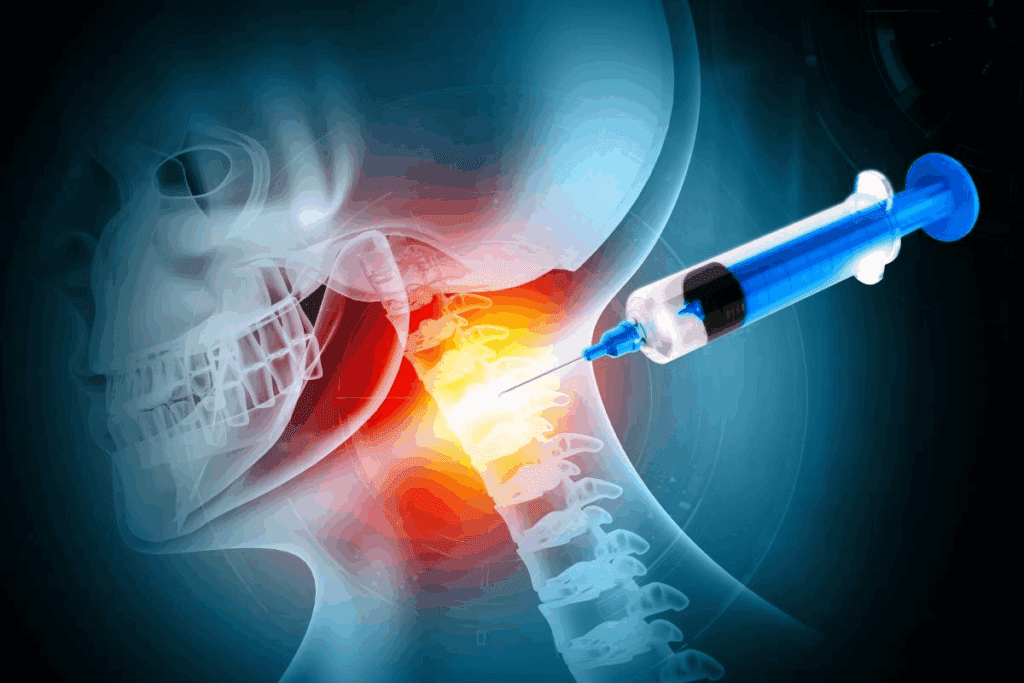
At Liv Hospital, we know how tough neck pain and radiculopathy can be. Cervical epidural steroid injections are a key treatment for these issues.
These injections are a minimally invasive procedure. They help reduce pain and swelling from nerve irritation. We target the affected area to help those with cervical radiculopathy and spondylosis.
In this article, we’ll cover seven important facts about cervical epidural steroid injections. We’ll guide you through the process and what you can expect.
Key Takeaways
- Understanding the role of cervical epidural steroid injections in pain management
- The importance of needle size in the procedure
- What to expect during the injection process
- Potential benefits and risks associated with the treatment
- How Liv Hospital’s expertise can support your care
What Are Cervical Epidural Steroid Injections?
Cervical epidural steroid injections put corticosteroids into the space around the spinal nerves in the neck. This method is used to treat chronic pain caused by nerve irritation and inflammation.
Definition and Purpose of the Procedure
This non-surgical treatment aims to reduce neck and arm pain. It delivers steroids directly to the affected area. This helps to target pain and inflammation.
It’s for those with chronic neck pain that hasn’t gotten better with other treatments. Injecting steroids into the epidural space helps reduce inflammation. This eases pain by calming irritated nerve roots.
Anatomical Overview of the Cervical Epidural Space
The cervical epidural space is around the dural sac, which holds the spinal cord and nerve roots. It’s between the dura mater and the spinal canal’s inner surface. This area is key for the procedure in the neck.
This space has fat, veins, and nerve roots. It’s perfect for steroid injections to lessen inflammation and nerve pressure.
Common Conditions Treated: Cervical Radiculopathy and Spondylosis
Cervical epidural steroid injections help with cervical radiculopathy and cervical spondylosis. Radiculopathy is when a nerve root in the neck gets inflamed or damaged. It causes pain, numbness, or weakness in the neck and arm.
Spondylosis is wear and tear on the neck’s joints and discs with age. It leads to neck pain and stiffness. Steroid injections in the epidural space manage this pain effectively.
The Growing Prevalence of Cervical ESI Treatments
Recent data shows a big jump in cervical epidural steroid injections (ESI) use in the U.S. This rise shows more people are turning to this treatment for neck pain and swelling.
