is the JAK2 V617F mutation.
Key features of clonal proliferation in PV include:
- Autonomous growth of erythroid progenitors
- Hypersensitivity to growth factors
- Dysregulation of apoptosis
JAK-STAT Signaling Pathway Dysregulation
The JAK-STAT pathway is very important in polycythemia vera. The JAK2 V617F mutation keeps this pathway active all the time. This leads to too many cells being made and not dying when they should.
The dysregulation of the JAK-STAT pathway contributes to:
- Increased erythropoiesis
- Enhanced granulopoiesis and megakaryopoiesis
- Resistance to apoptosis
Resulting Hematological Abnormalities
The problems in stem cells and the JAK-STAT pathway cause specific blood issues in PV. These include too much hemoglobin, too many white and red blood cells, and too many platelets.
Knowing how PV works is key to diagnosing and treating it. The role of JAK2 mutations is very important in this process.
Etiology of Polycythemia Vera: Genetic Foundations
Polycythemia Vera’s cause is linked to genetic changes, mainly in somatic mutations. Knowing these genetic roots helps us understand the disease better. It also guides us in creating better treatments.
Acquired Somatic Mutations
Polycythemia Vera comes from mutations in blood-making cells. These changes cause too many red and white blood cells and platelets. The key mutation is in the JAK2 gene.
The Central Role of JAK2 Gene Mutations
The JAK2 V617F mutation is common in PV, found in about 97% of cases. It changes the JAK2 protein, making it always active. This leads to more cells and contributes to PV.
Other Contributing Genetic Factors
While JAK2 V617F is key, other genes play a role too. Mutations in MPL and CALR are found in cases without JAK2 mutations. This shows PV’s genetic complexity.
| Genetic Mutation | Frequency in PV | Impact on Disease |
| JAK2 V617F | Approximately 97% | Constitutive activation of JAK-STAT pathway |
| MPL Mutations | Rare | Activation of MPL signaling, contributing to PV pathogenesis |
| CALR Mutations | Rare | Impact on CALR function, associated with PV development |
Grasping Polycythemia Vera’s genetic roots is key for better diagnosis and treatment. The mix of genetic mutations makes the disease complex. We need a detailed approach to manage it well.
Comprehensive Polycythemia Diagnosis Approach
To diagnose polycythemia vera, doctors use a detailed approach. This includes clinical checks, lab tests, and genetic exams. This method is key to spot the condition and tell it apart from other blood disorders.
Clinical Presentation and Initial Evaluation
The first step is a careful clinical check. Patients might have symptoms like headaches, dizziness, and tiredness. Doctors look for signs like an enlarged spleen or blood clots.
Signs that need more looking into include:
- Elevated hemoglobin or hematocrit levels
- Splenomegaly
- Thrombosis or hemorrhage
- Symptoms of hyperviscosity syndrome
Laboratory Workup Strategy
Lab tests are vital for diagnosing polycythemia vera. The first tests are a complete blood count (CBC), erythropoietin level check, and JAK2 mutation test.
| Laboratory Test | Significance in Polycythemia Vera Diagnosis |
| Complete Blood Count (CBC) | Checks hemoglobin, hematocrit, and platelet count |
| Erythropoietin Level | Low levels help confirm polycythemia vera |
| JAK2 Mutation Testing | Finds JAK2 V617F or exon 12 mutations typical of polycythemia vera |
A leading hematologist says, “Diagnosing polycythemia vera focuses on JAK2 mutations and erythropoietin levels, along with clinical and lab findings.”
“It’s important to combine clinical signs, lab results, and genetic tests for a correct diagnosis.”
Importance of Systematic Diagnostic Assessment
A thorough diagnostic process is essential. It ensures all key criteria are checked. This helps differentiate polycythemia vera from similar conditions like secondary erythrocytosis.
The main criteria for diagnosing polycythemia vera include:
- Elevated hemoglobin or hematocrit
- JAK2 V617F or exon 12 mutation
- Bone marrow that’s too busy
- Low serum erythropoietin level
By carefully checking these criteria, doctors can accurately diagnose polycythemia vera. They can then plan the right treatment.
