Last Updated on November 20, 2025 by Ugurkan Demir
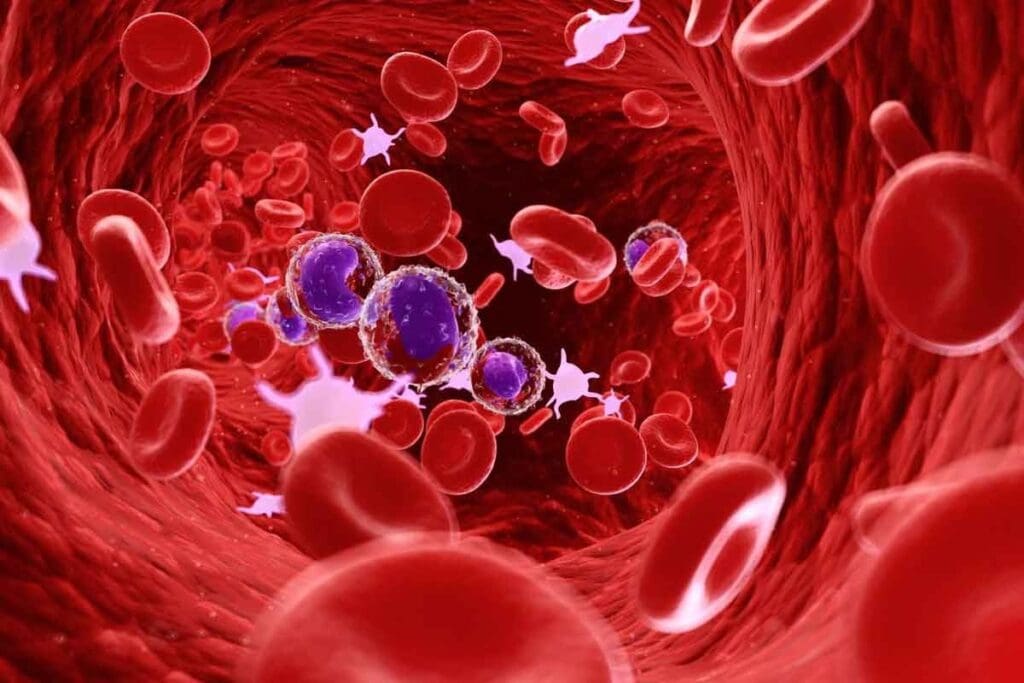
Feeling tired, dizzy, or short of breath might not just be stress. It could mean your body is making too many red blood cells. This is called secondary polycythemia. It’s different from primary polycythemia, which comes from a bone marrow issue. Secondary polycythemia is caused by outside factors.
At Liv Hospital, experts use top-notch tests to find what’s causing this condition. Knowing the symptoms and causes of secondary polycythemia is key to treating it well.
Spotting the signs and fixing the problems can really help patients. Liv Hospital focuses on the patient, aiming for the best care. They’re dedicated to helping those with this condition and raising awareness about secondary polycythemia symptoms.

Secondary polycythemia is a condition where the body makes too many red blood cells. This usually happens because of chronic hypoxia or other health problems. It’s different from primary polycythemia, also known as polycythemia vera, which is a disorder of the bone marrow.
Secondary polycythemia is when the body makes more red blood cells due to reasons outside the bone marrow. The hormone erythropoietin (EPO) plays a big role. It’s made when the body senses low oxygen levels, causing more red blood cells to be produced.
Several factors can lead to secondary polycythemia, including:
It’s important to know the difference between primary and secondary polycythemia for proper diagnosis and treatment. Primary polycythemia, or polycythemia vera, is a disorder where the bone marrow makes too many blood cells without an external reason. Secondary polycythemia, on the other hand, is a reaction to hypoxia or other factors, with increased EPO production.
The main differences are:
| Characteristics | Primary Polycythemia (Polycythemia Vera) | Secondary Polycythemia |
| Cause | Myeloproliferative disorder | External factors like chronic hypoxia, kidney tumors |
| EPO Level | Low | High |
| Bone Marrow | Overproduces blood cells | Normal response to increased EPO |

Erythropoietin, or EPO, is a hormone that helps make red blood cells. It’s important for keeping the right number of red blood cells in the body.