There’s a big change in how we treat neck problems. More people are choosing cervical ESI. This is because studies prove it works well for neck pain and other issues.
Statistical Trends in the United States
Studies reveal a steady climb in cervical ESI use over the last ten years. A report in a top medical journal shows a big jump in these procedures. This shows doctors and patients are favoring this treatment.
This trend isn’t just for one group. It’s happening across different ages and places in the U.S.
| Year | Number of Cervical ESI Procedures (in thousands) | Percentage Change |
| 2010 | 150 | – |
| 2015 | 220 | +46.7% |
| 2020 | 300 | +36.4% |
Increasing Adoption Among Medicare Patients
More Medicare patients are getting cervical ESI. Studies show this number has more than doubled in ten years. This is a big deal.
“The increasing use of cervical epidural steroid injections among Medicare beneficiaries reflects a broader trend towards more conservative management of cervical spine disorders.”
A leading pain management specialist
This trend is important. It shows how pain management is changing, mainly for older adults.
Factors Driving the Rise in Cervical Injection Procedures
Several things are leading to more cervical ESI procedures. These include:
- More people are getting neck and spine disorders
- More people know and accept ESI as a treatment
- Better injection techniques and safety
- More demand for treatments that don’t involve surgery
Cervical Epidural Steroid Injection Needle Size Explained
The needle size for cervical epidural steroid injections varies. A specific range is commonly used. This range balances minimizing tissue trauma and ensuring precise placement.
Standard 22-25 Gauge Needles: Why This Range?
The standard needle size for cervical epidural steroid injections is 22-25 gauge. This range is chosen for a good balance. It’s thin enough to reduce tissue trauma but thick enough for precise control.
Key benefits of using 22-25 gauge needles include:
- Reduced risk of tissue damage
- Less patient discomfort
- Improved precision in steroid delivery
How Needle Size Affects Tissue Trauma and Precision
The needle size in cervical epidural steroid injections greatly affects tissue trauma and precision. A larger needle may cause more tissue trauma, leading to increased pain and complications. On the other hand, a smaller needle may be harder to control, affecting the accuracy of steroid delivery.
Studies have shown that the 22-25 gauge range is effective. It minimizes trauma while maintaining procedural accuracy.
Specialized Needles for Different Cervical Approaches
Different cervical epidural steroid injection techniques require specialized needles. For example, the transforaminal approach might use a smaller gauge needle for narrower pathways. The interlaminar approach might use a slightly larger gauge needle for direct access.
| Cervical Approach | Typical Needle Gauge | Key Considerations |
| Interlaminar | 22-23 gauge | Direct access, slightly larger gauge acceptable |
| Transforaminal | 24-25 gauge | Navigating narrower pathways, precision is critical |
Understanding needle size and its implications for different cervical epidural steroid injection techniques is key. Healthcare providers can improve patient care by optimizing their approach. This enhances both the safety and efficacy of the procedure.
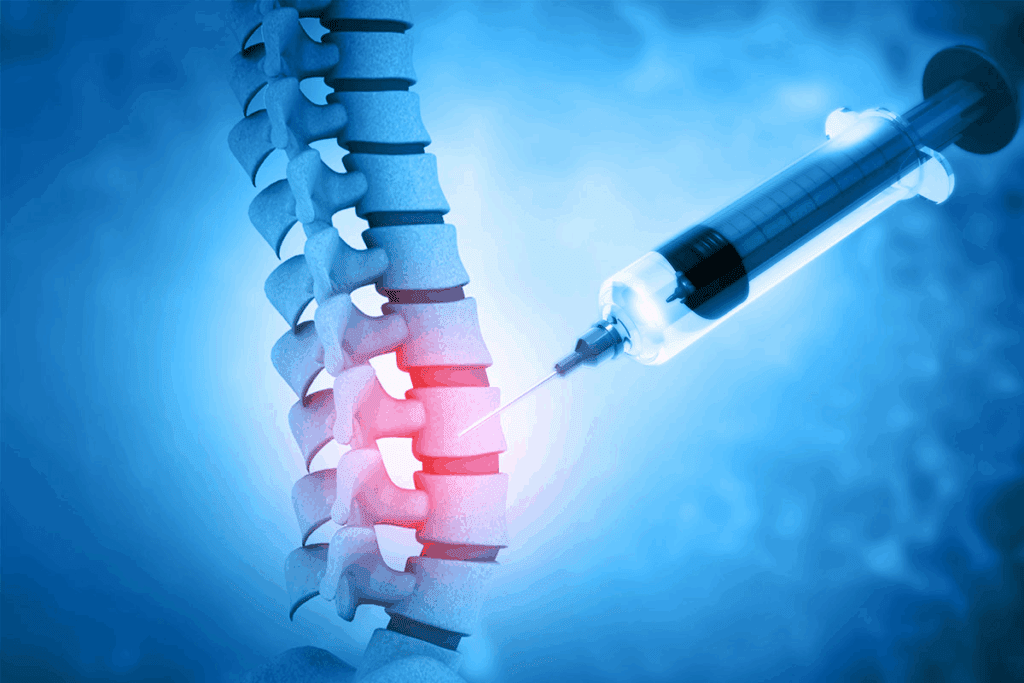
The Critical Role of Imaging in Cervical Epidural Procedures
Imaging is key to the success and safety of cervical epidural steroid injections. The complex anatomy of the cervical spine requires precise imaging. This ensures effective treatment and reduces risks.
