Last Updated on November 26, 2025 by Bilal Hasdemir
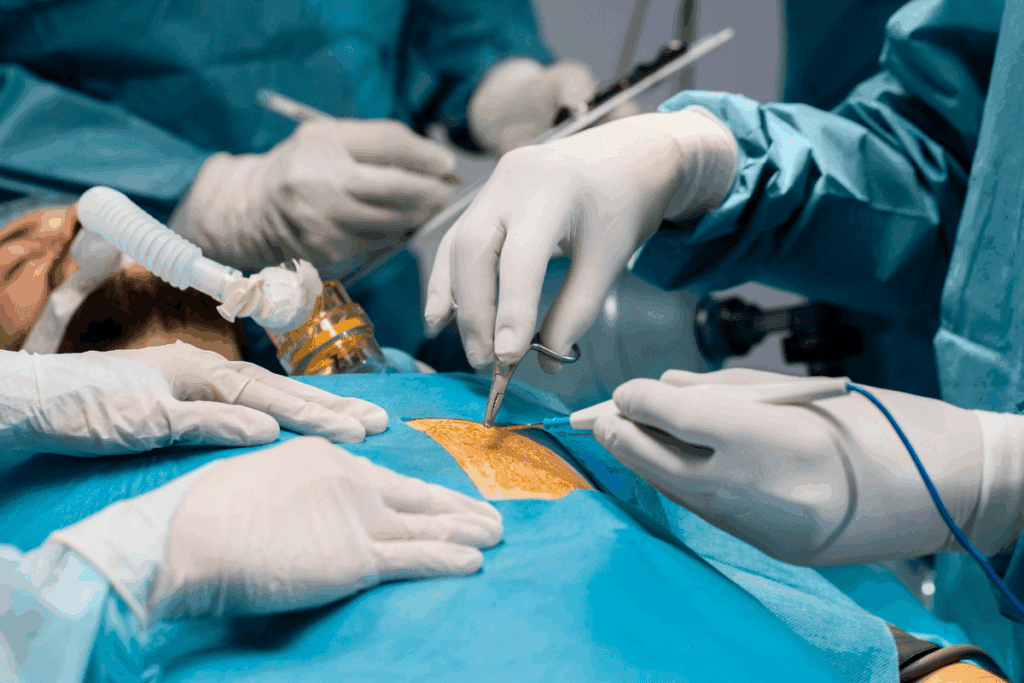
The ascending aorta is a key artery that starts from the heart. If it weakens or tears, it can be deadly. Cardiac aneurysm surgery, such as aortic repair surgery, is a safe way to fix problems like aortic aneurysms and dissections. At places like Liv Hospital, they focus on the patient and use the latest methods to treat them well.
Key Takeaways
- The ascending aortic repair is key for treating serious aortic issues.
- Open surgery is the main method, which involves replacing the bad part with a synthetic graft.
- Keeping the patient safe and precise is vital in aortic repair surgery.
- The surgery can be complex and needs a team effort.
- Using the latest techniques and caring for the patient is key for good results.
Understanding Ascending Aortic Pathology

It’s important to know about the ascending aorta’s structure to diagnose and treat problems. This part of the aorta starts at the heart’s left ventricle. It’s at risk for dilation and failure due to different issues.
Anatomy of the Ascending Aorta
The ascending aorta is about 5 cm long and is wrapped in the pericardium. It starts at the aortic valve and ends at the sternal angle, turning into the aortic arch. The anatomy of this section is critical because it has the aortic root, including the aortic valve and sinuses of Valsalva.
The normal diameter of the ascending aorta is under 4 cm. But, this can change with age, sex, and size. Understanding these variations is essential for spotting problems.
Common Pathologies Requiring Intervention
Two major issues with the ascending aorta are aneurysms and dissections. An aortic aneurysm is when the aorta gets bigger than 1.5 times its normal size. Aneurysms might not show symptoms and are often found by chance during imaging.
Aortic dissections happen when there’s a tear in the aorta’s intimal layer. This allows blood to flow between the aorta’s layers. It can lead to serious problems if not treated quickly.
Critical Measurements and Thresholds
Deciding to have surgery depends on the aneurysm’s size and symptoms. For the ascending aorta, surgery is usually needed when it’s over 5.5 cm. But, for people with Marfan syndrome, this size might be lower.
