Last Updated on November 26, 2025 by Bilal Hasdemir
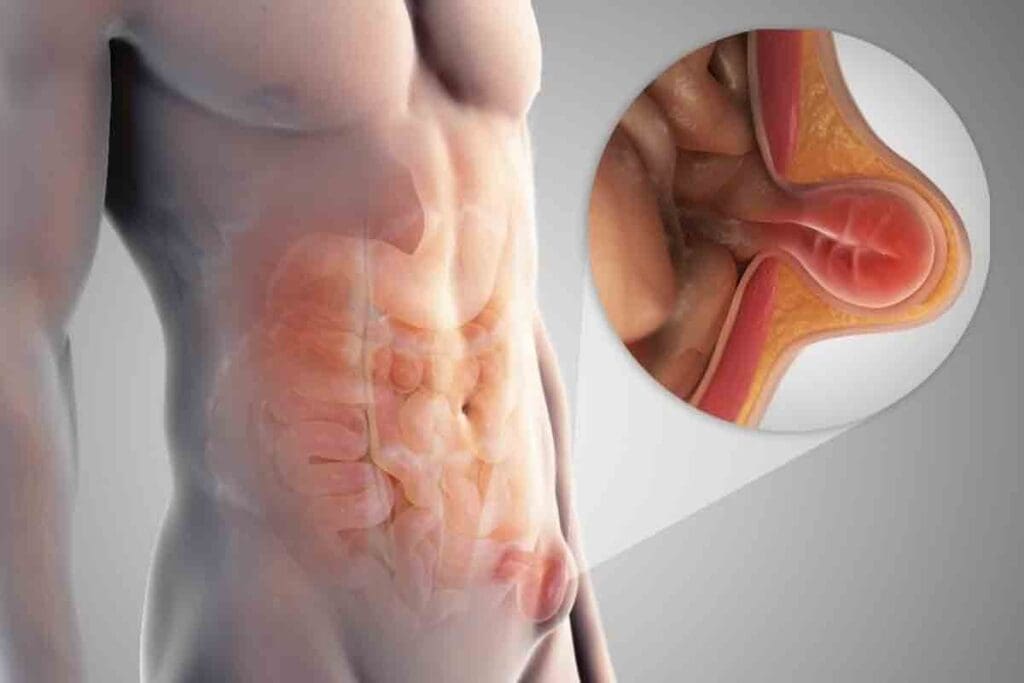
Hernias happen when part of an organ bulges through muscle or tissue. They can occur in different body parts, leading to pain and health issues.
Liv Hospital is known for caring for patients with hernias. It’s important to know the differences between hernia types for quick diagnosis and treatment.
There are many types of hernias, like inguinal, umbilical, and hiatal. Ventral hernias are a big group of hernias in the belly. They often happen in weak spots, maybe after surgery or because of other risks.

Hernias happen due to weak spots in the body and lifestyle choices. A hernia occurs when an organ or tissue bulges through a weak spot in the muscle or fascia. This can cause pain and discomfort.Ventral hernia vs umbilical: what’s the difference? Get the critical facts comparing these 7 hernia types, from inguinal to ventral.
A hernia occurs when an organ or tissue bulges through a weak spot in the muscle or fascia. This can happen in different parts of the body, like the belly, diaphragm, and groin.
Key signs of a hernia include a visible bulge, pain when coughing, lifting, or bending, and a feeling of heaviness or pressure.
Many things can increase the chance of getting a hernia. These include getting older, being overweight, having a chronic cough, and straining from physical activity. These factors can weaken the belly wall or raise pressure inside the belly, making hernias more likely.
The belly wall has layers like skin, subcutaneous tissue, muscles, and fascia. Knowing this helps us understand how hernias like inguinal, ventral, and umbilical ones happen.
The belly wall’s strength comes from its muscles working together. Weakness or defects in these muscles can cause hernias. This shows why knowing the anatomy is key to preventing and treating hernias.
