Last Updated on November 20, 2025 by Ugurkan Demir

Acute Lymphocytic Leukemia (ALL) is a cancer that affects the blood and bone marrow. It is marked by the quick growth of immature white blood cells called lymphoblasts. At Liv Hospital, we know that ALL is a malignant disorder of lymphoid progenitor cells. This leads to the unchecked growth of these immature cells in the bone marrow. Discover acute lymphoblastic leukemia pathophysiology, causes, and how the disease affects blood and cells.
ALL is the most common cancer in kids and can also hit adults. The disease moves fast, making immature blood cells instead of mature ones. This can cause many health issues. Our team at Liv Hospital helps patients through diagnosis and treatment, giving them hope and full care.
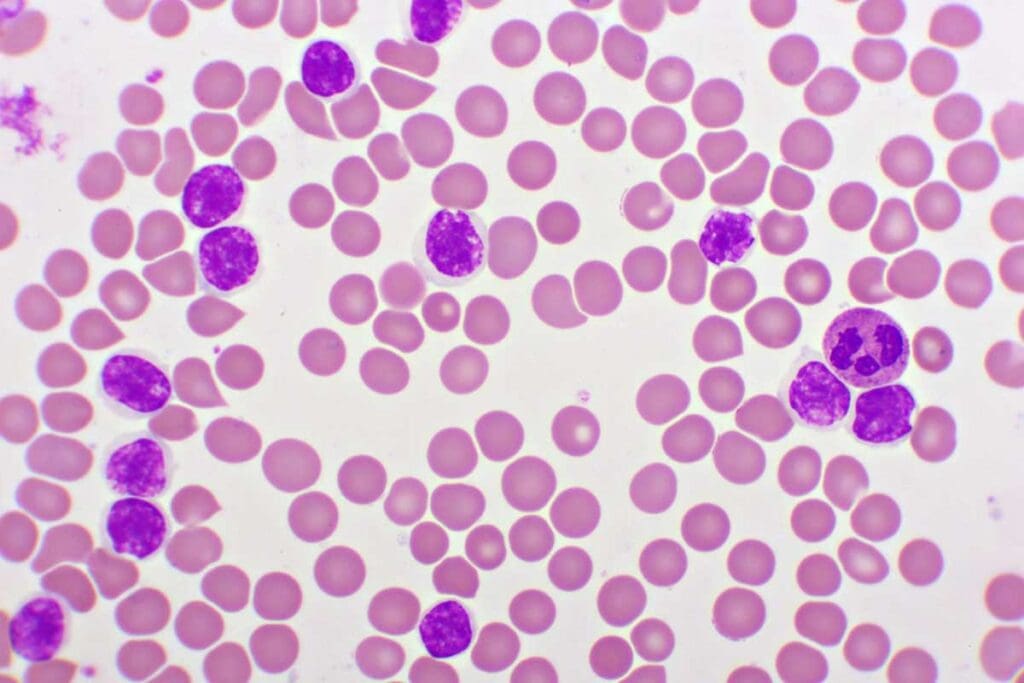
Acute Lymphocytic Leukemia (ALL) is a cancer that affects the blood and bone marrow. It’s caused by the fast growth of immature white blood cells, called lymphoblasts or leukemic blasts.
ALL is a cancer of the lymphoid lineage. It happens when lymphoblasts grow in the bone marrow, stopping normal blood cell production. There are different types of ALL, like B-cell and T-cell ALL.
The terms “Acute Lymphocytic Leukemia” and “Acute Lymphoblastic Leukemia” mean the same thing. The difference is mainly in how people in different places say it.
ALL is the most common cancer in kids, making up a big part of childhood cancers. Studies show it mostly affects children between 2 and 5 years old.
While ALL mostly affects kids, it can also happen in adults. Adults with ALL usually have a different treatment plan and outlook.
Long ago, ALL was thought to be a death sentence. But thanks to better medicine, like chemotherapy and care support, survival rates have greatly improved.
“The progress in treating ALL has been one of the most significant achievements in pediatric oncology, transforming a once-fatal disease into a highly curable condition for many patients.”
Source: A leading oncology journal
Our understanding of ALL has grown. We now know its genetic and molecular roots. This knowledge has led to new treatments that help patients live longer and better.
Understanding Acute Lymphoblastic Leukemia (ALL) is key to finding good treatments. The disease happens when lymphoid cells don’t grow right, causing the bone marrow to fail.
ALL starts with changes in lymphoid cells. These changes stop them from becoming real lymphocytes. Instead, they grow into lymphoblasts, which are not fully formed.
Leukemic cells take over the bone marrow. They push out the normal cells that make blood. This messes up blood production.
When the bone marrow is filled with leukemic cells, it can’t make enough blood. This leads to anemia, thrombocytopenia, and neutropenia. These problems make it hard to fight off infections and keep blood healthy.
| Hematological Parameter | Normal Condition | ALL Condition |
| Red Blood Cells | Normal count, functioning | Reduced count, anemia |
| Platelets | Normal count, functioning | Reduced count, thrombocytopenia |
| White Blood Cells | Normal count, functioning | Abnormal count, neutropenia |
As ALL gets worse, more leukemic cells build up. This makes treatment even more urgent and important.