Regular monitoring is key for those with known aneurysms. This includes regular imaging to check the aneurysm’s size and growth. Early diagnosis and monitoring help prevent serious issues and figure out the best time for surgery.
Timing of Surgical Intervention

Deciding when to have surgery for the ascending aorta is very important. It depends on symptoms, aneurysm size, and the patient’s health. These factors help doctors choose the right time for surgery.
Emergency Indications
Emergency surgery is needed for acute aortic dissection or rupture. These are serious and need quick action. Symptoms like severe chest pain or signs of organ problems mean surgery is urgent.
- Acute aortic dissection
- Aortic rupture
- Signs of cardiac tamponade
- Organ malperfusion
Elective Surgery Criteria
For those without symptoms, surgery is planned based on aneurysm size and growth. Elective repair is usually done when the aneurysm is 5–5.5 cm in diameter. Fast growth or significant aortic regurgitation also lead to surgery.
Elective surgery criteria aim to balance risks. It’s about avoiding surgery’s dangers versus the risk of aneurysm rupture. Each patient’s risk factors and aneurysm details are carefully looked at.
- Aneurysm diameter ≥5–5.5 cm
- Rapid growth rate (>0.5 cm/year)
- Significant aortic regurgitation
Preoperative Assessment and Planning
A thorough preoperative evaluation is key for successful heart aneurysm surgery. It involves a detailed check to spot risks and plan the surgery well.
Clinical Evaluation
The first step is a detailed medical history and physical check. This is important to find any health issues that might affect the surgery. The doctor looks at the patient’s overall health to choose the best surgery plan.
Essential Imaging Studies
Imaging studies are vital for aorta aneurysm surgery planning. Computed Tomography (CT) scans show the aneurysm’s size and location. Echocardiograms check the heart’s function and valves. These help the surgeon plan the repair.
The right imaging depends on the patient’s anatomy and the suspected problem. CT scans are great for measuring the aorta and spotting complications.
Risk Stratification Tools
Risk stratification is a big part of preoperative planning. It helps predict complications and adjust the surgery plan. Many tools and systems are used to assess risk, considering age, health issues, and surgery complexity.
Using these tools, surgeons can make better decisions about aorta surgery. This improves patient results.
Surgical Team Preparation
Ascending aorta surgery is complex and needs a well-coordinated team. The success of the surgery depends on the team’s preparation and work together.
Team Composition and Roles
The team for repairing the ascending aorta includes cardiothoracic surgeons, anesthesiologists, perfusionists, and nurses. Each team member has a key role in the surgery.
- Cardiothoracic surgeons do the aorta repair.
- Anesthesiologists handle the patient’s anesthesia and watch over them.
- Perfusionists manage the heart-lung machine.
- Nurses help with patient care and surgical tools.
Equipment and Materials
The right tools and materials are vital for a good surgery. This includes:
- Surgical tools made for aortic surgery.
- A heart-lung machine.
- Equipment to monitor anesthesia and vital signs.
- Dacron grafts for the aorta replacement.
Preoperative Briefing Protocol
A preoperative briefing is key to make sure everyone knows the plan and possible issues. It should cover:
- Review of the patient’s medical history and scans.
- Talk about the surgery plan and possible problems.
- Check the needed equipment and materials.
- Each team member’s role and duties.
Good communication in the briefing is essential for a smooth and successful surgery.
Patient Preparation and Anesthesia
Anesthetic considerations are key for patients getting surgery on the ascending aorta. The aaa heart surgery is complex. It needs a detailed plan for anesthesia to keep the patient safe and help the surgery team work well.
Anesthetic Considerations
For heart aneurysm surgery, choosing the right anesthetic is very important. The anesthesiologist must watch the patient’s heart and breathing closely. They also need to be ready for any problems that might happen.
The type of anesthesia depends on the patient’s health before surgery and how big the aortic problem is. Doctors might use total intravenous anesthesia or a mix of inhalation and IV drugs, based on what the patient needs.
Advanced Monitoring Setup
For aorta aneurysm surgery, advanced monitoring is a must. It lets the anesthesiologist keep a close eye on the heart and make quick changes if needed. This includes checking blood pressure, central venous pressure, and using TEE to see how the heart is doing.
It’s also important to watch the brain’s oxygen and temperature, which is why tools like NIRS might be used. This is important if the patient will be under deep hypothermic circulatory arrest.
