Inherited blood conditions affect millions worldwide, causing a big impact on health. These conditions are passed down through generations. They come from changes in genes that affect blood components, like red and white blood cells, platelets, and plasma. Explore 15 inherited blood diseases, including rare and common genetic conditions.
Liv Hospital is known for its high medical standards. It provides the latest info on hereditary blood disorders. Knowing about these genetic conditions is key to diagnosis and treatment. This article will look at 15 genetic blood disorders, explaining their causes and effects.
Key Takeaways
- Understanding genetic blood disorders is vital for effective diagnosis and treatment.
- Hereditary blood conditions result from genetic mutations affecting blood components.
- Liv Hospital offers up-to-date information on the latest research and treatments.
- A list of genetic blood disorders helps in identifying and managing these conditions.
- Genetic blood diseases have a significant impact on global health.
Understanding Inherited Blood Diseases and Their Impact
It’s important to know the genetic roots of inherited blood diseases to find good treatments. These conditions mess with the blood’s job. They come from genetic changes that can be passed down or happen on their own.
What Makes a Blood Disorder Genetic?
A blood disorder is genetic if it’s due to a gene mutation. These mutations mess with blood cell production or function. They can hit different parts of the blood, like red and white cells, and platelets.
Key genetic factors include:
- Mutations in genes coding for hemoglobin, leading to conditions like sickle cell disease and thalassemia.
- Deficiencies in clotting factors result in bleeding disorders such as hemophilia.
- Alterations in genes that regulate the production or function of blood cells.
How Blood Mutations Lead to Disease
Blood mutations can mess up blood cell function. For example, a mutation in the HBB gene causes sickle cell disease. In this disease, red blood cells get deformed and block blood vessels.
The ways these mutations cause disease are:
- Impaired production of essential proteins.
- Altered function of blood cells.
- Increased susceptibility to infections or bleeding.
Global Prevalence and Healthcare Burden
Inherited blood diseases are a big health problem worldwide. Sickle cell disease, for instance, affects millions, mostly in areas with lots of malaria.
These diseases put a big strain on healthcare. They need:
- Regular transfusions and monitoring.
- Specialized care to manage complications.
- Genetic counseling for families.
Some well-known hereditary blood diseases are sickle cell disease, beta thalassemia, and hemophilia. Sickle cell anemia is very common in many places. It’s key to manage these diseases well to better the lives of those affected.
Sickle Cell Disease: The Most Common Inherited Blood Disorder

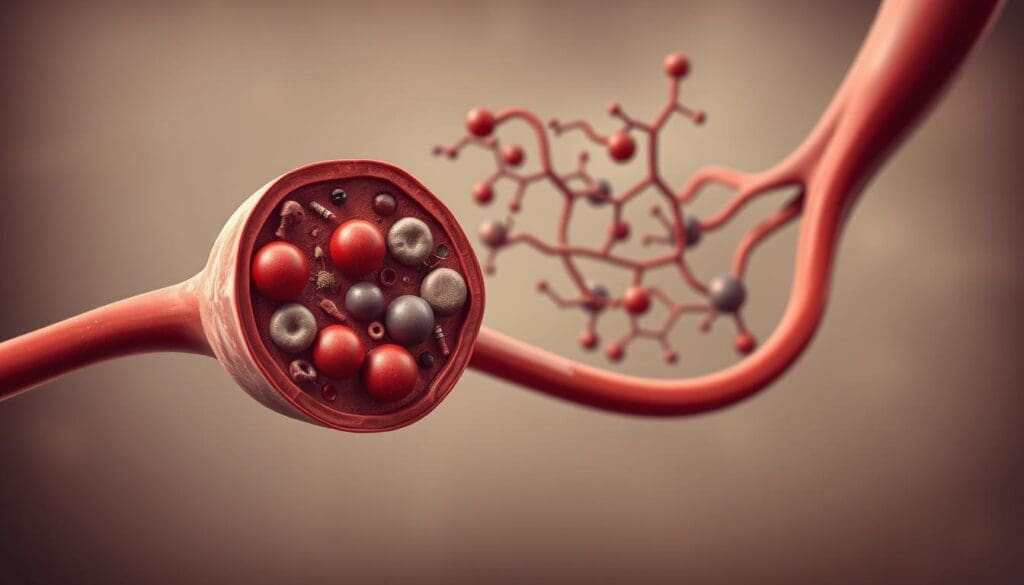
Sickle cell disease is a big health problem worldwide. It’s caused by a gene mutation that affects hemoglobin production. This leads to abnormal red blood cells that break down easily.
