At Liv Hospital, we know patients worry about shunt placement in the brain. A ventriculoperitoneal (VP) shunt is a thin, flexible tube system. It moves excess cerebrospinal fluid (CSF) from the brain’s ventricles to the abdomen.
This device is a lifesaver for treating hydrocephalus. It’s a condition where fluid builds up in the brain. The shunt system has three parts: a ventricular catheter inside the brain, a valve shunt behind the ear, and a distal catheter to the peritoneal cavity.
Key Takeaways
- A VP shunt is used to divert excess CSF from the brain’s ventricles.
- The shunt system consists of three parts: ventricular catheter, valve shunt, and distal catheter.
- It is a lifesaving device for individuals with hydrocephalus.
- Understanding the components and function of a VP shunt can alleviate concerns.
- Recent innovations in shunt design have improved patient outcomes.
Understanding Brain Shunts and Their Purpose
Brain shunts are medical devices that help treat conditions like hydrocephalus. They work by moving excess cerebrospinal fluid (CSF) from the brain. These devices are key in managing neurological conditions by controlling CSF flow and pressure.
Definition and Basic Function of Brain Shunts
A brain shunt acts like a drainage system. It helps reduce pressure caused by too much CSF in the brain. Its main job is to move this extra fluid to another part of the body where it can be absorbed.
Conditions Requiring Shunt Placement
Shunts are often needed for hydrocephalus, where CSF builds up in the brain. This leads to high pressure inside the skull. Other conditions that affect CSF flow or absorption may also require a shunt.
Cerebrospinal Fluid (CSF) and Its Role
Cerebrospinal fluid is vital for brain health. It cushions the brain, supplies nutrients, and removes waste. Studies on CSF metabolomics show its importance in understanding neurological diseases.
The shunt valve is a key part that controls CSF flow. It prevents too much fluid from draining, keeping the brain’s pressure just right.
| Condition | Role of CSF | Shunt Function |
|---|---|---|
| Hydrocephalus | Accumulation of CSF leading to increased intracranial pressure | Drain excess CSF to reduce pressure |
| Normal Pressure Hydrocephalus | Impaired CSF circulation and absorption | Regulate CSF flow and pressure |
| Other Neurological Conditions | Affects CSF circulation or absorption | Divert excess CSF to alleviate pressure |
What Does a Shunt Look Like? Visual Characteristics
Medical technology has improved a lot. Now, shunts are more effective and less noticeable. They are made to be small and work well, without being seen much.
Physical Appearance of Modern Shunt Systems
Shunt systems have parts like a ventricular catheter, a shunt valve, and a distal catheter. These parts look different based on who made them and how they are designed. They are usually made of flexible, safe materials like silicone.
Size and Materials Used in Shunt Construction
Shunts come in different sizes, but they are made to be small. They are made of strong, safe materials. Silicone is often used because it’s flexible and doesn’t break down easily.
Visibility of Shunts After Placement
After they are put in, shunts are usually not seen from the outside. But, some parts might be felt or seen in certain situations.
External Visibility Considerations
Most of the time, you can’t see the shunt outside the body. But, in very thin people or if it’s placed close to the skin, you might see or feel it.
Palpable Components
Some parts, like the shunt valve, can be felt under the skin. This is more likely if it’s near the surface.
| Component | Typical Material | Palpability |
|---|---|---|
| Ventricular Catheter | Silicone | No |
| Shunt Valve | Metal or Plastic | Yes |
| Distal Catheter | Silicone | No |
Knowing what a shunt looks like can help patients feel better after surgery. Even though it’s usually not seen, knowing what to expect can make them feel more at ease.