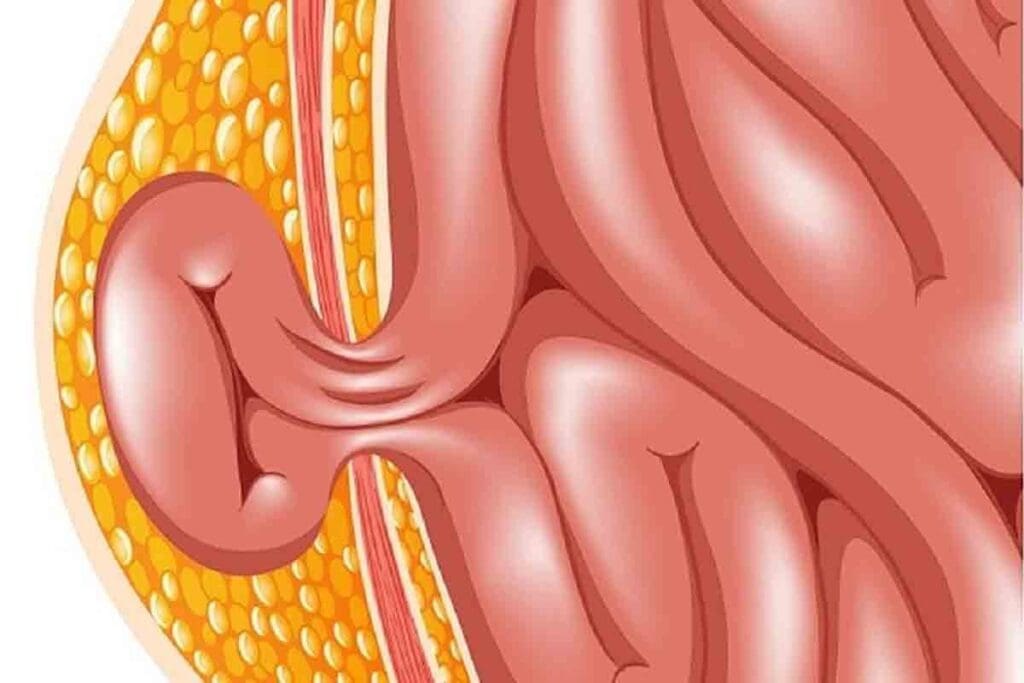
Inguinal hernias are the most common type of hernia, making up about 75% of all cases. They happen when fatty tissue or a small intestine bulge through the inguinal canal into the groin area.
Inguinal hernias are divided into two types: direct and indirect. Indirect inguinal hernias are more common. They occur when tissue enters the inguinal canal through a natural weakness at the internal ring. Direct inguinal hernias happen when tissue forces its way through the abdominal wall in the inguinal canal area. This is usually due to increased pressure or muscle weakness.
Males are more likely to get inguinal hernias because of the natural weakness in the inguinal canal. This area is a passageway through the abdominal wall in the groin. The inguinal canal in males is larger and more complex, making it a weak spot.
| Characteristics | Direct Inguinal Hernia | Indirect Inguinal Hernia |
| Cause | Weakness in the abdominal wall | Congenital or natural weakness at the internal ring |
| Prevalence | Less common | More common |
The symptoms of inguinal hernias vary but often include a bulge in the groin area. This bulge may be more noticeable when standing, lifting heavy objects, or coughing. Discomfort or pain, often when bending over, coughing, or lifting, is also common. Sometimes, the hernia may only show as a visible bulge without any symptoms.
In summary, inguinal hernias are common, mainly in males, and can affect quality of life. Knowing the differences between direct and indirect inguinal hernias and their symptoms is key to diagnosis and treatment.
Ventral hernias are a wide range of abdominal wall hernias, including umbilical hernias. Each type has its own features. Knowing the differences and similarities is key to a correct diagnosis and treatment.
Ventral hernias happen through weak spots in the abdominal wall, not in the groin. They can show up anywhere along the midline of the abdomen, from the breastbone to the pubic bone.
Ventral hernias include umbilical, epigastric, and incisional hernias. Each has its own characteristics.
Umbilical hernias are a type of ventral hernia near the navel. They are common in infants and some adults, like pregnant women.
Umbilical hernias often form because of the natural weakness in the abdominal wall where the umbilical cord was once attached.
Both ventral and umbilical hernias have similar risk factors. These include obesity, pregnancy, and previous abdominal surgery. These factors can raise intra-abdominal pressure and strain the abdominal wall, causing hernias.
| Risk Factor | Ventral Hernia | Umbilical Hernia |
| Obesity | High Risk | High Risk |
| Pregnancy | Moderate Risk | High Risk |
| Prior Surgery | High Risk | Moderate Risk |
Knowing these risk factors is important for preventing and catching both ventral and umbilical hernias early.
Epigastric hernias are less common but pose unique challenges. They occur above the belly button in the epigastric region. Knowing about these hernias is key to the right diagnosis and treatment.
Epigastric hernias happen in the upper belly, between the belly button and the chest. This spot is prone to hernias because of weak spots in the belly wall. Their location makes them stand out in diagnosis.
These hernias push fatty tissue through a belly wall defect. Over time, they can grow, causing pain and other issues. Factors like obesity and high blood pressure can speed up their growth.