EPO is mainly made by the kidneys when blood oxygen levels are low. It goes to the bone marrow, making more red blood cells. This keeps the body’s oxygen supply steady.
The making of EPO is controlled by many factors. When there’s enough oxygen, EPO production goes down. This balance is key for healthy red blood cells.
In secondary polycythemia, EPO is not regulated right. This leads to too many red blood cells. Causes include chronic low oxygen, tumors, and genetic issues.
This can make blood thick, raising the chance of blood clots. Knowing how EPO works in secondary polycythemia helps find better treatments.
It’s important to know the symptoms of secondary polycythemia to manage it well. This condition makes your blood thicker, affecting your body in many ways.
Fatigue and weakness are common in people with secondary polycythemia. The thick blood makes it hard for oxygen to reach your body’s tissues.
Headaches and dizziness happen often too. The thick blood can’t flow well to your brain, causing these issues.
Some people see things differently, like blurred vision. This is because the thick blood affects the tiny blood vessels in your eyes.
Chest and abdominal pain can also occur. This is because the thick blood increases the chance of blood clots forming in your body.
Here’s a table with the 10 key warning signs of secondary polycythemia:
| Symptom | Description |
| Fatigue and Weakness | Impaired blood flow and oxygen delivery |
| Headaches and Dizziness | Reduced blood flow to the brain |
| Vision Changes | Effects on small vessels in the eyes |
| Chest and Abdominal Pain | Increased risk of thrombosis |
| Itching | Especially after hot showers, due to histamine release |
| Shortness of Breath | Impaired oxygen delivery |
| Numbness or Tingling | Reduced blood flow to extremities |
| Joint Pain | Increased uric acid levels |
| Splenomegaly | Enlargement of the spleen due to sequestration of red blood cells |
| Thrombosis | Increased risk of blood clot formation |
Knowing these symptoms is key to catching secondary polycythemia early. If you or someone you know has these signs, see a doctor right away.
Hypoxia, or chronic oxygen deprivation, is a key trigger for secondary polycythemia. When the body senses low oxygen, it starts a series of responses. These aim to boost oxygen to vital organs.
Chronic hypoxia happens when the body, or part of it, faces long-term low oxygen. This can come from high altitude, respiratory diseases, or heart issues that block oxygen.
The effects of chronic hypoxia are wide-ranging. They lead to more erythropoietin (EPO), a hormone that boosts red blood cell production.
When oxygen levels drop, the kidneys make more EPO. This hormone tells the bone marrow to make more red blood cells. This response helps tissues and organs get enough oxygen.
More red blood cells mean better oxygen delivery. But, this can cause secondary polycythemia, with too many red blood cells.
Respiratory diseases can cause chronic hypoxia, a key factor in secondary polycythemia. When the body senses low oxygen, it makes more erythropoietin (EPO). This leads to more red blood cells being produced.
COPD and emphysema are big causes of secondary polycythemia. These diseases hurt lung function, making it hard to get enough oxygen. So, the body makes more red blood cells to compensate.
COPD and Emphysema Effects:
Sleep apnea can also cause secondary polycythemia. It happens when breathing stops during sleep, leading to chronic hypoxia. This triggers more red blood cell production.
Sleep apnea consequences include:
Pulmonary fibrosis scars lung tissue, leading to poor gas exchange and chronic hypoxia. This scarring can cause EPO production and lead to secondary polycythemia.
| Respiratory Condition | Effect on Oxygen Levels | Consequence |
| COPD/Emphysema | Reduced lung function, chronic hypoxia | Secondary polycythemia |
| Sleep Apnea | Intermittent hypoxia | Increased red blood cell production |
| Pulmonary Fibrosis | Impaired gas exchange, chronic hypoxia | Secondary polycythemia |
In conclusion, many respiratory conditions can lead to secondary polycythemia by causing chronic hypoxia. It’s important to understand these conditions and their effects on the body to manage and treat secondary polycythemia.
Heart problems are a big reason for secondary polycythemia. When the heart can’t send enough oxygen, the body makes more red blood cells to help.
Congenital heart defects are heart problems that babies are born with. Some defects cause chronic hypoxia, leading to more red blood cells. Tetralogy of Fallot is one example where this happens.
Heart failure means the heart can’t pump enough blood. This reduces oxygen to tissues, causing the body to make more red blood cells. Heart failure is complex, but its effect on oxygen delivery can lead to secondary polycythemia.
