Last Updated on November 26, 2025 by Bilal Hasdemir
When thinking about cerebral embolization procedures for issues like aneurysms or arteriovenous malformations, knowing the risks is key. At Liv Hospital, we help our patients through every step, making sure they get the best care.
Embolization is a treatment for cerebral arteriovenous malformations (AVMs). It’s a less invasive way to stop blood flow to these abnormal blood vessels. But, it’s important to know about the possible brain embolization side effects, which can vary from mild to severe.
We’ll talk about the 7 main risks of brain embolisation. This will help you make a well-informed choice about your treatment.
Key Takeaways
- Understanding the risks associated with cerebral embolization procedures.
- The importance of embolization in treating cerebral arteriovenous malformations.
- Potential side effects can range from mild to severe.
- Liv Hospital’s commitment to patient-centered care and clinical excellence.
- Guiding patients through every step of the embolization process.
What Is Brain Embolization and When Is It Used?
Brain embolization is a medical procedure that stops blood flow to certain brain areas. It’s key for treating conditions like aneurysms and arteriovenous malformations (AVMs).
Definition and Purpose of Brain Embolization
Brain embolization, also known as cerebral embolization, is a minimally invasive method. It delivers embolic materials to block blood flow in the brain. The main goal is to stop further bleeding or reduce the risk of rupture in aneurysms.
A study in the Journal of NeuroInterventional Surgery shows its importance. It says endovascular embolization is a key treatment for cerebral aneurysms. It’s a less invasive option compared to surgical clipping.
This shift towards endovascular techniques reflects the ongoing advancements in the field of neurointervention.
Conditions Treated with Embolization Procedures
Embolization procedures treat several conditions, including:
- Aneurysms: Abnormal dilations of blood vessels that can rupture and cause bleeding.
- Arteriovenous Malformations (AVMs): Abnormal connections between arteries and veins.
- Tumors: Certain types of brain tumors can be treated with embolization to reduce their blood supply.
| Condition | Description | Treatment Goal |
| Aneurysms | Abnormal dilation of blood vessels | Prevent rupture and bleeding |
| AVMs | Abnormal connections between arteries and veins | Reduce risk of hemorrhage |
| Tumors | Cancerous growths | Reduce blood supply to the tumor |
Types of Brain Embolization Techniques
Several techniques are used in brain embolization, including:
- Coil Embolization: Using coils to fill an aneurysm and prevent further blood flow.
- Liquid Embolization: Using liquid embolic agents to occlude AVMs or other vascular lesions.
- Particle Embolization: Using particles to embolize tumors or other conditions.
Knowing about the different brain embolization techniques helps patients make informed decisions about their care.
How Brain Embolization Procedures Are Performed

To understand brain embolization, it’s important to know how it’s done. These procedures use an endovascular approach. This means going through blood vessels to get to the target area.
The Endovascular Approach
The endovascular method is a minimally invasive technique. A catheter is inserted through a blood vessel in the groin or arm. It’s then guided to the brain using real-time imaging. This allows the practitioner to place embolic materials exactly where needed.
Materials and Devices Used
Many materials and devices are used in brain embolization procedures. These include:
- Catheters and guidewires for navigation
- Embolic agents like coils, particles, or liquid materials
- Stents or balloon catheters for support
The choice of materials depends on the condition being treated and the patient’s anatomy.
Duration and Recovery Timeline
The time needed for a brain embolization procedure varies. It can be from 30 minutes to several hours, depending on the case. Recovery times also vary, but most patients stay in the hospital for at least 24 hours after the procedure. Full recovery can take several days to weeks.
Common Brain Embolization Side Effects
Brain embolization is a treatment for many conditions. But, it’s important to know the common side effects. This helps patients understand what to expect after treatment.
Post-Procedure Headaches
Headaches are a common side effect after brain embolization. They can be mild or severe. Headaches are usually treated with medication and get better in a few days.
Nausea and Fatigue
Nausea and fatigue are also common after the procedure. They happen because of how the body reacts to the treatment. Rest and drinking plenty of water help to get better quickly.
Localized Pain and Discomfort
Some people feel pain or discomfort where the embolization was done. This pain is usually not too bad and can be eased with medication. It will get better as the body heals.
| Common Side Effects | Typical Duration | Management Strategies |
| Post-procedure headaches | A few days to a week | Medication, rest |
| Nausea and fatigue | A few days to a week | Rest, hydration |
| Localized pain and discomfort | A few days to several weeks | Pain relief medication |
Knowing about these side effects helps patients prepare for recovery. It also tells them when to see a doctor if symptoms get worse or don’t get better.