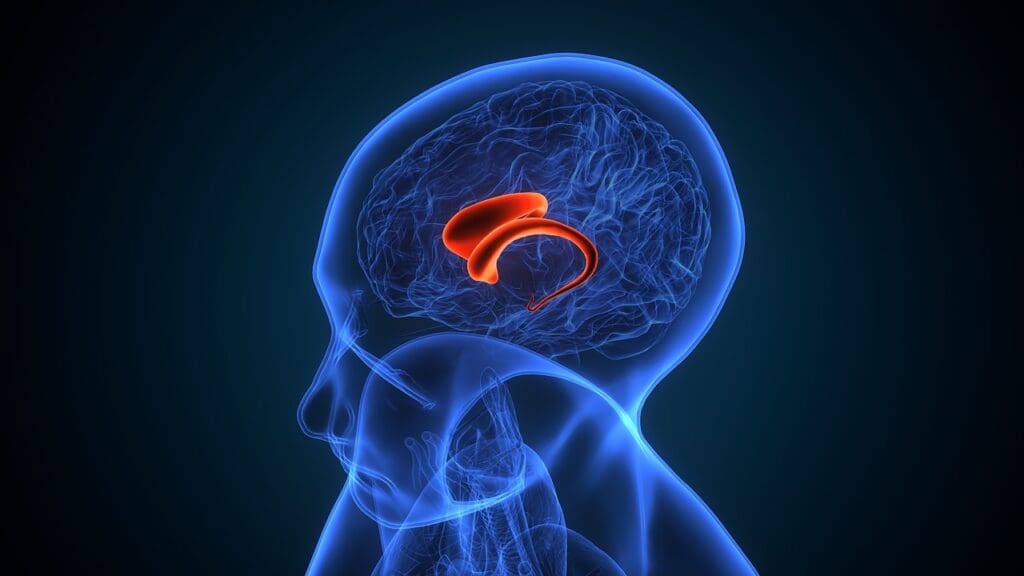
Anatomy of a Ventriculoperitoneal (VP) Shunt System
Knowing the parts of a Ventriculoperitoneal (VP) shunt system is key for patients and doctors. A VP shunt helps treat hydrocephalus by moving extra cerebrospinal fluid (CSF) from the brain to the belly. There, it gets absorbed.
The Ventricular Catheter: Placement and Design
The ventricular catheter is a key part of the VP shunt system. It goes into the brain’s ventricles to drain extra CSF. It’s made from flexible, safe materials like silicone.
Key Features: The catheter has holes to let CSF flow. Its placement is carefully done to ensure good drainage and avoid problems.
The Shunt Valve: Function and Location
The shunt valve controls CSF flow. It’s placed under the scalp, behind the ear. It can be fixed or adjustable, depending on the patient’s needs.
“The shunt valve is a critical element in managing the flow of cerebrospinal fluid, and its proper functioning is essential for the effective treatment of hydrocephalus.”
The VP Shunt Reservoir: Purpose and Identification
The VP shunt reservoir lets doctors take CSF samples and check the shunt. It’s under the scalp and used for tests.
The Distal Catheter: Routing and Termination
The distal catheter connects the shunt valve to the belly. It’s tunneled under the skin from the head to the abdomen.
Subcutaneous Pathway
The subcutaneous pathway is the route the distal catheter takes under the skin. It’s designed to lower infection risk and keep the catheter in place.
Peritoneal Placement
The catheter’s end is in the belly, where CSF is absorbed. The belly’s large area helps absorb the fluid well.
| Component | Function | Location |
|---|---|---|
| Ventricular Catheter | Drains CSF from the brain | Within the brain’s ventricles |
| Shunt Valve | Regulates CSF flow | Under the scalp, behind the ear |
| VP Shunt Reservoir | Allows for CSF sampling and shunt checking | Under the scalp |
| Distal Catheter | Connects shunt valve to peritoneal cavity | Tunneled under the skin to the abdomen |
We’ve looked at the VP shunt system’s anatomy, focusing on its main parts and roles. Understanding these is key for managing hydrocephalus well.
Types of Brain Shunts for Hydrocephalus Treatment
There are different types of brain shunts for hydrocephalus. Each type is designed to meet specific patient needs. This variety in design and function helps tailor treatments, leading to better outcomes for patients.
Ventriculoperitoneal (VP) Shunts
Ventriculoperitoneal (VP) shunts are widely used. They have a catheter in the brain’s ventricle, connected to a valve and then to the abdomen. These shunts work well for both kids and adults.