Positioning and Surgical Field Preparation
Getting the patient in the right position is important for surgery for heart aneurysm. They lie on their back with their arms by their sides. The area to be operated on is cleaned and covered to prevent infection.
The surgical team needs to have all the right tools ready and the operating room set up for a smooth surgery. A perfusionist is there to manage the heart-lung machine.
Establishing Cardiopulmonary Bypass
To fix the ascending aorta, setting up a good cardiopulmonary bypass is key. This method makes the surgery area bloodless. It also keeps the patient’s blood flowing while the repair is done.
Cannulation Techniques
Cannulation is a vital step in starting cardiopulmonary bypass. It involves putting cannulas in the aorta and right atrium. This redirects blood to the bypass machine. Careful placement of these cannulas is essential for good bypass and to avoid problems.
The spot for cannulation depends on the patient’s body and the aorta’s condition. Preoperative imaging helps plan the best cannulation strategy.
Initiation of Bypass
After cannulation, starting cardiopulmonary bypass is the next step. This means turning on the bypass machine and taking over the heart’s job. Monitoring the patient’s hemodynamics during this change is key to keeping them stable.
Starting the bypass needs teamwork between the surgical team and the perfusionist. They must manage flow, pressure, and blood gas levels well.
Temperature Management Strategies
Managing the patient’s temperature is important during cardiopulmonary bypass. The body’s temperature can be changed to help with the surgery. Hypothermia is often used to lower metabolic needs and protect organs during surgery.
There are different ways to manage temperature, like moderate hypothermia or deep hypothermic circulatory arrest. The choice depends on the surgery’s complexity and length.
Surgical Repair of Aorta: Standard Technique
The surgical repair of the ascending aorta is a critical procedure. It requires a deep understanding of the standard technique. This is key for treating aneurysms and dissections, which can harm patients if not treated quickly.
Median Sternotomy and Exposure
The first step is median sternotomy, which gives the best view of the ascending aorta. This method lets surgeons see the aorta and nearby structures clearly. It helps with the next steps of the surgery.
Median sternotomy involves a midline incision on the sternum. A sternal saw is used to divide the sternum. The pericardium is then opened, and stay sutures are placed. This provides great exposure of the ascending aorta.
Aortotomy and Diseased Segment Assessment
After exposure, the next step is aortotomy. This involves making an incision in the aorta to check the diseased segment. It’s a key step for evaluating the extent of the problem and planning the resection.
The aortotomy is done under cardiopulmonary bypass for a bloodless field. The incision is carefully planned to avoid damage and make repair easier.
Resection Technique
The resection of the diseased segment is a precise process. It’s done carefully to avoid complications. The diseased part is removed, trying to keep as much normal tissue as possible.
The technique used can vary based on the pathology. For example, in aortic aneurysms, the aneurysmal segment is removed. Then, the aorta is reconstructed with a Dacron graft.
Dacron Graft Selection and Sizing
Choosing and sizing the Dacron graft is very important. The graft must fit well to ensure a smooth anastomosis. This reduces the risk of complications like graft kinking or occlusion.
| Graft Size (mm) | Indication | Anastomotic Technique |
| 24-26 | Small aneurysms or normal aortic diameter | End-to-end anastomosis |
| 28-30 | Moderate-sized aneurysms | End-to-end anastomosis with reinforcement |
| 32 and above | Large aneurysms or extensive aortic disease | End-to-end anastomosis with additional grafting |
The graft size is based on the aorta’s diameter at the anastomosis. The anastomotic technique is chosen based on the case’s specific needs.
Valve-Sparing Aortic Root Replacement
The David procedure has changed how we treat aortic root aneurysms. It keeps the patient’s own aortic valve, which might cut down on the need for blood thinners. It also helps keep the valve working well.
David Procedure: Step-by-Step Approach
The David procedure starts with opening the chest through a median sternotomy. Then, the diseased aortic root is removed carefully, making sure the valve leaflets are saved.
The aortic valve is then put back into a Dacron graft. This graft replaces the old aortic root. The way the valve is reattached is very important to avoid problems.
Technical Considerations
Choosing the right Dacron graft is key in the David procedure. It must fit the patient’s body perfectly.
Also, attaching the coronary arteries to the graft is very important. It helps avoid blockages or narrowing of these arteries.