The 7 Key Diagnostic Criteria for Polycythemia Vera
Diagnosing polycythemia vera involves looking for specific signs that set it apart from other blood disorders. The criteria for diagnosing polycythemia vera include both clinical and lab findings.
Elevated Hemoglobin or Hematocrit Levels
Elevated hemoglobin or hematocrit levels are a key sign. This means there’s more red blood cells than usual. Doctors must consider the patient’s age, sex, and other factors to confirm this.
Bone Marrow Hypercellularity
Bone marrow hypercellularity is another important sign. Doctors check the bone marrow to see if it’s too full of cells. This is a sign of too many blood cells, which is common in polycythemia vera.
Presence of JAK2 V617F or Exon 12 Mutation
A JAK2 V617F or exon 12 mutation is a key marker for polycythemia vera. These mutations are found in most patients and help cause the disease. Testing for these mutations is key to confirming the diagnosis.
Subnormal Serum Erythropoietin Level
A subnormal serum erythropoietin level is also a key sign. Erythropoietin is a hormone that helps make red blood cells. Low levels of this hormone, along with high red blood cell counts, point to polycythemia vera.
Other factors like clinical presentation and laboratory findings are also important. Together, these help doctors accurately diagnose polycythemia vera and tell it apart from other conditions.
The 7 key diagnostic criteria for polycythemia vera are:
- Elevated hemoglobin or hematocrit levels
- Bone marrow hypercellularity
- Presence of JAK2 V617F or exon 12 mutation
- Subnormal serum erythropoietin level
- Other minor criteria that support the diagnosis
Understanding and using these criteria helps healthcare providers make accurate diagnoses and manage polycythemia vera effectively.
JAK2 Mutation Testing: The Cornerstone of PV Diagnosis
JAK2 testing is key in diagnosing polycythemia vera. Finding JAK2 mutations helps tell PV apart from other blood disorders.
JAK2 V617F Mutation: Present in Most Cases
The JAK2 V617F mutation is found in about 97% of PV cases. It’s a major marker for diagnosis. This mutation changes the JAK2 gene, turning on the JAK-STAT pathway.
This mutation’s common presence in PV patients makes it vital for diagnosis. It helps tell PV apart from other blood disorders.
JAK2 Exon 12 Mutations: Alternative Markers
In some PV patients without the JAK2 V617F mutation, JAK2 exon 12 mutations are found. These mutations also activate the JAK-STAT pathway. They are seen as alternative markers for PV.
- JAK2 exon 12 mutations are less common than V617F.
- They are typically found in patients with a clinical presentation suggestive of PV but who are V617F-negative.
Testing Methodologies and Interpretation
There are several ways to test for JAK2 mutations, including:
- Allele-specific PCR: A sensitive method for detecting the JAK2 V617F mutation.
- Sequencing: Useful for identifying JAK2 exon 12 mutations and other rare mutations.
- High-resolution melting analysis: A rapid screening method for detecting mutations.
Understanding JAK2 mutation testing results is complex. It needs a deep look at the clinical context and other criteria. A positive result for JAK2 V617F or exon 12 mutations supports PV diagnosis. A negative result might mean more tests are needed.
Peripheral Blood Analysis in Polycythemia Diagnosis
Peripheral blood analysis is a key tool in diagnosing polycythemia vera. It involves checking different parts of the blood to help diagnose the condition.
Complete Blood Count Patterns
A complete blood count (CBC) is a first step in diagnosing polycythemia vera. It shows important information about the blood. Key findings include:
- Elevated hemoglobin or hematocrit levels, showing more red blood cells.
- Leukocytosis, or more white blood cells.
- Thrombocytosis, or more platelets.
These signs are common in polycythemia vera. But, they can also show up in other blood disorders.
Peripheral Blood Smear Characteristics
Looking at the peripheral blood smear gives more clues. You might see:
- Red blood cell morphology: Different sizes and shapes.
- Nucleated red blood cells, showing bone marrow stress or problems.
- More granulocytes and their early forms.
The peripheral blood smear offers important clues. When combined with CBC results and other tests, it helps confirm polycythemia vera.
In summary, checking the blood is key in diagnosing polycythemia vera. By looking at CBC patterns and blood smear details, doctors can make a more accurate diagnosis.