Key Features of VP Shunts:
- Flexible and adjustable valve settings
- Ability to accommodate growth in pediatric patients
- Effective in managing hydrocephalus symptoms
Ventriculoatrial (VA) Shunts
Ventriculoatrial (VA) shunts are another option. They move CSF from the brain to the heart’s atrium. VA shunts are chosen when VP shunts can’t be used, often due to abdominal problems.
Characteristics of VA Shunts:
- Less commonly used than VP shunts
- Requires careful monitoring due to possible heart issues
- Good for patients with abdominal infections or adhesions
Ventriculopleural Shunts
Ventriculopleural shunts send CSF to the space around the lungs. They’re less common and used when other shunts can’t be placed.
Features of Ventriculopleural Shunts:
- Used when other shunt types are contraindicated
- Potential risks include pleural effusion and respiratory complications
Lumboperitoneal Shunts
Lumboperitoneal shunts move CSF from the lower back to the abdomen. They’re great for treating certain hydrocephalus types, like idiopathic intracranial hypertension.
Advantages of Lumboperitoneal Shunts:
- Less invasive compared to ventricular shunts
- Effective in managing conditions like pseudotumor cerebri
Endoscopic Third Ventriculostomy (ETV) as an Alternative
Endoscopic Third Ventriculostomy (ETV) creates a new CSF pathway in the brain. It might avoid the need for a shunt. ETV is a good option for some patients.
ETV Considerations:
- Suitable for patients with certain types of obstructive hydrocephalus
- Avoids the need for implanted hardware
- May reduce the risk of shunt-related complications
There are different shunt surgeries, like programmable and fixed-pressure shunts. Research has led to many shunt types, giving more treatment options for hydrocephalus patients.
| Shunt Type | Description | Key Indications |
|---|---|---|
| Ventriculoperitoneal (VP) Shunt | CSF diverted from brain ventricles to peritoneal cavity | General hydrocephalus treatment |
| Ventriculoatrial (VA) Shunt | CSF diverted from brain ventricles to heart atrium | Abdominal issues or VP shunt failure |
| Ventriculopleural Shunt | CSF diverted from brain ventricles to pleural space | Contraindications for VP or VA shunts |
| Lumboperitoneal Shunt | CSF diverted from lumbar subarachnoid space to peritoneal cavity | Idiopathic intracranial hypertension, pseudotumor cerebri |
Shunt Valve Technologies and Pressure Regulation
Shunt valves are key in managing hydrocephalus by controlling CSF flow. They prevent overdrainage. The shunt valve is a vital part of the VP shunt system. It controls CSF flow between the ventricles and the peritoneal cavity.
Fixed-Pressure Valves
Fixed-pressure valves keep a steady pressure difference. They open when the pressure hits a certain level, letting CSF flow out. But, they might not work for everyone, as they don’t adjust to changes in posture or activity.
Programmable (Adjustable) Valves
Programmable valves can be adjusted without surgery. This is great for patients with changing CSF needs. They help keep CSF flow just right, avoiding too much or too little drainage.
Anti-Siphon Devices and Gravity-Compensating Valves
Anti-siphon devices and gravity-compensating valves stop overdrainage, mainly when standing. They fight the siphoning effect from height differences. This helps avoid slit ventricle syndrome and other overdrainage issues.
Flow-Regulated Valves
Flow-regulated valves keep CSF flow steady, no matter the pressure. They aim to improve drainage consistency. This could lower the chance of shunt problems.
New shunt valve tech has greatly helped hydrocephalus care. Knowing about these valves helps doctors tailor treatments. This improves patient outcomes and life quality.
Imaging of Brain Shunts: How They Appear on Scans
CT scans and MRI are key tools for checking shunt placement and any issues. They help doctors see where the shunt is and if it’s working right. This is very important for treating hydrocephalus.