Valve Assessment and Repair Methods
Before surgery, the aortic valve is checked to see if it can be saved. A special ultrasound called transesophageal echocardiography (TEE) is used to check the valve’s function during surgery.
During the surgery, the surgeon looks at the valve for any damage. If needed, repairs are done to make sure the valve works right before it’s reattached.
Keeping the patient’s own valve helps in making the repair more natural. This could lead to better long-term results for the patient.
Blood Conservation Techniques
In aorta aneurysm surgery, using strong blood conservation methods is key. These methods aim to cut down blood loss and lessen the need for blood from others.
Cell Salvage Systems
Cell salvage systems are vital in blood conservation. They collect, process, and return a patient’s own blood lost during surgery. This method cuts down on the need for blood from others and lowers the risks of blood transfusions.
Benefits of Cell Salvage:
- Reduces need for blood from others
- Lowers risks of blood transfusion problems
- Saves the patient’s own blood
Antifibrinolytic Therapy
Antifibrinolytic agents, like tranexamic acid, are key in controlling bleeding during heart aneurysm surgery. They stop fibrinolysis, keeping clots stable and cutting down blood loss.
Tranexamic acid has been proven to greatly lower the need for blood transfusions in surgery.
Coagulation Management
Good coagulation management is essential in aaa heart surgery. It involves checking coagulation levels and using strategies to keep coagulation working well.
| Coagulation Parameter | Normal Value | Management Strategy |
| Prothrombin Time (PT) | 11-13.5 seconds | Give fresh frozen plasma if PT is too long |
| Activated Partial Thromboplastin Time (aPTT) | 25-35 seconds | Adjust heparin based on aPTT values |
| Fibrinogen Level | 200-400 mg/dL | Use cryoprecipitate or fibrinogen concentrate if low |
Transfusion Protocols
Transfusion protocols are key for guiding blood product use during and after heart aneurysm surgery. They help make smart choices about when to give red blood cells, plasma, and platelets.
By using these blood conservation methods, surgical teams can greatly improve patient results in aorta aneurysm surgery.
Brain Protection During Circulatory Arrest
Keeping the brain safe is key in aortic surgery, mainly when the heart stops. The complex repairs of the aorta, like the ascending aorta, need good ways to avoid brain damage.
Deep Hypothermic Circulatory Arrest
Deep hypothermic circulatory arrest (DHCA) is a common method for brain protection in aortic surgery. It cools the body to very low temperatures. This reduces the brain’s need for oxygen, protecting it during heart stoppage. Cooling to temperatures between 18°C to 22°C is common, making it safe for longer heart stops.
Using DHCA needs careful planning, including slow cooling and warming. This helps avoid brain and body problems.
Selective Cerebral Perfusion Methods
Selective cerebral perfusion (SCP) is another way to protect the brain during aortic surgery. It sends oxygen-rich blood directly to the brain’s blood vessels. This keeps the brain working during heart stoppage. SCP can be done through different ways of putting in the cannula, aiming at the brain’s arteries.
SCP lets for longer, safer heart stops. It can also be used with DHCA for better brain protection.
Monitoring Cerebral Oxygenation
It’s vital to watch the brain’s oxygen levels during heart stoppage to keep it safe. Tools like near-infrared spectroscopy (NIRS) give real-time brain oxygen levels. This helps the surgical team adjust their methods.
Pharmacological Neuroprotection
Pharmacological neuroprotection uses drugs to shield the brain from damage during heart stoppage. Drugs like corticosteroids, barbiturates, and anesthetics might help. They could lower the brain’s oxygen needs or fight off harmful substances.
Drugs play a supporting role to DHCA and SCP. They can help protect the brain more during complex aortic repairs.
Postoperative Management and Complications
After aorta aneurysm surgery, patients need careful management to avoid risks and ensure they recover well. Good postoperative care is key to preventing problems and getting the best results.
Immediate ICU Care Protocol
When patients arrive in the ICU, they are hooked up to advanced monitoring systems. Close monitoring helps catch any issues early, so they can be dealt with quickly.
The first steps in care include keeping oxygen levels right, managing pain well, and keeping the body at a normal temperature. These steps are important to reduce stress on the heart and help with recovery.
Hemodynamic Management
Managing blood flow is a big part of postoperative care after aorta aneurysm surgery. It’s about keeping blood pressure right, making sure vital organs get enough blood, and watching the heart’s output.