Bone Marrow Examination in Polycythemia Vera
A bone marrow examination is key to diagnosing polycythemia vera. It shows the bone marrow’s cell structure and growth patterns. These details are important to confirm the disease.
Bone Marrow Biopsy Findings
Bone marrow biopsy is vital for diagnosing polycythemia vera. It looks at bone marrow tissue for cell count, shape, and other features. In polycythemia vera, the marrow is usually hypercellular with cells from three types: erythroid, granulocytic, and megakaryocytic.
Trilineage Proliferation Patterns
In polycythemia vera, cells from all three types grow more. This leads to more blood cells being made. It causes high hemoglobin or hematocrit levels in patients.
Histological and Immunohistochemical Features
The bone marrow biopsy in polycythemia vera shows special features. These include clustering of megakaryocytes and some fibrosis. Immunohistochemical staining helps identify cell types and growth levels. These signs help tell polycythemia vera apart from other diseases.
Combining bone marrow findings with other tests is key. This includes clinical signs, lab results, and genetic tests like JAK2 mutation analysis. Together, they help make a correct diagnosis of polycythemia vera.
Differential Diagnosis: Conditions Mimicking Polycythemia Vera
It’s important to tell Polycythemia Vera apart from other conditions. This is key for the right treatment. We need to find out which conditions look like Polycythemia Vera.
Secondary Erythrocytosis
Secondary erythrocytosis happens when there’s too many red blood cells for no reason in the bone marrow. It’s not like Polycythemia Vera. It doesn’t have the JAK2 V617F mutation in most cases.
Other Myeloproliferative Neoplasms
Other conditions like essential thrombocythemia and primary myelofibrosis can look like Polycythemia Vera. They all have JAK2 mutations. This makes it hard to tell them apart. We need to look closely at the symptoms and lab results.
Relative Polycythemia
Relative polycythemia, or Gaisbock syndrome, is when your hematocrit goes up but not your red blood cells. It’s often caused by dehydration or plasma volume contraction. It’s important to know the difference from Polycythemia Vera because the treatment is different.
To figure out if someone has Polycythemia Vera, we need to look at their history, physical check-up, lab tests, and check for JAK2 mutations. By doing this, doctors can give the right treatment to patients with Polycythemia Vera and similar conditions.
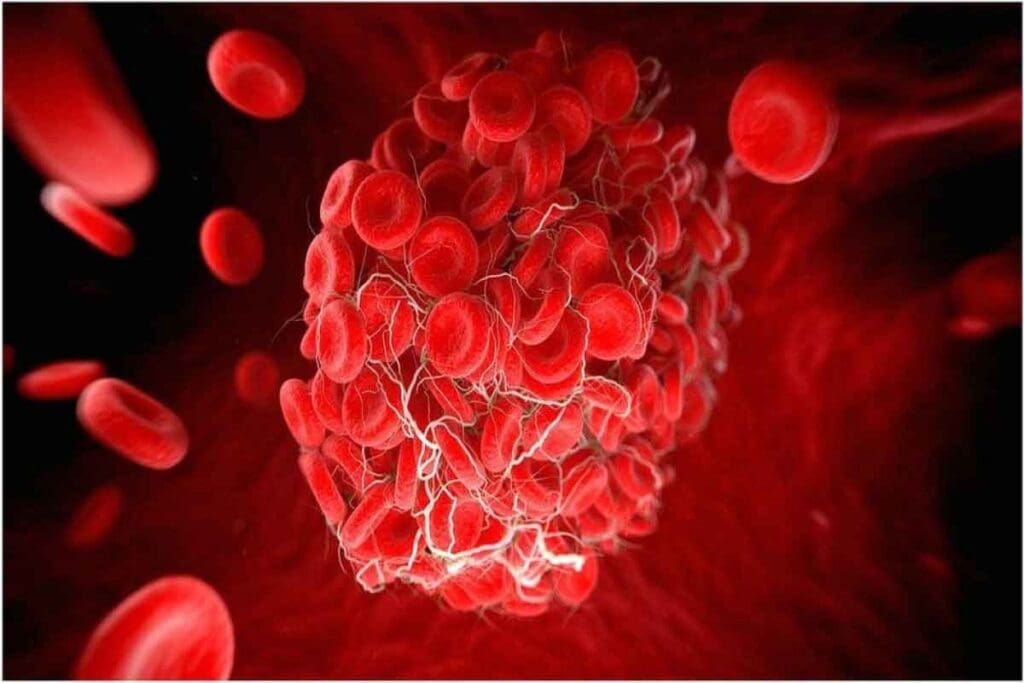
Complications and Risk Assessment in Polycythemia Vera
Polycythemia vera can lead to serious complications that affect a person’s life quality and survival. It’s important to understand these issues for effective management and risk assessment.
