Last Updated on November 27, 2025 by Bilal Hasdemir
Spinal disc problems can be confusing. But knowing the difference between a bulging disc and a herniated disc is key. At Liv Hospital, we focus on you to explain how each affects your health and treatment.
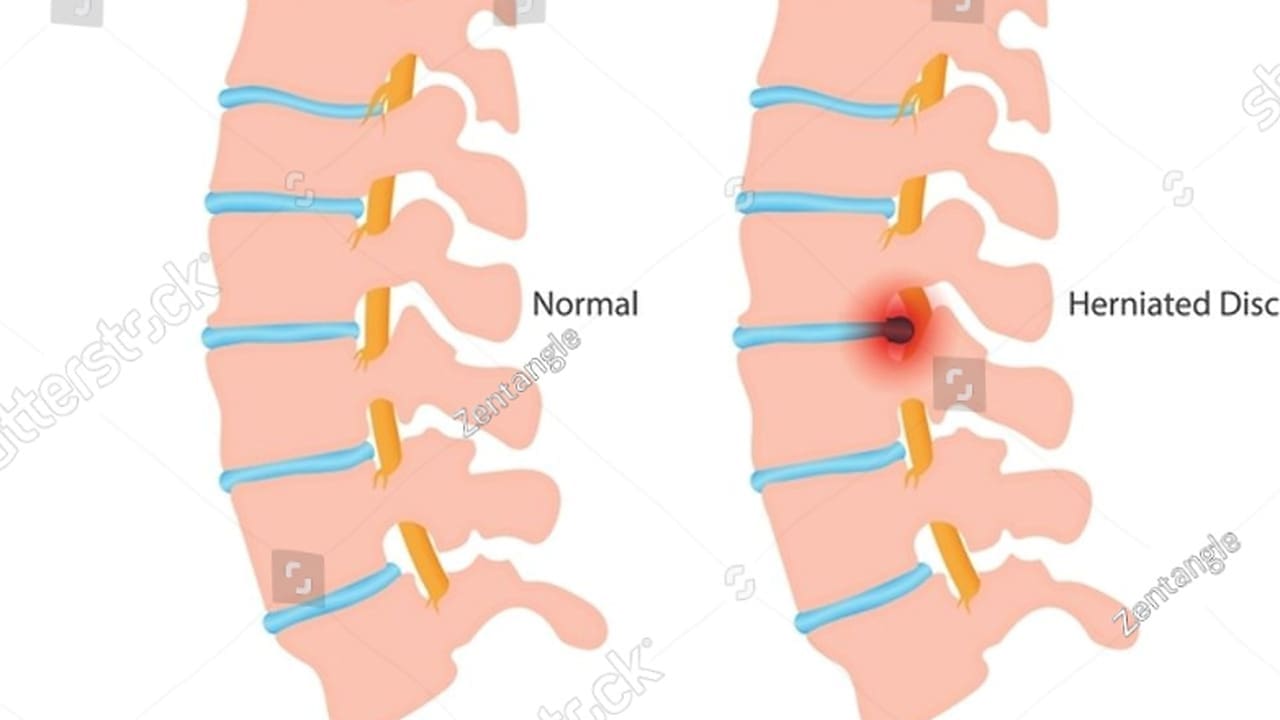
A bulging disc happens when the disc’s outer layer bulges out but stays together. This affects a wider area of the disc. On the other hand, a herniated disc occurs when a tear lets the softer inner core leak out. This can cause more serious symptoms.
We’ll walk you through the differences. And help you see the treatment options available.
To understand spinal disc issues, we first need to know about their anatomy and function. The intervertebral disc is between two vertebral bodies. It’s key for the spine’s flexibility and shock absorption.
A healthy spinal disc has three main parts: the nucleus pulposus at its center, the annulus fibrosus around it, and a thin fibrocartilage layer. The nucleus pulposus is like a gel that absorbs shock. The annulus fibrosus is a tough ring that holds the nucleus and supports the disc.
Spinal discs have several roles in the vertebral column:
Disc problems can happen anywhere in the spine. But, they’re more common in certain spots due to stress and wear. The most affected areas are:
Knowing about spinal disc anatomy is key for diagnosing and treating disc problems.