ALL’s genetic roots lie in specific changes to chromosomes and genes. These changes mess up how cells work. They are key to understanding how ALL starts and grows.
Chromosomal translocations swap genetic material between chromosomes. This creates fusion genes that can cause leukemia. For example, the BCR-ABL1 fusion gene, from the t(9;22) translocation, is common in some ALL cases (PMCID: PMC5455679). These changes can mess up genes that control cell growth and death.
Key chromosomal translocations in ALL include:
Gene mutations are important in ALL’s development. They can mess with cell cycle, DNA repair, and cell death. For example, TP53 gene mutations can stop cells from dying, letting damaged cells live and get more mutations.
Common gene mutations in ALL involve:
Genetic factors are big in ALL, but environment also matters. Ionizing radiation, some chemicals, and past chemotherapy are risks. For example, kids who got certain chemo for cancer are more likely to get ALL later.
It’s important to know how genes and environment interact to fight ALL. We keep studying to find better ways to prevent and catch ALL early.
Understanding Acute Lymphocytic Leukemia (ALL) starts with its classification. This step helps doctors know how to treat it best. ALL is split into types based on the lymphocyte affected and the classification systems used.
B-cell ALL is the most common type. It happens when B-cell lymphoblasts grow too much in the bone marrow. B-cell ALL is then split into subgroups based on when the leukemia starts in B-cell development.
T-cell ALL is rarer but has its own signs, like big masses in the chest. It comes from T-cell lymphoblasts turning cancerous. Doctors spot T-cell ALL by looking for specific T-cell markers.
The World Health Organization (WHO) system is key for ALL classification. It looks at the leukemia’s genetics and molecules. The WHO classification helps figure out the risk and plan treatment.
The French-American-British (FAB) system is older but important. It classifies ALL by how cells look. Even though the WHO system is now used more, the FAB system helps us see how ALL classification has changed.
Knowing how to classify ALL is vital for doctors to treat it well. The different systems give important details about the disease. This helps doctors make better treatment plans and improve patient care.
Pediatric acute lymphocytic leukemia is the most common cancer in kids. It’s a big challenge in taking care of children. About 25 percent of childhood cancers are ALL, making it a big worry for doctors and families.
ALL in kids mostly happens between 2 and 5 years old. Boys get it a bit more than girls. It’s also more common in rich countries, which might mean it’s linked to the environment or genes.
Studies show ALL in kids is getting more common. This means we need to keep studying why and how to stop it.
Childhood ALL has special genetic traits that are different from adult ALL. Some genetic changes, like the Philadelphia chromosome, affect how well kids do.
Genetic tests help doctors figure out the best treatment for each child. This makes treatment more effective.
Kids with ALL might feel tired, have fevers, or bruise easily. They might also have bone pain, swollen lymph nodes, or big spleens.
It’s very important to catch ALL early. We need to watch for these signs and test kids quickly to start treatment right away.
How well a kid does with ALL depends on a few things. Age, how many white blood cells they have, and how they react to treatment are key.
Kids between 1 and 9 years old usually do better. Quick response to treatment is also a good sign. This shows how important good treatment is.
“The cure rates for childhood ALL have improved dramatically over the past few decades, thanks to advances in chemotherapy and supportive care.”
We’re working hard to understand and treat pediatric ALL better. Our goal is to make sure kids with this disease have a good life.
ALL is not just a disease of children; it also affects adults. There are big differences in how common it is, who gets it, and how well they do. Finding and treating adult ALL is a special challenge.
Adults get ALL much less often than kids. But, when they do, their treatment and chances of getting better can be different. This is because adults have unique factors that affect their disease.
In the U.S., about 1.7 people out of 100,000 get ALL each year. More men than women get it, and most are around 40 years old when they’re diagnosed.
| Age Group | Incidence Rate (per 100,000/year) |
| 20-39 years | 1.2 |
| 40-59 years | 1.7 |
| 60+ years | 2.3 |
Adult ALL has different genetic and molecular traits from childhood ALL. For example, adults are more likely to have the Philadelphia chromosome.
Key Pathophysiological Features in Adult ALL:
Adults with ALL usually have a worse outlook than kids. This is because adults often have more health problems, can’t handle treatments as well, and have more serious genetic issues.
Comparison of Prognostic Factors:
| Prognostic Factor | Childhood ALL | Adult ALL |
| Complete Remission Rate | 90-95% | 70-85% |
| 5-Year Survival Rate | 85-90% | 40-50% |
| Relapse Rate | 15-20% | 30-40% |
It’s important to understand these differences. This helps doctors create better treatment plans for adults with ALL.
To diagnose Acute Lymphocytic Leukemia, doctors use several tools. These include blood counts and bone marrow exams. These steps are key to finding ALL and knowing its details.