Pathophysiology and Genetics
The disease makes red blood cells sickle-shaped due to hemoglobin S. This happens when the blood is not fully oxygenated. Factors like dehydration and stress can trigger it. It’s inherited in an autosomal recessive pattern, meaning you need two mutated genes to have the disease.
Clinical Manifestations and Complications
Sickle cell disease shows up in many ways, like pain episodes and anemia. It also makes infections more likely. Serious problems can include chest syndrome, stroke, and organ damage.
How bad the disease is can differ a lot between people. Things like genetics, environment, and healthcare access affect it a lot.
Current Treatment Approaches
Today, treatments aim to manage symptoms and prevent problems. This includes pain relief, blood transfusions, and medicines like hydroxyurea. Gene therapy is also being explored to fix the genetic issue.
Supportive care, like vaccines and antibiotics, is also key. Research into new treatments, like gene editing, is promising for better management of sickle cell disease.
Thalassemia Syndromes: Alpha and Beta Variants
Thalassemia syndromes are inherited blood disorders. They affect how the body makes hemoglobin. This happens because of genetic changes in the genes for the alpha or beta globin chains of hemoglobin.
Alpha Thalassemia: From Silent Carrier to Hydrops Fetalis
Alpha thalassemia comes from changes or missing genes in the alpha globin genes. Its severity can range from no symptoms to severe Hydrops Fetalis, which is often fatal.
There are four main types of alpha thalassemia:
- Silent carrier state (one gene affected)
- Alpha thalassemia trait (two genes affected)
- Hemoglobin H disease (three genes affected)
- Hydrops Fetalis (all four genes affected)
Beta Thalassemia Major and Minor
Beta thalassemia is caused by changes in the beta globin genes. Beta thalassemia major, or Cooley’s anemia, is severe and needs lifelong transfusions. On the other hand, beta thalassemia minor is milder and often has few symptoms.
Managing beta thalassemia includes regular blood transfusions and iron chelation therapy. Bone marrow transplantation may also be an option in some cases.
Management and Transfusion Protocols
Managing thalassemia involves a detailed plan. This includes regular blood transfusions and monitoring for complications. It’s important to follow strict transfusion protocols to avoid iron overload.
Iron chelation therapy helps manage iron overload from frequent transfusions. Newer chelation therapies have greatly improved the lives of thalassemia patients.
Hemophilia A and B: X-Linked Bleeding Disorders
Hemophilia is a condition where blood can’t clot properly. It’s mainly split into two types: A and B. This split is based on which clotting factor is missing or not working well.
Factor VIII vs. Factor IX Deficiency
Hemophilia A happens when there’s not enough Factor VIII. Hemophilia B is caused by a lack of Factor IX. Both are key for blood to clot, and without them, bleeding lasts longer.
The main difference between Hemophilia A and B is not just the clotting factor. It’s also in their genetics and how they affect people.
Inheritance Patterns and Gender Differences
Hemophilia A and B are X-linked recessive disorders. This means the genes for these conditions are on the X chromosome. Because of this, males are more likely to have it than females, as males only have one X chromosome.
Females can carry the mutated gene. They’re less likely to show symptoms, but can pass it to their kids.
Prophylactic Treatment and Gene Therapy Advances
Prophylactic treatment involves regular infusions of the missing clotting factor. This helps prevent bleeding. It has greatly improved life for those with hemophilia.
Gene therapy is a new hope. It tries to fix the genetic problem causing hemophilia. Recent gene therapy trials show promise in cutting down bleeding and better managing the condition.
Key advancements in hemophilia treatment include:
- Recombinant clotting factor concentrates
- Extended half-life clotting factors
- Gene therapy trials
These new treatments are changing how we manage hemophilia. They offer hope for better lives and outcomes.
Von Willebrand Disease: The Most Prevalent Clotting Disorder
Von Willebrand disease is a genetic condition that affects blood clotting. It happens when there’s a problem with the von Willebrand factor gene. This gene is important for platelet adhesion and protecting factor VIII.
Types 1, 2, and 3: Varying Severity Levels
Von Willebrand disease has three main types, each with its own severity. Type 1 is the mildest, with only a partial lack of von Willebrand factor. Type 2 has a quality issue with von Willebrand factor, split into subtypes. Type 3 is the most severe, with no von Willebrand factor at all, causing serious bleeding.