Fluoroscopic Guidance Techniques
Fluoroscopic guidance is the standard for these injections. It provides real-time images for accurate needle placement. A contrast agent is used to confirm the needle’s correct position in the epidural space.
Key aspects of fluoroscopic guidance include:
- Real-time visualization of the needle trajectory
- Confirmation of correct needle placement using contrast agents
- Ability to adjust needle position during the procedure
Safety Advantages of Real-Time Imaging
Real-time imaging during injections greatly improves safety. It lets the practitioner see the needle in real-time. This reduces the risk of accidental injection into blood vessels or nerves.
The safety advantages include:
- Reduced risk of intravascular injection
- Minimized risk of nerve root injury
- Improved accuracy of steroid delivery
| Safety Feature | Benefit |
| Real-time visualization | Immediate detection of possible complications |
| Contrast agent use | Confirmation of correct needle placement |
| Adjustable needle positioning | Enhanced precision during the procedure |
Alternative Imaging Methods for Cervical Spine Injections
While fluoroscopy is common, other methods like CT guidance and ultrasound are used too. These alternatives are chosen based on the case’s complexity and the need for detailed images.
CT guidance provides high-resolution images. It’s useful for complex cases where detailed anatomy is needed.
A comparison of imaging modalities is provided below:
| Imaging Modality | Advantages | Limitations |
| Fluoroscopy | Real-time imaging, widely available | Radiation exposure, limited soft tissue detail |
| CT Guidance | High-resolution imaging, excellent for complex cases | Higher radiation dose, less real-time capability |
| Ultrasound | No radiation, real-time capability | Limited by operator skill, less effective for deep injections |
In conclusion, imaging is essential for the success and safety of cervical epidural steroid injections. The choice of imaging modality depends on the procedure, patient anatomy, and available resources.
Cervical Epidural Steroid Administration Techniques
The method used for cervical epidural steroid administration is key to treatment success. We use different techniques to place the steroid where it’s needed most. This helps reduce pain and swelling.
Interlaminar Approach: Procedure and Considerations
The interlaminar approach injects the steroid into the epidural space. It’s a common method for cervical epidural steroid injections.
Key considerations:
- Needle placement is critical to avoid complications.
- Fluoroscopic guidance is often used to ensure accurate placement.
- Patient positioning is key to the procedure’s success.
Transforaminal Approach: When and Why It’s Used
The transforaminal approach injects the steroid into the neural foramen. It’s used when pain is focused on a specific nerve root.
The benefits include:
- Targeted delivery of the steroid to the affected nerve root.
- Potential for more effective pain relief.
- Useful for diagnostic purposes to identify the source of pain.
C7-T1 Junction: Special Considerations for Epidural Injection
The C7-T1 junction is a common site for epidural injections. It has a larger interlaminar space. But there are special considerations.
Important factors:
- Anatomical variations can affect needle placement.
- Care must be taken to avoid injury to surrounding structures.
- Fluoroscopic guidance is essential for accurate needle placement.
In conclusion, the choice of technique for cervical epidural steroid administration depends on various factors. These include the patient’s anatomy and the specific condition being treated. We carefully evaluate each patient to determine the most appropriate approach.
The Complete Cervical ESI Procedure: From Preparation to Recovery
The cervical epidural steroid injection (ESI) procedure is a detailed medical process. It needs careful preparation and precise steps. We know patients might feel nervous about this treatment. But with the right guidance, they can feel more confident.
