At Liv Hospital, we focus on top-notch healthcare. Understanding Acute Lymphocytic Leukemia (ALL) is key to treating it well. Learn acute lymphocytic leukemia pathophysiology, mechanisms, and how ALL impacts blood cell production.
ALL is a serious disease where immature cells grow too much in the bone marrow. It mostly hits kids. We look into the genetic changes, how it mess up blood-making, and the bone marrow failure it cause.
By understanding ALL, we give hope to families facing this tough diagnosis. Our care is both advanced and caring, focusing on each patient.
Key Takeaways
- ALL is a malignant disorder affecting immature lymphoid precursors in the bone marrow.
- Understanding the pathophysiology of ALL is key to effective treatment.
- Genetic mutations and disrupted hematopoiesis contribute to ALL.
- Liv Hospital prioritizes innovative and multidisciplinary care.
- Our approach combines cutting-edge science with patient-centered care.
Overview of Acute Lymphocytic Leukemia
Acute Lymphocytic Leukemia is a complex condition. It involves the overproduction of lymphoblasts in the bone marrow. This disrupts the normal production of blood cells, leading to health issues.
To understand ALL, we need to look at its definition, terminology, and epidemiology.
Definition and Terminology
Acute Lymphocytic Leukemia, also known as Acute Lymphoblastic Leukemia, is a type of cancer. It affects the blood and bone marrow. The term “acute” means it progresses quickly if not treated.
“Lymphocytic” refers to the type of cells affected, which are lymphocytes. These cells are important for the immune system. The disease is characterized by the rapid production of immature lymphocytes, known as lymphoblasts.
These lymphoblasts crowd out normal cells in the bone marrow. Understanding the terminology helps us understand the nature of ALL.
The disease is often associated with symptoms like fatigue, pale skin, and frequent infections. The rapid progression of ALL necessitates prompt diagnosis and treatment.
“Acute lymphoblastic leukemia (ALL) is a malignant disorder of lymphoid progenitor cells. It fails to produce normal hematopoiesis, leading to anemia, neutropenia, and thrombocytopenia.”
Epidemiology and Incidence Rates
ALL is the most common type of cancer in children, making up about 25% of all childhood cancers in the United States. The incidence of ALL is highest among children aged 1-4 years. While it’s predominantly a childhood disease, ALL can also occur in adults, though with less frequency.
| Age Group | Incidence Rate of ALL per 100,000 |
| <1 year | 24.1 |
| 1-4 years | 83.8 |
| 5-9 years | 43.1 |
| 10-14 years | 24.9 |
| 15-19 years | 13.4 |
The incidence rates vary significantly across different age groups. The peak incidence is observed in early childhood. Understanding these patterns is key for diagnosis and research into the causes of ALL.
Normal Lymphocyte Development and Differentiation

Lymphocyte development is a complex process. It involves the maturation of B-cells and T-cells. These white blood cells are key to our immune system.
B-cell and T-cell Maturation Process
B-cells mature in the bone marrow, while T-cells develop in the thymus. Both places have specific steps for their growth. These steps include gene rearrangement and selection.
B-cell maturation creates a unique B-cell receptor. This is vital for B-cells to recognize specific antigens.
T-cell maturation in the thymus rearranges T-cell receptor genes. It also selects T-cells to ensure they are functional and self-tolerant.
Regulatory Mechanisms in Lymphopoiesis
Lymphopoiesis is tightly regulated. This includes transcriptional regulation, cytokine signaling, and interactions with the microenvironment.
This regulation is key for lymphocytes to develop correctly. It helps them respond well to antigens. Without it, we might face immunodeficiency or diseases like Acute Lymphocytic Leukemia.
| Characteristics | B-cell Maturation | T-cell Maturation |
| Location | Bone Marrow | Thymus |
| Gene Rearrangement | Immunoglobulin genes | T-cell receptor genes |
| Selection Process | Clonal deletion and receptor editing | Positive and negative selection |
In conclusion, lymphocyte development is complex and tightly regulated. Understanding these processes is key to grasping Acute Lymphocytic Leukemia.
Acute Lymphocytic Leukemia Pathophysiology
To understand ALL, we must look at how lymphoid cells turn cancerous. This change is key to the disease’s development.