Diagnostic Challenges and Approaches
Diagnosing Von Willebrand disease can be tough. It needs careful lab tests and genetic analysis. Tests check von Willebrand factor antigen levels and factor VIII. Genetic testing helps find gene mutations, confirming the diagnosis.
Treatment Options and Lifestyle Management
Treatment for Von Willebrand disease varies based on the type and severity. Desmopressin is often used to boost von Willebrand factor and factor VIII. For severe cases, von Willebrand factor concentrates are used. It’s also important to avoid certain medications and make lifestyle changes.
Managing Von Willebrand disease requires a full plan. This includes medical treatment and lifestyle changes. The goal is to reduce bleeding risks and improve life quality.
Factor Deficiencies: Beyond Hemophilia
Hemophilia is well-known, but other factor deficiencies like Factor VII, XI, and XIII also pose health risks. These genetic disorders can cause mild to severe bleeding. They affect many people, leading to different symptoms.
Factor VII Deficiency
Factor VII deficiency is a rare disorder where Factor VII, a key protein, is lacking. It’s often linked to gene mutations. Symptoms range from mild to severe, including bleeding in joints and the gut.
To diagnose it, tests check Factor VII levels. Treatment may include replacing it with recombinant Factor VIIa for bleeding or surgery.
Factor XI Deficiency (Hemophilia C)
Factor XI deficiency, or Hemophilia C, is different from A and B hemophilia. It’s more common in people of Ashkenazi Jewish descent. It’s caused by F11 gene mutations, leading to low Factor XI levels.
Bleeding symptoms can vary and aren’t always linked to Factor XI levels. Treatment often involves plasma or Factor XI concentrates for surgery or severe bleeding.
Factor XIII Deficiency
Factor XIII deficiency is rare and affects clot stability. It’s caused by mutations in the F13A1 or F13B genes. This leads to prolonged bleeding.
It can cause bleeding in newborns, slow wound healing, and miscarriages in women. Diagnosis involves testing Factor XIII activity. Treatment includes Factor XIII concentrates to manage bleeding.
Inherited Disorders Affecting Red Blood Cell Structure
Genetic mutations can cause problems with red blood cells. These issues can lead to inherited disorders. These disorders can make life harder for those affected.
Red blood cells are keytor carrying oxygen. But they can be affected in many ways. This can cause conditions that are mild or very serious.
Hereditary Spherocytosis
Hereditary spherocytosis is a genetic disorder. It makes red blood cells shape differently, into spheres instead of the usual disk shape. This leads to early destruction of red blood cells, causing anemia.
The severity of hereditary spherocytosis can vary a lot. Some people have mild symptoms, while others need a lot of medical help.
Hereditary Elliptocytosis
Hereditary elliptocytosis is another disorder affecting red blood cell shape. The cells are more oval than the usual disk shape. This condition can cause a range of symptoms, from none at all to severe anemia.
The symptoms vary because of different genetic causes. This makes the condition unpredictable.
Glucose-6-Phosphate Dehydrogenase Deficiency
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is a common disorder. It affects the enzyme that protects red blood cells. People with this deficiency can have severe reactions to certain things.
Managing G6PD deficiency means avoiding triggers. Sometimes, medical treatment is needed during severe episodes.
Pyruvate Kinase Deficiency
Pyruvate kinase deficiency is a rare disorder. It affects the enzyme pyruvate kinase, which is important for energy in red blood cells. This deficiency causes anemia because red blood cells don’t last long.
Treatment depends on how severe the condition is. It might include blood transfusions and other support.
Inherited disorders affecting red blood cells show how complex genetics can be. Knowing about these conditions is key to helping those affected.
Rare Inherited Blood Diseases and Their Manifestations
Rare inherited blood diseases are hard to diagnose and treat because they show many different symptoms. These conditions are often caused by genes and can really affect a person’s life. Doctors need to understand these rare diseases to give the right care.
Diamond-Blackfan Anemia
Diamond-Blackfan Anemia (DBA) is a rare genetic disorder that stops the body from making enough red blood cells. It usually starts in infancy or early childhood. Key features include:
- Anemia
- Congenital anomalies
- Increased risk of certain malignancies
DBA treatment often includes corticosteroids and blood transfusions. Sometimes, bone marrow transplantation is an option.