Thrombotic and Hemorrhagic Complications
Thrombotic and hemorrhagic complications are major risks with polycythemia vera. The blood’s increased viscosity due to more red blood cells can cause clots. This is a big reason for illness and death.
Thrombotic events can happen in arteries and veins, affecting the brain, heart, and legs. Hemorrhagic issues are less common but can happen, often due to bleeding disorders or treatments.
Disease Progression to Myelofibrosis or Leukemia
Polycythemia vera can turn into more serious diseases like myelofibrosis or leukemia. The chance of this happening depends on several factors, including genetic changes and how long the disease lasts.
| Risk Factor | Description | Impact on Disease Progression |
| JAK2 V617F mutation | A genetic mutation present in the majority of PV patients | Increases the risk of thrombotic events |
| Advanced age | Patients over 60 years old | Higher risk of disease progression and thrombotic events |
| History of thrombosis | Previous thrombotic events | Increased risk of future thrombotic events |
Risk-Adapted Management Approaches
Managing polycythemia vera depends on the patient’s risk level. Those at higher risk, like older patients or those with clot history, need stronger treatments. This includes medicines to reduce blood cell counts and blood thinners.
These tailored management plans aim to lower complication risks while keeping treatment side effects down. Regular check-ups and adjusting treatment plans are key to better patient outcomes.
Conclusion: Integrating Diagnostic Findings for Optimal Management
Effective polycythemia vera management starts with accurate diagnosis. Healthcare providers use this to create treatment plans. These plans help reduce symptoms and prevent serious health issues.
Diagnosis involves several tests. These include complete blood count, blood smear, and JAK2V617F assay. A bone marrow examination is also key. Knowing the patient’s genetic makeup, like JAK2 mutations, helps doctors understand the disease better.
Managing polycythemia vera well means using different treatments. These include phlebotomy, cytoreductive therapy, and drugs like ruxolitinib. Tailoring treatment to each patient improves their health and happiness.
FAQ
What is polycythemia vera?
Polycythemia vera is a rare blood disorder. It causes too many red and white blood cells and platelets. This happens because of a problem with blood cells’ growth.
What are the diagnostic criteria for polycythemia vera?
Doctors check for high blood counts and a busy bone marrow. They also look for specific gene mutations. These signs help confirm the diagnosis.
What is the role of JAK2 testing in diagnosing polycythemia vera?
JAK2 testing is key in diagnosing this condition. Almost all cases have the JAK2 V617F mutation. Some cases have JAK2 exon 12 mutations.
How is peripheral blood analysis used in diagnosing polycythemia vera?
Blood tests show high counts of red and white blood cells. A blood smear can also reveal signs of the disease.
What is the significance of bone marrow examination in polycythemia vera diagnosis?
A bone marrow test checks for too many cells and abnormal growth. It helps confirm the diagnosis.
What are the complications associated with polycythemia vera?
The disease can lead to blood clots and bleeding. It can also turn into more serious conditions like myelofibrosis or leukemia.
How is polycythemia vera differentiated from other myeloproliferative neoplasms?
It’s different from other blood disorders based on symptoms, lab results, and genetic tests. Each condition has unique signs.
What is the pathophysiology of polycythemia vera?
The disease starts with abnormal blood cell growth. This disrupts the JAK-STAT pathway, leading to too many cells.
What is the etiology of polycythemia vera?
It’s caused by genetic mutations, mainly in the JAK2 gene. Other genes can also play a role.
How is polycythemia vera managed?
Treatment depends on the patient’s risk level. It includes blood removal, medication, and supportive care. These steps help manage the disease.
References:
- Passamonti, F., Rumi, E., Pietra, D., Elena, C., Boveri, E., Cazzola, M. (2023). Polycythemia Vera. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK557660/