Doctors might use special medicines to help with blood pressure and heart function. Careful adjustment of these medicines is needed to avoid problems.
Common Complications
Even with modern surgery and care, problems can happen after heart aneurysm surgery. Issues like bleeding, heart rhythm problems, and breathing troubles are common.
- Bleeding: Needs quick action and might mean going back to surgery.
- Cardiac Arrhythmias: Treated with medicines or cardioversion.
- Respiratory Complications: May need long-term ventilation or other treatments.
Long-term Follow-up Imaging Schedule
Keeping an eye on the aorta over time is vital after aorta surgery. A plan for regular imaging, like CT or MRI scans, is important.
How often to do these scans depends on the patient’s risk factors and their surgery details. Usually, annual or biannual scans are suggested to watch the aorta and catch any problems early.
Conclusion
Surgical repair of the ascending aorta is a complex task. It needs a team effort to get the best results. A detailed care plan is key from start to finish.
The surgery involves advanced techniques like aorta repair and ascending aortic repair. These require great skill and precision. Each patient’s needs are unique, so the treatment must be customized.
Combining pre-surgery checks, surgery, and aftercare can greatly improve patient results. A team of experts, including surgeons and critical care specialists, is essential. Their collaboration is vital for a successful aortic repair.
FAQ
What is the purpose of surgical repair of the ascending aorta?
The main goal of fixing the ascending aorta is to treat serious problems like aneurysms and dissections. This is done by replacing the bad part with a man-made graft.
What are the common pathologies that require surgical intervention in the ascending aorta?
Problems like aortic aneurysms and dissections need surgery. These issues make the aorta weak.
What are the critical measurements that indicate the need for surgical intervention?
Important measurements are the size of the aneurysm and how fast it grows. Sizes over 5.5 cm often need surgery. Other factors can also raise the risk of rupture.
When is emergency surgical intervention required for ascending aortic pathology?
You need emergency surgery for acute dissections, ruptures, or other serious issues. These problems can make the aorta very weak.
What preoperative assessments are essential for planning surgical repair of the ascending aorta?
Before surgery, doctors do a full check-up and imaging tests like CT or MRI. They also use tools to figure out the best surgery plan.
What is the role of cardiopulmonary bypass in surgical repair of the ascending aorta?
Cardiopulmonary bypass is key for the surgery. It lets the heart and lungs rest while the aorta is fixed.
What is the David procedure in the context of valve-sparing aortic root replacement?
The David procedure is a way to fix the aortic valve without replacing it. It involves putting the valve in a graft to keep it working.
How is brain protection achieved during circulatory arrest?
To protect the brain, doctors use deep hypothermia and selective cerebral perfusion. They also watch the brain’s oxygen levels and use medicine to help protect it.
What are the key aspects of postoperative management following surgical repair of the ascending aorta?
After surgery, the main focus is on the ICU. Doctors manage blood pressure and watch for complications. They also plan for follow-up tests.
What blood conservation techniques are used during aortic surgery?
To save blood, doctors use cell salvage systems and antifibrinolytic therapy. They also manage coagulation and follow transfusion rules to reduce blood loss.
How is the surgical team prepared for ascending aortic repair?
The team gets ready with a detailed briefing. Everyone knows their role, the tools needed, and the surgery plan.
What is the significance of aneurysm size in determining the need for surgical repair?
Aneurysm size is very important. Sizes over 5.5 cm usually mean surgery is needed because of the high risk of rupture.
References
- Erbel, R., Aboyans, V., Boileau, C., Bossone, E., Di Bartolomeo, R., Eggebrecht, H., Evangelista, A., Falk, V., Frank, H., Gaemperli, I., Grabenwöger, J., Haude, M., Hasfuß, S., Kahlert, P., Kerner, J., Kotecha, D., Lancellotti, P., Leclercq, C., Limbourg, T., Manning, W., Nienaber, C. A., Ó Hartaigh, B., Pepi, M., Piazza, N., Piñeiro, R., Prati, F., Roffi, M., Rottbauer, W., Schfäers, H. J., Scheps, S., Taylor, K. C., Vahanian, A., & Windecker, S. (2014). 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). European Heart Journal, 35(41), 2873–2926. https://academic.oup.com/eurheartj/article/35/41/2873/452293