Cyanotic Heart Disease
Cyanotic heart disease is a type of congenital defect that lowers blood oxygen. It makes the skin look blue and increases red blood cell production. The body tries to get more oxygen to tissues.
In summary, heart issues like congenital defects, heart failure, and cyanotic disease cause secondary polycythemia. Knowing these causes helps in treating the condition.
High altitude environments are tough on the human body. They trigger changes that can increase red blood cell counts. At elevations over 8,000 feet, the air has less oxygen. This makes the body work harder to get oxygen to tissues.
Going to high altitudes means the body gets less oxygen. To fix this, the kidneys make more erythropoietin (EPO). EPO tells the bone marrow to make more red blood cells. This helps keep vital organs oxygenated.
An expert in high-altitude medicine, says, “The increase in red blood cells is key. It lets the body survive in low-oxygen places.”
How well people adapt to high altitude varies. Some adjust fast, while others take longer or face more severe symptoms. Acclimatization is the body’s way of adjusting to less oxygen. It involves changes in breathing, red blood cell production, and more.
Staying at high altitudes for a long time can cause high altitude polycythemia or erythrocytosis. This is when there are too many red blood cells. It makes blood thicker and raises the risk of heart problems. Symptoms include headaches, dizziness, and tiredness.
“High altitude polycythemia is a big worry for people living high up. It can cause serious health issues if not handled right.”
To manage high altitude polycythemia, making lifestyle changes and getting medical help is key. People living high up should watch their health closely. Regular doctor visits can catch problems early.
Lifestyle choices like smoking and certain medications can increase the risk of secondary polycythemia. These factors can cause chronic hypoxia or disrupt normal body functions. This leads to more red blood cells being made.
Smoking is a major lifestyle factor that raises the risk of secondary polycythemia. Carbon monoxide exposure is a key part of smoking’s health risks. When people smoke, they breathe in carbon monoxide. This gas binds to hemoglobin, making it harder for blood to carry oxygen.
This creates a state of chronic hypoxia. It triggers the body to make more erythropoietin (EPO). This, in turn, increases the production of red blood cells.
Smoking’s impact on red blood cell production is significant. Studies show smokers are more likely to get secondary polycythemia because of carbon monoxide. The table below shows how smoking and carbon monoxide affect red blood cell production.
| Factor | Effect on Red Blood Cell Production | Mechanism |
| Smoking | Increased | Carbon monoxide reduces oxygen delivery |
| Carbon Monoxide Exposure | Increased | Binds to hemoglobin, reducing oxygen transport |
| Chronic Hypoxia | Increased | Triggers EPO production |
Using testosterone and anabolic steroids is another lifestyle factor that can lead to secondary polycythemia. These substances can boost erythropoiesis, causing more red blood cells to be made. A study in a well-respected medical journal found users of these substances are at higher risk of secondary polycythemia.
It’s important for those using testosterone or anabolic steroids to get regular checks for signs of secondary polycythemia. This includes looking at hematocrit levels. Healthcare providers need to know the risks and take steps to prevent them.
Secondary polycythemia can be caused by less common factors like renal and genetic conditions. These conditions affect how the body makes red blood cells.
Kidney tumors are a rare cause of secondary polycythemia. Some kidney tumors make erythropoietin (EPO), a hormone that boosts red blood cell production. Too much EPO can cause an increase in red blood cells, leading to polycythemia.
The most common kidney tumor linked to EPO production is renal cell carcinoma. Other tumors, like renal adenomas, can also increase EPO production.
| Type of Kidney Tumor | Association with EPO Production |
| Renal Cell Carcinoma | Strongly associated with EPO production |
| Renal Adenomas | Occasionally associated with EPO production |
| Other Renal Tumors | Rarely associated with EPO production |
Genetic disorders can mess up the body’s oxygen sensing, causing secondary polycythemia. These disorders often involve genes in the hypoxia-inducible factor (HIF) pathway.
One such disorder is Chuvash polycythemia. It’s a rare genetic condition caused by a VHL gene mutation. This mutation makes HIF active, leading to more EPO and polycythemia.
It’s important to know about these rare causes of secondary polycythemia. This knowledge helps doctors diagnose and treat the condition better.