Key factors influencing epigastric hernia progression:
Epigastric and ventral hernias differ in the belly wall. Epigastric hernias are above the belly button, while ventral hernias can be anywhere. Knowing these differences is vital for correct diagnosis and treatment.
| Hernia Type | Location | Characteristics |
| Epigastric Hernia | Above the umbilicus | Involves fatty tissue protrusion |
| Ventral Hernia | Anywhere on the abdominal wall | Can involve various contents, including intestine |
In summary, epigastric hernias are unique due to their location and nature. Understanding them is vital for proper management and treatment.
The diaphragm is a key muscle for breathing. But a hiatal hernia can push the stomach through it. This can cause digestive problems and discomfort. Knowing about hiatal hernias helps in treating symptoms well.
Hiatal hernias are mainly of two types: sliding and paraesophageal hernias. Sliding hiatal hernias happen when the stomach moves up into the chest. This is the most common type and can cause heartburn and regurgitation.
Paraesophageal hernias occur when part of the stomach bulges through the diaphragm. This can lead to serious problems, like strangulation.
Hiatal hernias are linked to Gastroesophageal Reflux Disease (GERD) and other digestive issues. When the stomach bulges through the diaphragm, stomach acid can flow back into the esophagus. This can cause heartburn, chest pain, and trouble swallowing.
It’s important to understand the connection between hiatal hernias and GERD. This helps in managing symptoms and avoiding more problems.
It’s key to tell hiatal hernias apart from other abdominal hernias. Unlike inguinal and umbilical hernias, hiatal hernias involve the stomach bulging through the diaphragm.
| Hernia Type | Location | Common Symptoms |
| Hiatal Hernia | Diaphragm | Heartburn, Regurgitation, Chest Pain |
| Inguinal Hernia | Groin | Bulge in the Groin, Discomfort during Coughing or Lifting |
| Umbilical Hernia | Belly Button | Bulge around the Navel, Pain or Discomfort |
This comparison shows the unique features of hiatal hernias. It highlights the need for accurate diagnosis.
Diaphragmatic hernias happen when there’s a hole in the diaphragm. This lets organs from the belly move into the chest. They can be either congenital or acquired.
Congenital diaphragmatic hernias (CDH) are present at birth. They cause organs to move into the chest. This can lead to breathing problems and high blood pressure in the lungs.
The exact reason for CDH is not fully understood. It’s thought to be caused by genetics and environment.
Acquired diaphragmatic hernias happen later in life. They can be caused by accidents or increased pressure in the belly. They can also come from surgery or other health issues.
Diaphragmatic hernias are different from inguinal and umbilical hernias. They happen in the diaphragm, not in the groin or navel. Knowing the differences helps doctors treat them right.
Diaphragmatic hernias need a special surgery. This is different from the surgery for other hernias.
In conclusion, diaphragmatic hernias are complex. They need a deep understanding of their causes, symptoms, and treatments. By comparing them with other hernias, doctors can better help patients.
After surgery, some people get incisional hernias, a kind of ventral hernia. These hernias happen through scars from past surgeries. This is a big worry for those who have had belly surgery.
Many things can make incisional hernias more likely. These include surgical technique, wound infection, and patient comorbidities like obesity and diabetes. Also, poor healing and high pressure inside the belly can play a part.
The chance of getting an incisional hernia depends on the surgery type. Laparotomy incisions are more likely to herniate than laparoscopic ones. Smoking and malnutrition can also hurt healing and raise the risk.
Incisional hernias fall under the ventral hernia category, which also includes umbilical and epigastric hernias. Knowing the differences between these is key to treatment. Incisional hernias happen through scars from past surgeries, unlike umbilical hernias near the belly button.
When we compare ventral hernia vs inguinal hernia, ventral hernias, like incisional ones, happen in the belly wall. Inguinal hernias are in the groin. This is important for choosing the right treatment.
To prevent incisional hernias, we need to improve surgery techniques and handle wound infections quickly. We also need to manage patient health issues. Using minimally invasive surgical techniques and mesh reinforcement during surgery can help, too.
Even with these steps, there’s a chance of the hernia coming back. The size of the hernia, the repair method, and any complications can affect this. Keeping an eye on patients after surgery and fixing any problems fast is key to lowering the risk of recurrence.
Inguinal hernias are more common, but femoral hernias are more dangerous. They happen through the femoral canal, below the inguinal ligament. Femoral hernias are more common in women than in men.
Femoral hernias occur through the femoral canal. This canal is a weak spot in the abdominal wall. It’s more prone to herniation.
Key anatomical features that contribute to femoral hernia formation include:
Femoral hernias have a higher risk of strangulation than other hernias. Strangulation happens when the blood supply to the herniated tissue is cut off. This is a medical emergency that needs immediate attention.
“The risk of strangulation in femoral hernias is significantly higher than in inguinal hernias, stressing the need for quick diagnosis and treatment.”