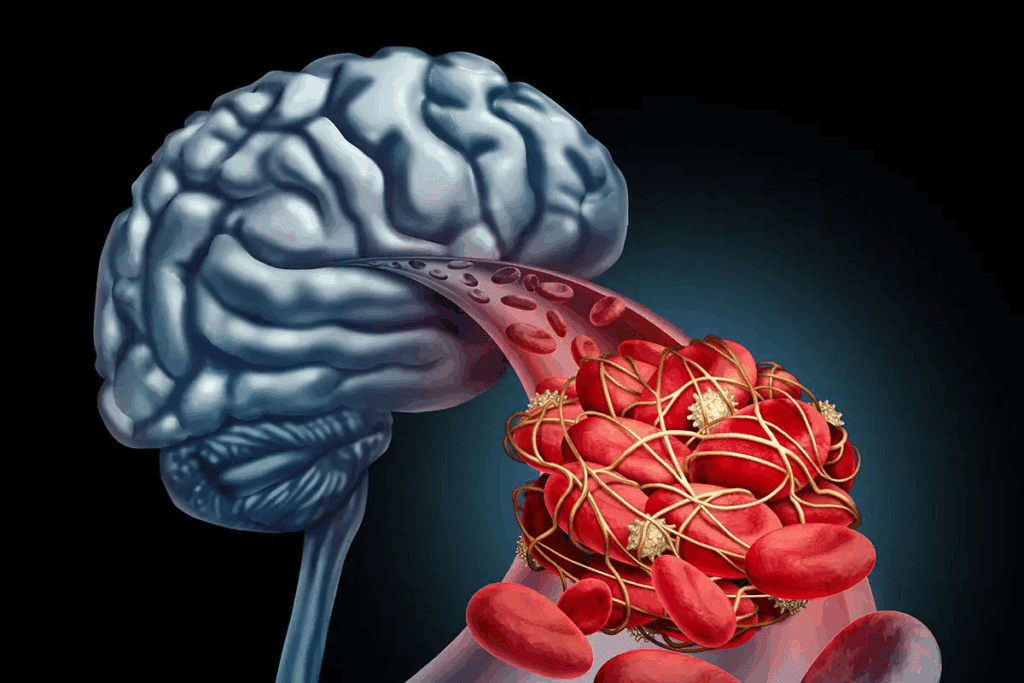
Risk #1: Ischemic Complications
Brain embolization carries a risk of ischemic complications. These complications can happen when the procedure reduces blood flow to brain areas.
Understanding Ischemic Events
Ischemic events happen when blood flow to the brain is cut off. This can damage brain tissue. In brain embolization, these events can be caused by blockages or procedural issues.
Symptoms of Ischemic Complications
Symptoms of ischemic complications vary based on the brain area affected. They can include sudden weakness, trouble speaking, and vision problems. It’s important to recognize these symptoms quickly.
Treatment Approaches for Ischemia
Treatment for ischemia after brain embolization aims to restore blood flow. This might involve thrombolytic therapy or mechanical thrombectomy. Acting fast is key to avoiding lasting brain damage.
A medical expert stresses the importance of early treatment. “Quick action is essential for better outcomes in brain embolization patients.”
“The key to managing ischemic complications lies in swift and appropriate action.” As highlighted by professionals
Risk #2: Hemorrhagic Complications
Hemorrhagic complications are a big worry for those getting brain embolization treatments. We want to make sure patients know about these risks. They can happen during or after the treatment.
Post-Procedural Hemorrhage
Post-procedural hemorrhage is a risk after certain surgeries. This can happen for a few reasons, like an aneurysm rupturing or embolic material moving.
Aneurysm Rupture During Treatment
Aneurysm rupture during treatment is a serious issue. It’s rare but needs careful watching and quick action from the medical team.
Emergency Management of Bleeding
When bleeding happens, acting fast is key. Doctors might do an immediate check-up to find where the bleeding is. Then, they might use more coils or special agents to stop it.
| Complication | Risk Factors | Management |
| Post-Procedural Hemorrhage | Aneurysm size, location, and shape | Immediate angiography, coiling, or hemostatic agents |
| Aneurysm Rupture | Aneurysm wall weakness, procedural factors | Emergency coiling, balloon remodeling |
| Hemorrhagic Complications | Patient health, procedural complexity | Close monitoring, preparedness for emergencies |
It’s important for patients to know about these risks and how they’re handled. We aim to give the best care and support to lessen these risks.