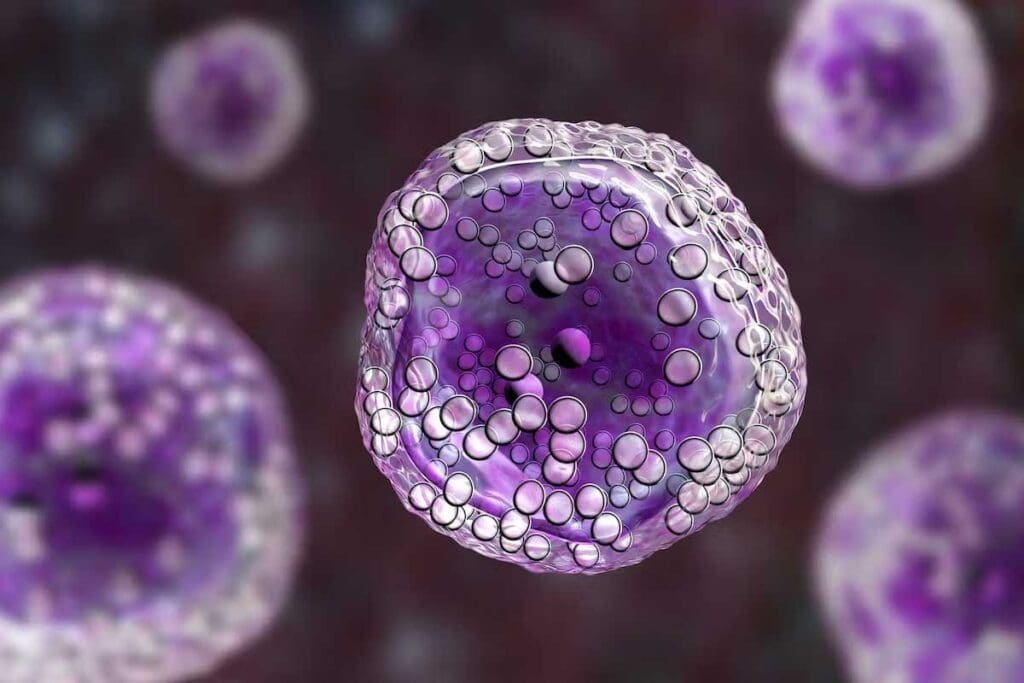
Malignant Transformation of Lymphoblasts
The change of lymphoblasts into cancer cells is vital in ALL. This change is often caused by genetic mutations. Genetic alterations can turn on cancer genes and turn off genes that fight cancer, leading to too many cells.
These genetic changes can happen for many reasons, like mistakes in DNA copying or exposure to harmful substances. The process involves both genetic and epigenetic factors, leading to cancer cells.
Clonal Expansion in Bone Marrow
After cells turn cancerous, they grow quickly in the bone marrow. This growth stops normal blood cell production. The bone marrow fills with cancer cells, disrupting blood cell creation.
The cancer cells grow because they can avoid dying and grow faster than normal cells. This leads to more cancer cells in the bone marrow, blood, and other parts of the body.
Disruption of Normal Hematopoiesis
ALL disrupts normal blood cell production. As cancer cells grow, they block the creation of healthy blood cells. This can cause anemia, low platelets, and low white blood cells.
This disruption causes symptoms like tiredness, infections, and bleeding. Knowing how it happens helps in finding better treatments.
Genetic Alterations in ALL
Understanding the genetic basis of Acute Lymphocytic Leukemia (ALL) is key for diagnosis and treatment. Genetic changes, like chromosomal translocations, are vital in ALL’s development and growth.
Chromosomal Translocations
Chromosomal translocations are a key feature of ALL. They create fusion genes that drive leukemia. The ETV6-RUNX1 fusion is common in pediatric ALL, found in about 25% of cases.
This fusion combines the ETV6 gene on chromosome 12 with the RUNX1 gene on chromosome 21. Another important translocation is BCR-ABL1, seen in some ALL patients, mostly adults. It’s more common in Chronic Myeloid Leukemia (CML).
The BCR-ABL1 fusion gene makes a tyrosine kinase that helps leukemia cells grow and live longer.
Other Recurrent Genetic Abnormalities
ALL also has other genetic changes that help it grow. These include mutations in genes for lymphocyte development, cell cycle, and DNA repair.