Distinguishing between femoral and inguinal hernias can be tricky. Accurate diagnosis is ketoor proper treatment. Femoral hernias are below the inguinal ligament, while inguinal hernias are above it.
Diagnostic considerations include:
Understanding the differences between femoral and inguinal hernias is vital for healthcare providers. Each type has unique anatomical locations and risks. This requires a personalized approach to patient care.
Hernias can cause serious problems if not treated properly. Different hernias, like inguinal, umbilical, and hiatal, face similar risks. It’s important to know these risks to get the right treatment.
Knowing about complications like strangulation, incarceration, and obstruction is key. These can happen with many hernias and need quick medical help.
Strangulation cuts off blood to the hernia, causing tissue death. It’s a serious emergency needing immediate surgery. Some hernias, like femoral, are more at risk because of where they are.
Symptoms of strangulation include severe pain, nausea, vomiting, and fever. Spotting these symptoms early is vital to avoid serious problems.
Incarceration is when a hernia gets stuck and can’t go back in. This can block the intestine, causing severe pain, nausea, and vomiting. These are serious issues that might need emergency surgery.
The risk of these problems depends on the hernia’s size, how long it’s been there, and adhesions. Knowing these factors can help prevent complications.
Pain is a common sign of hernia problems. A sudden increase or change in pain can mean incarceration or strangulation. It’s important to recognize these signs for timely treatment.
Different hernias cause different types of pain. For example, inguinal hernias hurt in the groin, while hiatal hernias cause chest pain. Knowing these differences helps in diagnosing and treating complications.
Comparing hernias like hiatal hernia vs epigastric hernia or ventral hernia vs hiatal hernia helps understand their unique risks. For instance, hiatal and epigastric hernias both involve protrusions but have different locations and risks.
| Hernia Type | Common Complications | Symptoms of Complications |
| Inguinal Hernia | Incarceration, Strangulation | Groin pain, nausea, vomiting |
| Hiatal Hernia | GERD, Obstruction | Chest pain, difficulty swallowing |
| Umbilical Hernia | Incarceration, Strangulation | Abdominal pain, nausea |
| Ventral Hernia | Incarceration, Obstruction | Abdominal pain, vomiting |
In conclusion, knowing the complications and emergencies of different hernias is key. Recognizing risks and symptoms of complications like strangulation, incarceration, and obstruction helps in making informed decisions. This can prevent serious outcomes.
It’s important to know the differences between various hernias. This includes understanding ventral hernia vs umbilical and inguinal hernia vs ventral hernia. Each has its own unique characteristics and treatment options, from waiting to see if it gets better to surgery.
When looking at epigastric hernia vs hiatal hernia, the location and symptoms matter a lot. Liv Hospital aims to offer top-notch care. They help patients make the best choices for their treatment.
Knowing the causes, risks, and possible complications of different hernias is key. Patients can work with their doctors to find the best treatment plan. Whether it’s a ventral, inguinal, or another type of hernia, making informed choices is essential for success.
A hiatal hernia happens when the stomach bulges through the diaphragm. An epigastric hernia, on the other hand, is a ventral hernia. It occurs above the belly button and often involves fatty tissue.
Inguinal hernias show up in the groin area. Umbilical hernias appear near the navel. Inguinal hernias are more common in men. Umbilical hernias are seen more in infants and women.
Ventral hernias cover a wide range and include umbilical hernias. Umbilical hernias are a specific type of ventral hernia. They happen near the navel.
Diaphragmatic hernias involve organs bulging through the diaphragm. They can be present at birth or develop later. Inguinal and umbilical hernias occur in the abdominal wall. They have different causes and risk factors.
Femoral hernias occur through the femoral canal and are more common in women. Inguinal hernias happen in the groin area and are more common in men. Femoral hernias are at a higher risk of strangulation.
Incisional hernias can happen due to obesity, poor wound healing, and previous abdominal surgery.
Each type of hernia can cause complications like strangulation, incarceration, and obstruction. This happens when the herniated tissue gets trapped or compromised.
Symptoms of a strangulated hernia include severe pain, nausea, vomiting, and fever. These symptoms need immediate medical attention.
Treatment for hernias varies. It can range from watchful waiting to surgical repair. The choice depends on the type and severity of the hernia.
Sliding hiatal hernias have the stomach sliding up into the chest. Paraesophageal hiatal hernias have the stomach bulging up beside the esophagus.
No, ventral hernias are a broader category that includes epigastric hernias. Epigastric hernias are a specific type of ventral hernia. They occur above the umbilicus.
Yes, umbilical hernias can happen in adults. They are more common in women and people with obesity or previous abdominal surgery.
Obesity is a common risk factor for many hernias. This includes inguinal, umbilical, and ventral hernias.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!