Pre-Procedure Patient Assessment and Preparation
Before a cervical ESI, patients get a full check-up. This ensures they’re right for the treatment. We look at their medical history, current meds, and allergies. A physical exam also checks their nerve health and any risks.
To get ready for the procedure, patients are told to:
- Stop taking blood thinners before the procedure
- Avoid eating or drinking for a while before the injection
- Have someone drive them home after the procedure
Step-by-Step Injection Process
The cervical ESI procedure has several important steps:
- Patient positioning: The patient lies on their stomach or side, depending on the approach.
- Sterilization: The area is cleaned and sterilized to prevent infection.
- Local anesthesia: The area is numbed with a local anesthetic.
- Fluoroscopic guidance: Real-time imaging guides the needle into the epidural space.
- Contrast injection: A contrast agent is used to confirm the needle’s position.
- Steroid administration: The steroid is injected into the epidural space.
Immediate Post-Procedure Monitoring
After the injection, patients are watched closely for any immediate issues. We look for signs of nerve problems, allergic reactions, or other problems. We also check their blood pressure and heart rate.
Recovery Timeline and Activity Guidelines
Recovery times after a cervical ESI vary. Most patients can go back to normal activities in a few days. We advise them to:
- Avoid hard activities for 24-48 hours after the procedure
- Watch the injection site for infection or other issues
- Follow up with their healthcare provider as directed to check the treatment’s success
Understanding the cervical ESI procedure helps patients prepare better. It also improves their chances of a good outcome.
Effectiveness of Cervical Epidural Steroid for Pain Management
Cervical epidural steroid injections are a topic of great interest in medicine. We look into how well they work for chronic pain in the neck.
Expected Duration of Pain Relief
These injections help a lot with neck pain from radiculopathy and spondylosis. How long the pain relief lasts varies a lot. Things like how bad the pain is, how well the injection was done, and the patient’s health matter a lot.
Some people feel better right away, while others take a few days. This shows why treatment plans need to be tailored to each person.
Success Rates for Different Cervical Conditions
How well these injections work can depend on the condition. For example, they really help with cervical radiculopathy. Studies show success rates between 60% and 80% for this.
For cervical spondylosis, the success rates can vary. But, injections are a good option when other treatments don’t work. How much inflammation there is and how much the nerves are compressed play big roles.
Factors Influencing Treatment Outcomes
Many things can affect how well these injections work. These include how well the injection was done, if there’s inflammation, and the patient’s health. Also, whether to use the interlaminar or transforaminal approach can make a difference.
- The severity of the cervical condition
- The presence of comorbidities such as diabetes or osteoporosis
- The patient’s response to previous treatments
Healthcare providers can make treatment plans better by thinking about these factors. This can lead to better results for patients.
Potential Risks and Complications of Cervical Spine Injections
It’s important to know the risks of cervical epidural steroid injections. These injections are usually safe and help with neck pain. But there are risks and complications to be aware of.
Common Side Effects and Their Management
Most people do well with these injections. But, some might feel:
- Temporary increase in pain
- Headache
- Facial flushing
- Insomnia
- Transient blood sugar elevation in diabetic patients
These side effects are usually mild and go away in a few days. We suggest staying hydrated, resting, and using over-the-counter pain relievers if needed.
Rare but Serious Complications
Though rare, serious problems can happen. These include:
- Spinal cord injury or stroke: These are very rare but can happen.
- Infection: Epidural abscess or meningitis are rare but possible risks.
- Nerve damage: This can cause ongoing pain or nerve problems.
It’s important to know that serious problems are more likely with the transforaminal approach.
Risk Factors That Increase Complication Rates
Some factors can make complications more likely. These include:
- Patient-related factors: Being older, having diabetes, or other health issues
- Technique-related factors: The choice of injection method
- Operator experience: The skill of the person doing the injection
Knowing these factors helps us tailor treatment to each patient.
Safety Protocols to Minimize Adverse Events
We follow strict safety rules to lower the risk of problems:
- Using real-time fluoroscopic guidance during the procedure
- Employing sterile technique to prevent infection
- Carefully selecting patients based on their medical history and current condition
- Utilizing the minimum effective dose of corticosteroid
By sticking to these rules, we greatly reduce the chance of bad outcomes and aim for the best results for our patients.
Patient Selection Criteria for Cervical Spondylosis Injections
Choosing the right patients for cervical spondylosis injections is key. It’s about finding the right candidates. Knowing the right technique and understanding the body’s anatomy is also important.