- Mutations in lymphocyte development genes: Like PAX5 and IKZF1, often seen in B-cell ALL.
- Cell cycle regulators: Changes in CDKN2A and CDKN2B lead to too much cell growth.
- DNA repair mechanisms: Problems in DNA repair can cause genetic instability, a hallmark of leukemia.
These genetic changes help start and grow ALL. They also affect how well the disease responds to treatment. Knowing a patient’s ALL genetics is vital for planning treatment.
Molecular Mechanisms of Leukemogenesis
The development of Acute Lymphocytic Leukemia (ALL) involves complex cellular processes. These processes are key to understanding how ALL starts and grows.
Dysregulation of Cell Cycle Control
One major factor in ALL is the disruption of cell cycle control. This control ensures cells grow, divide, and die properly. In ALL, genetic changes cause lymphoblasts to grow out of control. For example, changes in cyclin-dependent kinases (CDKs) and their inhibitors can lead to uncontrolled cell growthas seen in recent studies.
Cell cycle dysregulation often comes from mutations or changes in gene expression. This can cause an increase in lymphoblasts in the bone marrow, a hallmark of ALL.
Impaired Cellular Differentiation
ALL also involves a block in cellular differentiation. Normally, lymphoid progenitor cells turn into mature lymphocytes. But in ALL, this process stops, leading to more undifferentiated lymphoblasts.
The block in differentiation is often caused by genetic changes that affect important transcription factors. For example, some chromosomal translocations can create fusion genes that disrupt normal development.
Resistance to Apoptotic Signals
ALL cells are also resistant to apoptosis, or programmed cell death. Normally, damaged or unnecessary cells die. But in ALL, leukemic cells find ways to avoid dying, allowing them to keep growing.
Many genetic changes contribute to apoptotic resistance in ALL. For instance, mutations in genes like BCL2 help lymphoblasts live longer. Understanding these mechanisms is key to finding new treatments that can help cells die as they should.
By studying the molecular mechanisms of ALL, we can better understand its development. This knowledge helps us find new ways to treat the disease.
Consequences of Bone Marrow Failure
In ALL, bone marrow failure leads to severe issues. These include anemia, thrombocytopenia, and neutropenia. These problems happen because leukemic cells block normal blood cell production in the bone marrow.
Development of Anemia
Anemia is a big problem for ALL patients. It happens when the bone marrow can’t make enough red blood cells. This results in low hemoglobin levels. Symptoms of anemia include fatigue, weakness, and shortness of breath, making life harder for patients.
Thrombocytopenia and Hemorrhagic Complications
Thrombocytopenia, or low platelet count, is another issue in ALL. It raises the risk of hemorrhagic complications, from small bruises to serious bleeding. Patients might see petechiae, ecchymosis, or even bleeding in the brain.
Neutropenia and Susceptibility to Infections
Neutropenia makes patients very prone to infections. The risk of infection is significantly increased because their immune system is weak. This makes it hard for them to fight off infections. Common infections include bacterial sepsis, pneumonia, and fungal infections.
Managing these complications is key in treating ALL patients. Understanding bone marrow failure helps doctors create better treatment plans. This can improve patient outcomes.
Extramedullary Manifestations
Extramedullary manifestations of ALL are tough to diagnose and treat. These happen when leukemia cells spread to organs and tissues outside the bone marrow. This leads to various health problems.
Central Nervous System Involvement
One big problem with ALL is when leukemia cells get into the central nervous system (CNS). This can cause headaches, nausea, vomiting, and problems with nerves in the head. It’s a big worry because it needs special tests and treatments to reach the brain.
“The presence of CNS involvement at diagnosis is a poor prognostic factor, necessitating intensified treatment protocols.” Studies show that how common CNS involvement is can change treatment plans a lot.
Testicular Infiltration
Testicular infiltration is another issue in ALL, mainly in males. It makes the testicles swell without pain. Like the CNS, the testicles can be a safe place for leukemia cells, needing special care.
- Doctors can find testicular infiltration by feeling the testicles and using ultrasound or biopsy.
- It often shows up in cases where the leukemia has come back, so it’s important to keep a close eye on it.