Fanconi Anemia
Fanconi Anemia is a rare genetic disorder that makes it hard for the body to make blood cells, leading to bone marrow failure. It is characterized by:
- Congenital abnormalities
- Progressive bone marrow failure
- Increased susceptibility to cancer
Management strategies include supportive care with blood transfusions and antibiotics, as well as hematopoietic stem cell transplantation.
Gaucher Disease
Gaucher Disease is a lysosomal storage disorder caused by a lack of the enzyme glucocerebrosidase. This leads to cells storing too much glucocerebroside, mainly affecting the spleen, liver, and bone marrow. Symptoms include:
- Anemia
- Thrombocytopenia
- Bone pain and fractures
Treatment involves enzyme replacement therapy (ERT) to help manage symptoms and improve life quality.
Congenital Dyserythropoietic Anemia
Congenital Dyserythropoietic Anemia (CDA) is a group of rare inherited disorders that cause anemia and other problems. Clinical features may include:
- Anemia
- Jaundice
- Splenomegaly
Managing CDA focuses on treating anemia and reducing iron overload, often through blood transfusions and iron chelation therapy.
Rare inherited blood diseases, like those mentioned, need a detailed and team-based approach for management. Advances in genetic testing and treatments are helping improve lives for those with these conditions.
Thrombophilia: Genetic Blood Clotting Disorders
Thrombophilia is a group of genetic disorders that make people more likely to get blood clots. These disorders can greatly increase the chance of getting venous thromboembolism (VTE). VTE includes deep vein thrombosis (DVT) and pulmonary embolism (PE).
Factor V Leiden Mutation
The Factor V Leiden mutation is a common cause of inherited thrombophilia. It changes the factor V gene, making it hard for activated protein C (APC) to work. This disrupts the normal way blood clots are prevented, leading to more clots.
Prothrombin G20210A Mutation
The prothrombin G20210A mutation is another big cause of thrombophilia. It makes more prothrombin, a clotting factor, in the blood. People with this mutation are more likely to get VTE.
Protein C and S Deficiencies
Protein C and S deficiencies are linked to thrombophilia, too. These proteins help stop blood clots by controlling the coagulation process. Without enough, the risk of clots goes up.
Antithrombin Deficiency
Antithrombin is a key protein that stops many clotting enzymes. Not having enough antithrombin raises the risk of blood clots.
Knowing about these genetic factors is key to diagnosing and treating thrombophilia. A list of genetic clotting disorders includes:
- Factor V Leiden mutation
- Prothrombin G20210A mutation
- Protein C deficiency
- Protein S deficiency
- Antithrombin deficiency
Genetic tests can spot people at risk early. This lets doctors take steps to prevent blood clots.
White Blood Cell Genetic Disorders
Genetic mutations can harm white blood cells, leading to immunodeficiency disorders. These cells are key to our immune system, fighting infections and diseases. When they’re affected, serious health issues can arise.
Chronic Granulomatous Disease
Chronic granulomatous disease (CGD) is a genetic disorder that weakens the immune system. It makes it hard to fight off certain bacteria and fungi. CGD is caused by mutations in the genes that encode for the subunits of the enzyme NADPH oxidase. This enzyme is vital for making reactive oxygen species that kill pathogens.
Leukocyte Adhesion Deficiency
Leukocyte adhesion deficiency (LAD) is a genetic disorder that affects the immune system. It prevents leukocytes from sticking to the endothelium and moving to infection sites. This leads to frequent bacterial and fungal infections. The condition is often fatal if not treated promptly and effectively.
Chediak-Higashi Syndrome
Chediak-Higashi syndrome is a rare genetic disorder that impacts the immune system. It makes it hard for certain cells, including white blood cells, to fight infections. Symptoms include a reduced ability to fight off infections, albinism, and neurological disorders.
| Disorder | Primary Impact | Common Symptoms |
| Chronic Granulomatous Disease | Impaired ability to kill bacteria and fungi | Recurrent life-threatening infections |
| Leukocyte Adhesion Deficiency | Inability of leukocytes to adhere and migrate | Recurrent bacterial and fungal infections |
| Chediak-Higashi Syndrome | Impaired immune cell function | Recurrent infections, albinism, and neurological issues |
Diagnosis and Management of Genetic Blood Disorders
Genetic blood disorders need accurate diagnosis and specific treatment plans. Early detection and proper care are key to better outcomes.