Understanding the difference between bulging and herniated discs is key for treatment. Both affect the spinal discs but in different ways. This impacts how we care for each condition.
A bulging disc stays mostly intact, bulging outward but not torn. On the other hand, a herniated disc has a tear. This allows the soft center to leak out.
| Characteristics | Bulging Disc | Herniated Disc |
|---|---|---|
| Structural Integrity | Remains intact, bulges outward | Tear in the annulus fibrosus |
| Nucleus Pulposus | Contained within the disc | Leaks out through the tear |
| Symptoms | Typically less severe | Often more severe, potentially with nerve compression |
Many think bulging and herniated discs are the same. But they’re not. They have different effects on treatment. Another myth is that a bulging disc always turns into a herniated one. This isn’t true.
“The distinction between a bulging disc and a herniated disc is not just semantic; it has real implications for patient care and treatment outcomes.” –
Spine Specialist
The difference between bulging and herniated discs affects treatment. A bulging disc might just need physical therapy and pain meds. But a herniated disc might need surgery, if nerves are compressed.
Every patient is different, and treatment must match their needs. Accurate diagnosis helps us tailor care. This improves results and makes patients happier.
A bulging disc happens when the tough outer layer of a spinal disc bulges out but doesn’t break. This is a common issue in the spine and can cause pain for many people.
A bulging disc shows when the disc’s tough outer layer, called the annulus fibrosus, bulges out. But, unlike a herniated disc, the outer layer stays strong, and the disc doesn’t break. On MRI scans, a bulging disc looks like a soft bulge beyond the vertebrae.
Bulging discs can come from getting older, repeated strain on the spine, or genetics. As we age, our spinal discs lose water and can bulge more easily.
Getting a bulging disc is often a slow process. It can get worse with heavy lifting, bending, or sudden twists. Knowing these risks helps prevent and manage bulging discs.
How a bulging disc progresses can differ a lot between people. Some might not feel any pain, while others might have a lot of discomfort or nerve problems if the disc presses on nerves.
| Characteristics | Bulging Disc | Herniated Disc |
|---|---|---|
| Outer Layer Integrity | Remains intact | Ruptured |
| Disc Protrusion | Diffuse protrusion | Focal protrusion |
| Symptoms | Variable, often mild | Often severe, may include radiculopathy |
It’s key to know that bulging discs are often a part of aging. Understanding and managing them can help ease pain and improve life quality.
A herniated disc happens when the outer layer of the disc tears. This lets the softer inner core leak out. This can cause pain and discomfort, mainly if it presses on nearby nerves.
It’s important to know how spinal discs work to understand herniations. A spinal disc has two main parts: the tough outer layer called the annulus fibrosus, and the softer, gel-like inner core, the nucleus pulposus.
The annulus fibrosus keeps the nucleus pulposus inside. But if it tears, the nucleus pulposus can leak out, causing a herniated disc. Many things can cause this, like getting older, injuries, or strains.
When the annulus fibrosus tears, the nucleus pulposus can leak out. This can irritate nearby nerves, leading to pain, numbness, or weakness in the back or limbs, depending on where the herniated disc is.
Herniated discs are also called slipped discs, ruptured discs, and protruded discs. These names all mean the same thing: the disc’s inner material leaks out through a tear in the outer layer.
It’s key to know that while bulging discs and herniated discs both involve the spinal disc, they are different. They have different signs and need different treatments.
Bulging and herniated discs come from many factors like age, job, and lifestyle. Knowing these can help prevent and treat them.
Bulging discs often happen due to wear and tear in the spine. This can be from age-related wear and tear, repeated strain, or bad posture. These issues can make the discs lose height and flexibility, causing them to bulge.
Herniated discs happen when the annulus fibrosus ruptures. This lets the nucleus pulposus spill out. It can be from sudden injury, lifting wrong, or degenerative disease.
Age is a big risk for bulging and herniated discs. As we get older, our spinal discs lose water and flexibility. This makes them more likely to bulge or herniate.