Lymphadenopathy and Organomegaly
Lymphadenopathy and organomegaly are common in ALL. They happen when leukemia cells fill up lymph nodes and organs like the spleen and liver. This makes these areas grow bigger.
Lymphadenopathy can be uncomfortable and might be seen on physical exams or scans. Organomegaly can cause belly pain and affect how well a person feels.
“The presence of significant lymphadenopathy and organomegaly can complicate the clinical management of ALL, requiring a more detailed treatment plan.”
In summary, ALL’s extramedullary manifestations, like CNS involvement, testicular infiltration, and lymphadenopathy and organomegaly, are big challenges. Knowing about these helps doctors come up with better treatment plans and improve patient care.
Childhood vs. Adult ALL
ALL behaves differently in kids and adults, affecting how well they do and how they’re treated. Age is key in understanding the disease’s traits and how it responds to treatment.
Unique Features of Pediatric ALL
Pediatric ALL is the most common childhood cancer. It has special biological and clinical features. High hyperdiploidy or certain genetic translocations, like TEL-AML1, are common and linked to a good outlook.
Kids with ALL often show signs of bone marrow failure, like anemia and low blood counts. The disease can also spread to other areas, like the brain.
Age-Related Differences in Genetic Profiles
Genetics play a big role in ALL, and kids and adults have different patterns. Pediatric ALL often has genetic changes that affect lymphoid cell growth. Adult ALL, on the other hand, has more complex genetic issues, like the Philadelphia chromosome or MLL gene rearrangements.
These genetic differences affect how aggressive the disease is and how well it responds to treatment. For example, the Ph+ chromosome in adult ALL is a bad sign, but TKIs have helped some patients.
Prognostic Implications of Age
Age is a big factor in how well someone with ALL will do. Kids usually have a better chance than adults. This is because kids often have better genetics, can handle strong treatments better, and get tailored care.
Adult ALL, with its higher-risk genetics, faces more challenges. But, new ways to track MRD and new treatments are making a difference for adults too.
Etiology of Acute Lymphocytic Leukemia
ALL’s causes include environmental, genetic, and viral factors. Knowing these helps us find better ways to prevent and treat it.
Environmental Risk Factors
Some environmental factors raise the risk of getting ALL. Ionizing radiation is one, as seen in atomic bomb survivors and those who got radiation therapy.
Also, chemicals like benzene and organic solvents might increase the risk. But, more research is needed to confirm this.
Genetic Predisposition
Genetics are key in ALL’s causes. People with Down syndrome are at higher risk. Other genetic issues, like mutations in lymphocyte genes, also play a part.
“Genetic predisposition is a critical factor in the development of ALL, highlighting the need for genetic screening and counseling in high-risk populations.”
Viral Associations
Some viruses might lead to ALL, but how they do it isn’t clear. Human T-cell leukemia virus-1 (HTLV-1) causes adult T-cell leukemia/lymphoma. Its link to ALL is less known but shows viruses can play a role in lymphoid cancers.
Diagnostic Approaches and Classification
To accurately diagnose Acute Lymphocytic Leukemia, we use several methods. These include looking at the blood and bone marrow, doing tests like immunophenotyping, and analyzing chromosomes and genes. We also use systems to figure out the risk level of the disease.
Peripheral Blood and Bone Marrow Examination
The first step in diagnosing ALL is checking the blood and bone marrow. Peripheral blood examination can show signs like anemia and too few platelets. The bone marrow test is key to seeing how much cancer is there.
A study in the Journal of Clinical Oncology says, “bone marrow examination is the best way to diagnose ALL”.
“The presence of more than 20% lymphoblasts in the bone marrow is diagnostic of ALL.” – CCN Guidelines
Immunophenotyping
Immunophenotyping is a key tool for finding out what kind of cancer cells we’re dealing with. It uses flow cytometry to look at cell surface markers. Immunophenotyping helps tell if it’s B-cell or T-cell ALL, which affects treatment plans.
Cytogenetic and Molecular Analysis
Cytogenetic analysis looks at the chromosomes of cancer cells for genetic changes. Molecular analysis, like PCR and FISH, finds specific genetic mutations. These tests give us important information for treatment.
Risk Stratification Systems
Risk stratification is vital in managing ALL. It sorts patients into risk groups based on age, blood cell count, genetic changes, and how they respond to treatment. Risk stratification helps decide how intense the treatment should be and predicts how well the patient will do.