Genetic Testing and Counseling
Genetic testing and counseling are vital for managing genetic blood disorders. Genetic testing finds the exact mutation causing the disorder. This allows for focused treatments. Genetic counseling gives patients and families info on the disorder’s inheritance, risks, and treatment options.
| Genetic Test | Purpose | Benefits |
| Mutation Analysis | Identify specific genetic mutations | Targeted treatment, risk assessment |
| Carrier Testing | Determine carrier status | Family planning, risk reduction |
| Prenatal Testing | Diagnose genetic disorders in fetuses | Early intervention, informed decision-making |
Prenatal and Newborn Screening
Prenatal and newborn screening are key to early genetic disorders. Prenatal screening tests during pregnancy for genetic issues. Newborn screening tests are performed after birth to find disorders not seen clinically.
Emerging Therapies: Gene Therapy and CRISPR
Gene therapy and CRISPR are big steps forward in treating genetic blood disorders. Gene therapy fixes or replaces the faulty gene. CRISPR/Cas9 edits genes precisely, potentially fixing mutations at their source.
- Gene therapy could cure some genetic blood disorders.
- CRISPR/Cas9 edits genes with great precision.
- These new treatments are being studied and tested.
Multidisciplinary Care Approaches
Managing genetic blood disorders needs a team effort. Hematologists, geneticists, nurses, and others work together. This team approach ensures patients get the best care, improving their quality.
By combining genetic testing, counseling, and new treatments in a team care plan, doctors can greatly improve the diagnosis and treatment of genetic blood disorders.
Conclusion: Living with Inherited Blood Disorders
Living with inherited blood disorders needs a lot of care and support. Thanks to medical progress and genetic research, people with these conditions have better lives. Places like Liv Hospital lead in using the newest treatments, giving patients hope.
Genetic blood disorders, like sickle cell disease and thalassemia, need a team effort to manage. This includes genetic tests, prenatal screenings, and new treatments like gene therapy. Knowing the genetic cause helps doctors give better treatments.
People with inherited blood disorders need special care. This care includes treating the disorder and managing related issues. As research gets better, the future looks brighter for those with genetic blood disorders.
FAQ
What are inherited blood diseases?
Inherited blood diseases are caused by genetic mutations. They affect blood cells or the clotting process. These disorders can be passed down from parents to children.
What is the most common inherited blood disorder?
Sickle cell disease is a common inherited blood disorder. It affects millions of people worldwide.
What is thalassemia, and how is it managed?
Thalassemia is a genetic disorder that affects hemoglobin production. Management includes regular blood transfusions and iron chelation therapy. Sometimes, bone marrow transplantation is needed.
What is hemophilia, and how is it treated?
Hemophilia is a genetic disorder that affects blood clotting. It leads to excessive bleeding. Treatment involves clotting factor infusions and sometimes gene therapy.
What is von Willebrand disease?
Von Willebrand disease is a genetic disorder that affects blood clotting. It causes bleeding symptoms. It’s the most common inherited bleeding disorder.
What are the different types of genetic blood clotting disorders?
There are several genetic blood-clotting disorders. These include factor V Leiden mutation and prothrombin G20210A mutation. Also, protein C and S deficiencies, and antithrombin deficiency, among others.
How are genetic blood disorders diagnosed?
Genetic blood disorders are diagnosed through clinical evaluation and laboratory tests. Genetic testing, including prenatal and newborn screening, is also used.
What are the emerging therapies for genetic blood disorders?
New therapies include gene therapy and CRISPR gene editing. These aim to correct the genetic defect.
How can individuals with inherited blood disorders manage their condition?
Individuals can manage their condition through a multidisciplinary care approach. This includes regular medical check-ups and following treatment plans. Lifestyle modifications are also important.
What is the importance of genetic counseling for families affected by inherited blood disorders?
Genetic counseling is vital for families affected by inherited blood disorders. It provides information on risk, reproductive options, and condition management.
Are there any rare inherited blood diseases?
Yes, there are several rare inherited blood diseases. These include Diamond-Blackfan anemia and Fanconi anemia. Gaucher disease and congenital dyserythropoietic anemia are also rare.
How do genetic blood disorders affect white blood cells?
Genetic disorders can affect white blood cells. This leads to conditions like chronic granulomatous disease. It impairs the immune system’s function.
References
- Weatherall, D. J. (2025). Inherited disorders of hemoglobin – Disease control priorities. In GeneReviews®. University of Washington. https://www.ncbi.nlm.nih.gov/books/NBK11727/