Some jobs and lifestyles raise the risk of these discs. Jobs that involve heavy lifting, bending, or twisting are risky. So is a sedentary life or smoking. Staying fit and exercising can lower these risks.
Knowing what causes bulging and herniated discs helps protect our spines. It helps us avoid these problems.
Bulging and herniated discs can both cause pain, but they have different symptoms. Knowing these differences is key for the right diagnosis and treatment.
Bulging discs often lead to pain and stiffness in the spine area. The pain is usually dull and can spread to nearby spots. For example, a bulging disc in the lower back might cause pain in the buttocks or thighs.
On the other hand, a bulging disc in the neck could lead to shoulder or arm pain. Bulging discs are generally less severe than herniated discs. Yet, they can sometimes irritate nerves, causing numbness, tingling, or weakness in the limbs.
Herniated discs have more intense symptoms than bulging discs. When the outer layer of the disc ruptures, it can irritate nearby nerves. This often leads to sharp, shooting pains that follow the nerve’s path.
Common symptoms include radiculopathy, which is pain, numbness, tingling, or weakness along the nerve’s path. For instance, a herniated disc in the lower back can cause sciatica, pain that goes from the lower back to the leg and foot.
Nerve compression happens when a disc problem puts pressure on a nerve. This can cause radiculopathy, with symptoms like pain, numbness, tingling, or weakness. The severity of radiculopathy depends on how much the nerve is compressed and which nerve it is.
Radiculopathy can really affect your daily life, making simple tasks hard. It’s important to see a doctor quickly to figure out the cause and start treatment.
While many disc problems can be treated without surgery, some symptoms need urgent care. These include sudden, severe pain; numbness or weakness in the limbs; loss of bladder or bowel control; and trouble walking or staying balanced.
If you have any of these severe symptoms, get medical help right away. Quick action can prevent lasting damage and improve treatment results.
To diagnose bulging and herniated discs, we use a mix of clinical checks and imaging. These tools help us see the discs’ condition and plan the best treatment.
First, we do a detailed physical check. We look at patients’ health history and do neurological tests. We also check for nerve problems. This helps us choose the right imaging tests.
Magnetic Resonance Imaging (MRI) is key for seeing spinal discs. It tells us if a disc is bulging or herniated by showing if the nucleus has broken through. We look at MRI scans closely to make this call.
Though MRI is best for soft tissues, CT scans and X-rays are great for bones. They help us see the spine’s alignment, find fractures, and check disc space.
At times, we suggest electromyography (EMG) and nerve conduction studies (NCS). These tests check nerve function and spot damage. They help us see how disc issues affect nerves and guide treatment.
Here’s a comparison of the diagnostic methods we discussed:
| Diagnostic Method | Primary Use | Key Benefits |
|---|---|---|
| Physical Examination | Initial assessment | Non-invasive, cost-effective |
| MRI | Soft tissue evaluation | High-resolution images of discs and nerves |
| CT Scans/X-rays | Bony structure assessment | Quick, widely available |
| EMG/NCS | Nerve function assessment | Assesses nerve damage and function |
Bulging discs can be treated in many ways, from simple to complex methods. The right treatment depends on how bad the symptoms are, how big the bulge is, and the patient’s health.
The first step is often rest and activity modification. This means avoiding heavy lifting and bending. It also means not doing things that make the problem worse. This helps the disc heal and reduces pain.
We suggest changing daily activities to protect the spine.
Physical therapy is key in treating bulging discs. It helps strengthen the muscles around the spine and improves flexibility. It also helps with posture.
Exercises like stretching, core strengthening, and aerobic activities are common. Our physical therapists create a program that meets each patient’s needs and goals.
Pain management is very important in treating bulging discs. Over-the-counter pain relievers can help with pain and inflammation. Sometimes, stronger medicines or muscle relaxants are needed.
We help patients find a pain management plan that works well without too many side effects.
For those who don’t get better with simple treatments, minimally invasive interventions might be an option. These include things like epidural steroid injections or percutaneous disc decompression. They aim to reduce inflammation and relieve nerve pressure.
We talk to our patients about the benefits and risks of these options to find the best choice.