To find out if someone has secondary polycythemia, doctors use several tools. These include complete blood counts and tests for erythropoietin levels. It’s important to use these tests to tell secondary polycythemia apart from other conditions.
A complete blood count (CBC) is often the first test for secondary polycythemia. It checks the levels of different blood cells. In secondary polycythemia, the CBC shows more red blood cells, hematocrit, and hemoglobin.
CBC Parameters in Secondary Polycythemia:
| Parameter | Typical Finding |
| Red Blood Cell Count | Elevated |
| Hematocrit | Elevated |
| Hemoglobin | Elevated |
Erythropoietin (EPO) level testing is key for diagnosing secondary polycythemia. EPO is a hormone that helps make red blood cells. In secondary polycythemia, EPO levels are high because of conditions like hypoxia or kidney disease.
Imaging like ultrasound or CT scans can help find the cause of secondary polycythemia. This could be kidney tumors or other issues causing low oxygen. Genetic tests might also be used to check for other polycythemia causes.
Diagnosing secondary polycythemia involves many steps. Doctors use lab tests, imaging, and clinical checks to find the root cause of high red blood cell counts.
Managing secondary polycythemia means understanding its causes and treating it. The goal is to ease symptoms, prevent problems, and improve life quality.
The first step is to find and fix the cause. This might mean treating chronic hypoxia or heart and lung issues. It could also mean stopping certain medicines that cause the problem. Fixing the cause helps lower red blood cell counts to normal.
Therapeutic phlebotomy is used when red blood cell levels are too high. It removes blood to lower red blood cell counts. This helps prevent blood clots but watch out for iron deficiency.
Some medicines can help by lowering red blood cell production or easing symptoms. For example, drugs that reduce erythropoietin levels can be helpful. Antiplatelet agents may also be used to prevent blood clots. The right medicine depends on the cause and the patient’s health.
Changing your lifestyle is key in managing secondary polycythemia. Quitting smoking helps because it reduces hypoxia. Eating right, exercising, and avoiding high places are also important. Drinking enough water helps prevent dehydration.
With a treatment plan that includes fixing causes, treatments, and lifestyle changes, people with secondary polycythemia can see big improvements. Their quality of life can greatly improve.
Living with secondary polycythemia means knowing a lot about it. It’s important to know it’s not cancer. This helps ease worries about it being linked to cancer.
The life expectancy for those with secondary polycythemia depends on the cause. Managing the cause well can help you live a normal life. This shows how key early diagnosis and treatment are.
To manage secondary polycythemia, you need to tackle the main issue. This could be a lung problem, heart issue, or something else. You might also need to do blood removal and make lifestyle changes. These steps help reduce symptoms and avoid serious problems.
Knowing about secondary polycythemia’s causes and signs helps you deal with it better. Working with your doctor, you can create a good treatment plan. This way, you can manage your condition and live better.
Secondary polycythemia is when your body makes too many red blood cells. This happens because of something outside your body, like not enough oxygen. It’s not because of a problem in your bone marrow.
It can be caused by not enough oxygen, breathing problems, heart diseases, or being at high altitudes. Smoking and using certain steroids can also cause it.
EPO is a hormone that helps make red blood cells. When there’s not enough oxygen, your body makes more EPO. This leads to making too many red blood cells.
You might feel tired, have headaches, or see things differently. You could also have pain in your chest or belly. These are signs of too many red blood cells.
No, it’s not cancer. It’s your body’s way of reacting to something else. Unlike primary polycythemia vera, which is a type of cancer.
Doctors check your blood and EPO levels. They might also use imaging or special tests to find out why it’s happening.
Treatment depends on the cause. It might include removing blood, taking medicine, or changing your lifestyle. This helps manage the condition.
Yes, managing the cause and getting proper treatment can help. People with secondary polycythemia can live active lives.
At high altitudes, your body makes more EPO to handle less oxygen. This can cause more red blood cells to be made, leading to high altitude polycythemia syndrome.
Life expectancy depends on the cause and how well it’s managed. With good treatment, outcomes can be much better.
Secondary polycythemia is a reaction to external factors. Polycythemia vera is a bone marrow disorder that causes too many red blood cells.
Yes, changing your lifestyle can help. Quitting smoking, avoiding certain steroids, and managing health issues can manage secondary polycythemia.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!