Risk #3: Neurological Deficits
Brain embolization is a treatment for some vascular conditions. But, it comes with a risk of neurological deficits. This is because the procedure involves working with blood vessels in the brain.
Temporary vs. Permanent Deficits
Neurological deficits from brain embolization can be either short-term or permanent. Short-term deficits might go away in a few days or weeks. But, permanent deficits can greatly affect a patient’s life.
A study in a top medical journal found that brain aneurysm embolization patients face a higher risk of neurological deficits. This is compared to those having other endovascular procedures.
Cranial Nerve Palsy
Cranial nerve palsy is a type of neurological deficit that can happen after brain embolization. It occurs when the cranial nerves get damaged during the procedure. Symptoms include facial weakness, double vision, or trouble swallowing.
Cognitive and Motor Function Impacts
The procedure can also affect cognitive and motor functions. Patients might have memory problems, trouble focusing, or weakness in their limbs. The severity of these effects depends on the procedure’s location and complexity.
| Potential Neurological Deficits | Symptoms | Possible Outcomes |
| Temporary Deficits | Reversible symptoms such as weakness or numbness | Full recovery expected |
| Permanent Deficits | Lasting symptoms including paralysis or cognitive impairment | Long-term impact on quality of life |
| Cranial Nerve Palsy | Facial weakness, double vision, or swallowing difficulties | Variable recovery; may require rehabilitation |
It’s important for patients thinking about arteriovenous malformation embolization or cerebral embolisation to know these risks. Talking to a healthcare provider about these risks is key to making an informed choice.
“The risk of neurological deficits is a critical consideration in the decision-making process for brain embolization. Patients should be thoroughly informed about the possible risks and benefits to ensure they are prepared for any outcome.”
Peer-reviewed neurosurgical studies emphasize.
Risk #4: Stroke as a Serious Complication
Stroke is a serious risk during or after brain embolization. It’s important for patients and doctors to understand this. Knowing about stroke helps everyone involved.
Mechanism of Stroke During Embolization
Stroke can happen when a clot moves to the wrong place in the brain. Endovascular embolization is precise but can block blood flow. This can lead to ischemic strokes in important brain areas.
Risk Factors That Increase Stroke Likelihood
Several things can make stroke more likely during brain embolization. These include the patient’s health before the procedure, the complexity of the issue being treated, and the challenges during coil embolization for aneurysm. Knowing these helps decide if the benefits outweigh the risks.
“The risk of stroke during embolization procedures is a critical factor that necessitates careful patient selection and meticulous procedural technique.”
According to interventional neuroradiology specialists.
Outcomes and Recovery After Procedural Stroke
Recovery from a stroke caused by brain embolization varies. Some fully recover, while others face lasting brain damage. Quick action and close monitoring are key to managing stroke.
In summary, while stroke is a serious risk of brain embolization, knowing about it can help. It’s vital for patients to talk about their risks with their doctors.
Risk #5: Vessel Perforation and Damage
Brain embolization can lead to serious issues like vessel perforation. This is a major concern for us. It can greatly affect how well a patient does.
Causes of Vessel Perforation
Vessel perforation can happen for many reasons. These include the use of catheters and guidewires. Also, the complexity of blood vessel anatomy and diseases can play a part. Coil embolization for aneurysms needs to be done very carefully to avoid these problems.
Immediate Consequences
The effects of vessel perforation can be very bad. They can include bleeding, the need for urgent care, and even life-threatening issues. It’s very important to quickly spot and handle these problems.
Treatment Options for Vessel Damage
There are ways to treat damage from aneurysm embolization. These include using endovascular methods like coiling or stent deployment. Sometimes, surgery is needed to fix the damage.
| Cause | Consequence | Treatment |
| Catheter/guidewire use | Hemorrhage | Coiling |
| Vascular anatomy complexity | Emergency need for intervention | Stent deployment |
| Underlying vascular disease | Life-threatening complications | Surgical repair |
It’s key for both doctors and patients to know about the risks of vessel damage. By understanding these risks, we can work to prevent and manage them. This helps ensure the best results for those going through cerebral embolisation.
Risk #6: Device and Material Complications
Devices and materials used in brain embolization can pose risks. It’s important for patients to know about these risks. This knowledge helps them make better choices about their treatment.
Coil Migration Issues
Coil migration is a problem where the coil moves from its place. This can cause serious issues. It might need more procedures to fix the coil or deal with complications.
Allergic Reactions to Embolization Materials
Some people may have allergic reactions to the materials used in embolization. These reactions are rare but can be severe. They need quick medical attention.