With a complete treatment plan, people with bulging discs can see big improvements. We focus on giving each patient the care they need, tailored just for them.
Treating herniated discs involves different methods, from non-surgical to surgical options. We will look at the best ways to manage herniated discs.
First, we try non-surgical treatments. This includes rest, physical therapy, and managing pain. Most people see big improvements in 6-12 weeks.
Conservative Management Strategies:
Managing pain is key in treating herniated discs. We use medicines like NSAIDs and muscle relaxants to help with pain and swelling.
For those who don’t get better with non-surgical methods, injections can help. These injections put corticosteroids near the spinal cord.
If non-surgical methods don’t work, surgery might be needed. Common surgeries include discectomy and microdiscectomy.
| Surgical Procedure | Description | Recovery Time |
|---|---|---|
| Discectomy | Removal of the herniated disc | 4-6 weeks |
| Microdiscectomy | Minimally invasive removal of the herniated disc | 2-4 weeks |
Knowing about herniated disc treatments helps in making good choices. We aim to support you fully during your treatment.
Understanding different spinal conditions is key to making an accurate diagnosis. This includes degenerative disc disease and spinal stenosis. When symptoms like bulging or herniated discs appear, it’s important to look at other conditions that might be causing pain.
Degenerative disc disease (DDD) happens when spinal discs wear down over time, often due to aging. A bulging disc can be part of DDD, but not all bulging discs are due to degeneration. DDD also involves changes like disc height loss, annular tears, and inflammation.
To tell DDD apart from a simple bulging disc, look at these factors:
| Characteristics | Degenerative Disc Disease | Bulging Disc |
|---|---|---|
| Primary Cause | Aging and wear | Often related to injury or posture |
| Disc Changes | Loss of height, tears, inflammation | Bulging without significant degeneration |
| Symptoms | Chronic pain, stiffness | Variable, sometimes asymptomatic |
Disc protrusion and disc bulge are often confused, but they’re different. A disc bulge is a general bulging of the disc margin. A disc protrusion is a more focused extension of disc material beyond the normal space.
The main differences are:
Spinal stenosis is when the spinal canal narrows, compressing nerves and causing pain. Facet joint problems, like arthritis and cysts, can also lead to pain and nerve compression.
It’s common for several spinal conditions to occur together, making diagnosis and treatment harder. For example, a patient might have a bulging disc and spinal stenosis, or degenerative disc disease with facet joint arthritis.
When this happens, we must figure out which conditions are causing the most symptoms. This might involve:
Knowing the difference between bulging and herniated discs is key to managing them well. At Liv Hospital, we offer top-notch healthcare to international patients. We help them deal with disc problems effectively.
Dealing with disc issues needs a mix of lifestyle changes, physical therapy, and sometimes medical help. Being proactive can help lessen symptoms and enhance life quality.
Understanding your disc problem is the first step in managing it. Our team at Liv Hospital is here to give you personalized care. We make sure you get the right treatment for your specific case, whether it’s a bulging or herniated disc.
We combine medical knowledge with a focus on the patient. This way, we help you manage your condition. You can make informed choices about your care and move forward with confidence.
A bulging disc happens when the disc pushes out but doesn’t break. A herniated disc, on the other hand, is when the outer layer breaks. This lets the soft inside leak out.
No, they are not the same. Both involve changes in spinal discs, but they are different conditions.
Doctors use physical exams, MRI, CT scans, and X-rays to diagnose these conditions.
Symptoms include mild to moderate back pain, stiffness, and less mobility.
Symptoms can be severe back pain, numbness, tingling, and weakness. This depends on where and how bad the herniation is.
Yes, a bulging disc can turn into a herniated disc. But not all bulging discs will become herniated.
Treatment options depend on the condition and how severe it is. They can include rest, physical therapy, medications, minimally invasive procedures, and surgery.
Degenerative disc disease is wear and tear on spinal discs over time. A bulging disc is when the disc pushes out.
Yes, staying healthy, exercising, and good posture can help prevent or manage disc problems.
If you have severe pain, numbness, tingling, or weakness, or if symptoms get worse, see a doctor. They can help figure out the best treatment.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!