- Standard risk: Patients with good prognostic factors.
- High risk: Patients with bad prognostic factors.
By using these methods together, we can accurately diagnose and classify ALL. This lets us create treatment plans that fit each patient’s needs.
Advances in Understanding ALL Molecular Mechanisms
Research into Acute Lymphoblastic Leukemia (ALL) is making big strides. New methods like genomic profiling and epigenetic analysis are key. These advances let scientists dive deep into the genetic and molecular roots of ALL.
Genomic Profiling Technologies
Genomic profiling has changed the game in ALL research. It helps spot specific genetic changes that cause the disease. Next-generation sequencing (NGS) is a big part of this, finding mutations and chromosomal issues that were hard to see before.
A study in theNational Center for Biotechnology Information shows how much genomic profiling has helped us understand ALL.
Epigenetic Alterations
Epigenetic changes, like DNA methylation and histone modification, are vital in ALL. They can change how genes work without altering the DNA itself. This helps turn normal cells into cancer cells. Knowing about these changes has led to new treatments.
Microenvironment Interactions
The bone marrow microenvironment is key in ALL’s development. It helps leukemic cells grow and resist treatment. Studying these interactions could lead to new treatments that target the microenvironment.
Leukemic Stem Cell Concepts
Leukemic stem cells (LSCs) are a major focus in ALL research. They are believed to start and keep the disease going. Learning about LSCs, like how they self-renew and resist treatment, is essential for better treatments.
By understanding more about ALL’s molecular mechanisms, we can create better treatments. This will help improve how well patients do.
Conclusion
Understanding acute lymphocytic leukemia (ALL) is key to better treatments and outcomes. We’ve looked at how the disease works, including genetic changes and how it affects the body.
Diagnosing ALL involves several steps. These include blood and bone marrow tests, and looking at cells and genes. New technologies have helped us learn more about the disease.
This article aims to help healthcare workers and patients understand ALL. Managing ALL well needs a team effort. It requires the latest research and findings.
FAQ
What is Acute Lymphocytic Leukemia (ALL)?
Acute Lymphocytic Leukemia (ALL) is a blood cancer. It happens when immature lymphocytes grow too much in the bone marrow.
What are the different types of Acute Lymphocytic Leukemia?
ALL is mainly divided into B-cell ALL and T-cell ALL. These types are named after the lymphocytes they affect.
What is the pathophysiology of Acute Lymphocytic Leukemia?
ALL starts when lymphoblasts turn cancerous. They grow too much in the bone marrow. This disrupts normal blood cell production, causing bone marrow failure.
What are the genetic alterations associated with ALL?
ALL often has genetic changes like the ETV6-RUNX1 fusion. Other genetic problems also occur.
How is Acute Lymphocytic Leukemia diagnosed?
Doctors diagnose ALL by checking blood and bone marrow. They use tests like immunophenotyping and genetic analysis. They also sort patients into risk groups.
What are the consequences of bone marrow failure in ALL?
Bone marrow failure in ALL can cause anemia and low blood counts. This leads to tiredness, bleeding, and more infections.
What are the extramedullary manifestations of ALL?
ALL can affect areas outside the bone marrow. This includes the brain, testicles, and lymph nodes. It can also cause organs to grow bigger.
How does the etiology of ALL involve environmental risk factors?
Exposure to radiation and chemicals can increase the risk of ALL. These environmental factors play a role in its development.
What is the significance of age in Acute Lymphocytic Leukemia?
Age is a big factor in ALL. Kids usually do better than adults. This is because their bodies are more resilient.
What are the advances in understanding ALL molecular mechanisms?
New discoveries include using genetic profiling and studying epigenetics. Researchers also look at how the environment around cancer cells affects them.
What is the role of genetic predisposition in ALL?
Some people are more likely to get ALL because of their genes. This is due to inherited mutations.
Are there any viral associations with Acute Lymphocytic Leukemia?
Some viruses, like the human T-cell leukemia virus, might be linked to leukemia. But their exact role in ALL is being studied.
References
- National Cancer Institute. (2023). Acute lymphoblastic leukemia treatment (PDQ®)–patient version.
https://www.cancer.gov/types/leukemia/patient/all-treatment-pdq