A complete blood count (CBC) is the first step in diagnosing ALL. It looks for signs like anemia, thrombocytopenia, or leukocytosis. These signs show if leukemia is present by checking the bone marrow.
| CBC Parameter | Normal Range | Typical Finding in ALL |
| Hemoglobin | 13.5-17.5 g/dL (male), 12-16 g/dL (female) | Decreased (anemia) |
| Platelet Count | 150,000-450,000/µL | Decreased (thrombocytopenia) |
| White Blood Cell Count | 4,500-11,000/µL | Variable (leukopenia or leukocytosis) |
A bone marrow exam is key to confirming ALL. It involves aspiration and biopsy to see how far the leukemia has spread. This helps figure out the leukemia’s type and how much it’s present.
Immunophenotyping is a vital tool for finding out the type of leukemia cells. It uses flow cytometry to see if the leukemia is B-cell or T-cell. This info is important for choosing the right treatment.
Cytogenetic and molecular tests give insights into the leukemia’s genes. Methods like karyotyping, FISH, and PCR help spot genetic changes. For more on these, check the National Center for Biotechnology Information.
Together, these methods help us accurately diagnose ALL. They let us know the type of leukemia and plan the best treatment.
At Liv Hospital, we use a variety of treatments for ALL. We tailor our approach to each patient’s needs. The treatment for Acute Lymphocytic Leukemia (ALL) includes different methods. These are chosen based on the patient’s risk factors and the disease’s characteristics.
Risk-adapted therapy is key in treating ALL. We look at several factors to decide on the treatment intensity. These include the patient’s age, white blood cell count at diagnosis, and genetic abnormalities.
Key factors influencing risk-adapted therapy include:
Chemotherapy is a mainstay in ALL treatment. We use different chemotherapy protocols. These protocols are divided into phases, such as induction, consolidation, and maintenance.
| Phase | Objective | Common Agents |
| Induction | Achieve remission | Vincristine, Prednisone, Anthracyclines |
| Consolidation | Eliminate residual leukemia cells | High-dose Methotrexate, Cytarabine |
| Maintenance | Prevent relapse | Mercaptopurine, Methotrexate |
Targeted therapies are a new and promising area in ALL treatment. These therapies target specific molecules in leukemia cells.
Monoclonal antibodies and tyrosine kinase inhibitors are examples. They have shown good results in some ALL patients.
Stem cell transplantation is considered for high-risk patients or those who have relapsed. This involves replacing the bone marrow with healthy stem cells. These can come from a donor or the patient themselves.
The decision to proceed with stem cell transplantation is based on:
We aim to provide complete care for ALL patients at Liv Hospital. We use a combination of treatments to help our international patients.
Recovering from Acute Lymphocytic Leukemia (ALL) means facing treatment-related issues and long-term effects. It’s important to know about these to give the best care.
ALL treatment can cause immediate problems. These affect different parts of the body. For example:
Managing these complications is key. It helps patients feel better and stick to their treatment plan. Growth factors can help lessen some of these side effects.
ALL survivors may deal with long-term effects that affect their quality of life. These include:
| Long-term Effect | Description |
| Cognitive Impairment | Difficulty with concentration and memory |
| Cardiac Issues | Increased risk of heart disease |
| Osteoporosis | Weakening of bones |
A study shows that childhood cancer survivors face long-term health problems. This highlights the need for ongoing care.
“The late effects of cancer treatment can be significant, and it’s vital that survivors receive follow-up care to manage these issues.”
Survivors’ quality of life is very important. It includes physical health, mental state, and social connections. It’s essential to provide comprehensive support services to help.
An oncologist once said, “Improving survivors’ quality of life needs a multi-faceted approach. It’s not just about physical health but also emotional and social needs.”
ALL survivors face a big risk of getting secondary malignancies. Risks include genetic factors, past radiation, and some chemotherapy.
By understanding these risks and taking action, we can better the long-term outcomes for ALL survivors.
Acute Lymphocytic Leukemia (ALL) is a complex disease that needs a detailed approach for diagnosis and treatment. Our overview shows how important it is to understand its causes, types, and how it affects different ages.
Early detection and tailored treatment are key to managing ALL. New treatments and therapies have greatly helped patients. We aim to give top-notch care to international patients, helping them get the best results.
It’s also important to manage complications and long-term effects to improve patients’ lives. By focusing on their physical, emotional, and mental health, we can greatly help them on their path to recovery.
Acute Lymphocytic Leukemia, also known as Acute Lymphoblastic Leukemia, is a blood and bone marrow cancer. It’s caused by the fast growth of immature white blood cells called lymphoblasts.
There are two main types of ALL. B-Cell Acute Lymphocytic Leukemia and T-Cell Acute Lymphocytic Leukemia. They differ based on the type of lymphoblasts present.
Doctors use a complete blood count and bone marrow examination to diagnose ALL. They also do immunophenotyping, cytogenetic, and molecular analysis. This helps confirm the disease and its subtype.
Treatment for ALL includes risk-adapted therapy and different chemotherapy protocols. Targeted therapies and stem cell transplantation are also options. The treatment plan is based on the patient’s risk factors and disease characteristics.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!