Ideal Candidates for Cervical ESI
Patients with cervical spondylosis symptoms who haven’t gotten better with other treatments are good candidates. They often have cervical radiculopathy or neck pain. A good doctor will check their medical history and do a physical exam to see if they’re a good fit.
Contraindications and Precautions
Some conditions make CESI not safe. These include active infections, coagulopathy, and known allergy to corticosteroids or contrast agents. Doctors also need to be careful with patients who have diabetes or hypertension.
Alternative Treatments for Non-Candidates
For those who can’t have CESI, other treatments are available. Options include physical therapy, oral medications (like NSAIDs or pregabalin), and lifestyle changes. Sometimes, surgery is needed for severe cases.
Integrating ESI into Comprehensive Pain Management
CESI is a part of a bigger pain management plan. It’s often used with physical therapy and medications. The choice to use CESI depends on the patient’s overall health and treatment goals.
Conclusion: Navigating Decisions About Cervical Epidural Treatments
Cervical epidural steroid injections are a great way to manage neck pain and radiculopathy. It’s important to know about the procedure, its benefits, and risks. This helps in making the right choice.
Choosing cervical epidural treatments needs careful thought. You should consider your own situation and medical history. Knowing about needle size, imaging, and how it’s given helps you make a good decision.
Talking to a healthcare professional about your condition and options is key. This way, you can find the best treatment for your neck problem. It could be for cervical radiculopathy or spondylosis.
FAQ
What is a cervical epidural steroid injection?
A cervical epidural steroid injection is a small procedure. It involves putting steroids around the spinal cord in the neck. This helps reduce inflammation and eases pain.
What is the typical needle size used for cervical epidural steroid injections?
The needles used are usually between 22 to 25 gauge. This size is small enough to be precise but not too small to cause harm.
What conditions are treated with cervical epidural steroid injections?
These injections help with conditions like neck pain and radiating symptoms. They are used for cervical radiculopathy, spondylosis, and other inflammatory issues.
How is the cervical epidural space accessed during the injection?
The space is accessed through different methods. The choice depends on the patient’s condition and the doctor’s preference.
What is the role of imaging in cervical epidural steroid injections?
Imaging, like fluoroscopy, is key. It guides the needle placement in real-time. This ensures the procedure is accurate and safe.
What are the possible risks and complications of cervical epidural steroid injections?
While safe, there are risks. These include temporary pain or discomfort. Rare but serious issues like infection or nerve damage can also occur.
How long does pain relief from cervical epidural steroid injections last?
The relief can last weeks to months. Some may need more than one injection to keep the pain away.
Are there any contraindications for cervical epidural steroid injections?
Yes, there are. Conditions like active infections or bleeding disorders are contraindications. Also, certain allergies and precautions for diabetes, hypertension, or specific medications apply.
How are patients prepared for a cervical epidural steroid injection?
Patients get a full assessment. This includes medical history and imaging studies. They are also told what medications to stop before the procedure.
What is the recovery process like after a cervical epidural steroid injection?
Patients are watched for a bit after the procedure. Some can go back to normal activities right away. Others are told to rest for a while to recover better.
Can cervical epidural steroid injections be part of a broader pain management plan?
Yes, they can be part of a bigger plan. This plan might include physical therapy or other medications to manage pain.
References
- Benzon, H. T., Huntoon, M. A., Rathmell, J. P., & American Academy of Neurology (AAN) Panel. (2023, December). Epidural Steroids for Cervical and Lumbar Radicular Pain: A Systematic Review and Meta-Analysis. Neurology. https://pubmed.ncbi.nlm.nih.gov/39938000/
- Epstein, N. E. (2018). Major risks and complications of cervical epidural steroid injections. Surgical Neurology International, 9, 86. https://surgicalneurologyint.com/wp-content/uploads/2018/04/8843/SNI-9-86.pdf
- Narayanaswami, P. (2024, March 29). A new systematic review summarizes the efficacy of epidural spinal injections for chronic back pain. Practical Neurology. https://practicalneurology.com/news/a-new-systematic-review-summarizes-the-efficacy-of-epidural-spinal-injections-for-chronic-back-pain/2473789/
- Benyamin, R., Singh, V., Parr, A. T., Conn, A., Diwan, S., & Abdi, S. (2009). Systematic review of the effectiveness of cervical epidurals in the management of chronic neck pain. Pain Physician, 12(1), 137-157. https://painphysicianjournal.com/current/pdf?article=MTE3NQ%3D%3D&journal=47