Long-term Implant Considerations
It’s also important to think about the long-term effects of implants. The durability and how well they work over time can affect patient outcomes. Regular checks are needed to make sure the implant is safe and effective.
| Complication | Description | Potential Consequences |
| Coil Migration | Coil moves from intended position | Additional procedures, possible serious complications |
| Allergic Reactions | Reaction to embolization materials | Severe reactions needing quick medical help |
| Long-term Implant Issues | Durability and compatibility concerns | Regular monitoring needed, risk of device failure |
It’s key for patients to understand the risks of device and material complications in brain embolization. Knowing these risks helps them talk better with their healthcare provider. This way, they can make more informed decisions about their care.
Risk #7: Recurrence and Treatment Failure
Brain embolization carries a risk of recurrence and treatment failure. Patients undergoing brain embolization surgery should know this. It’s possible for the treated condition to come back or for the treatment to not fully work.
Recanalization of Treated Areas
Recanalization is when blood flow returns to a treated area. This can happen with coil embolization aneurysm procedures. The aneurysm might reopen over time. We watch patients for signs of this to act quickly.
Incomplete Embolization Outcomes
Sometimes, the embolization procedure doesn’t fully treat the area. It’s important to know the difference between an aneurysm and an embolism. If treatment is not complete, there’s a risk of rupture or other problems.
Need for Additional Procedures
If treatment doesn’t work or the condition comes back, more procedures might be needed. We talk with our patients about this possibility. Together, we figure out the best next steps for a good outcome.
Conclusion: Making Informed Decisions About Brain Embolization
It’s important for patients to know the risks and benefits of brain embolization. We’ve talked about 7 key side effects and risks. These include ischemic and hemorrhagic complications, and neurological deficits.
Knowing these risks helps patients make better choices about their treatment. The procedure can be effective for some medical conditions. But, it’s key to talk about these risks and benefits with a doctor to find the best treatment.
Being aware of possible side effects helps patients feel more confident in their treatment choices. We’re here to support and guide patients through brain embolization procedures.
FAQ
What is brain embolization?
Brain embolization is a procedure that blocks blood flow to certain brain areas. It’s used to treat conditions like aneurysms and arteriovenous malformations (AVMs).
What are the common side effects of brain embolization?
Side effects include headaches, nausea, and fatigue. You might also feel pain or discomfort where the catheter was inserted.
What are ischemic complications in brain embolization?
Ischemic complications happen when brain tissue doesn’t get enough blood. This can cause damage or stroke. Symptoms include sudden weakness, confusion, or trouble speaking.
What is the risk of hemorrhagic complications during brain embolization?
Hemorrhagic complications are serious and involve bleeding in or around the brain. Risks include post-procedure bleeding and aneurysm rupture.
Can brain embolization cause neurological deficits?
Yes, it can lead to neurological deficits. These can be temporary or permanent. They might affect your cognitive and motor functions.
How does stroke occur as a complication of brain embolization?
Stroke can happen if a blood clot or debris blocks a brain blood vessel. Risks include the procedure’s complexity and pre-existing vascular conditions.
What is vessel perforation, and how is it managed?
Vessel perforation is when a blood vessel is accidentally punctured. It can cause bleeding. Treatment might include emergency endovascular repair or surgery.
What are device and material complications in brain embolization?
Complications include coil migration and allergic reactions to materials used. Coil migration means the coils move out of place. Allergic reactions can occur to the materials.
Can brain embolization fail, or is additional treatment needed?
Yes, it can fail. This might mean the treated area recanalizes or isn’t fully embolized. More procedures might be needed to achieve the desired outcome.
What is the difference between an aneurysm and an embolism?
An aneurysm is a blood vessel bulge. An embolism is when a clot blocks a blood vessel. Brain embolization treats aneurysms by blocking blood flow.
What is endovascular embolization?
Endovascular embolization is a procedure where a catheter delivers materials to block blood flow. It’s used for aneurysms and AVMs.
What is coil embolization for aneurysm treatment?
Coil embolization uses tiny coils to fill an aneurysm. This promotes clotting and blocks further blood flow.
References
- Sugiu, K., or others. (2008). Complications of embolization for cerebral arteriovenous malformations. Journal of Neurosurgery, 109(3), 463-468. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3522223/
- Ahmad, S. (2020). Clinical outcome of endovascular coil embolization for cerebral aneurysms in Asian population in relation to risk factors: a 3-year retrospective analysis. BMC Surgery, 20, Article 104. https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-020-00756-1