Shunt Appearance on CT Scans
CT scans are often used to check VP shunts. On a CT scan, a shunt looks like a line from the ventricle to the belly. The shunt’s metal parts show up well against the brain, making it easy to see where it is.
Shunt Visualization in MRI
MRI gives detailed brain pictures and can check shunt placement without radiation. But, how a shunt looks on MRI depends on its material. Some parts might look like dark spots or odd shapes, so doctors need to be careful when looking at them.
X-ray Identification of Shunt Components
X-rays help see the shunt’s path. They can spot any problems like kinks or breaks. X-rays are great for making sure the shunt tubing is connected from the head to the belly.
Ultrasound Imaging of Shunts in Infants
Ultrasound is good for checking shunts in babies without radiation. It’s very useful for putting in the first shunt and for follow-ups in young kids.
Identifying Proper Placement
It’s very important to place the shunt correctly to manage hydrocephalus well. Imaging helps make sure the ventricular catheter is in the right spot in the ventricle. It also checks if the other end is in the right place, like in the belly.
Detecting Possible Complications
Imaging is also key for spotting shunt problems like blockages, infections, or mechanical failures. Regular scans can find issues early. This means doctors can act fast and avoid serious problems.
Using different imaging methods helps doctors make sure shunts work well. This improves care for patients with hydrocephalus.
Shunts for Hydrocephalus in Children vs. Adults
Shunts for hydrocephalus change a lot between kids and adults. This is because kids and adults have different bodies and health issues. We need to treat hydrocephalus in different ways for each age group.
Pediatric Considerations in Shunt Design and Placement
For kids, shunts must grow with them. Pediatric shunts are made to be flexible for changing needs as they grow.
A study showed how important it is to think about kids’ needs:
“The management of hydrocephalus in children requires a complete approach. We must consider the child’s age, size, and developmental stage.”
Adult Hydrocephalus Shunt Requirements
Adults need different shunts than kids. Adult shunts focus on lasting strength and stability. This is because adults’ hydrocephalus is usually more stable and doesn’t change as much with growth.
Growth Accommodation in Pediatric Patients
One big challenge in kids’ shunt care is growing. This means using shunts that can change as they grow.
| Feature | Pediatric Shunts | Adult Shunts |
|---|---|---|
| Design Focus | Adaptability and adjustability for growth | Long-term durability and stability |
| Valve Type | Often programmable or adjustable | Fixed-pressure or programmable |
| Monitoring | Frequent follow-ups for growth assessment | Regular check-ups, less frequent than in children |
Long-term Management Differences
Managing shunts long-term is different for kids and adults. Kids need close monitoring because of growth and possible shunt problems. Adults usually don’t need as many check-ups unless there’s a problem.
It’s key to understand these differences for the best care. By making shunts and care plans for each age group, we can help patients live better lives.
Innovations in Shunt Design and Technology
New shunt designs focus on making them safer and more effective. These advancements come from ongoing research and new technologies.
Antimicrobial Shunt Materials
One big improvement is antimicrobial shunt materials. These materials help prevent infections, a common problem with shunts. By adding antimicrobial properties, makers hope to cut down on shunt-related infections.
Smart Shunts with Monitoring Capabilities
Smart shunts are another exciting development. They can track intracranial pressure and other important health signs in real time. This helps doctors make better decisions for their patients.
Minimally Invasive Placement Techniques
There’s also a push for less invasive shunt placement methods. These methods cause less damage and help patients recover faster. This means better care for everyone.
Research Directions in Reducing Malfunction Rates
Scientists are working hard to make shunts last longer and work better. They’re looking at stronger materials and designs that can grow with children. This is key for kids, as their needs change over time.
Some of the key innovations include:
- Advanced valve technologies that allow for more precise pressure regulation
- Improved catheter designs that reduce the risk of blockage
- Integration of sensors for real-time monitoring
These new shunt designs and technologies are vital. They help manage hydrocephalus better and improve patients’ lives.
Conclusion: The Future of Brain Shunt Technology
As we wrap up our look at brain shunt technology, it’s obvious that research and innovation will keep getting better. At Liv Hospital, we’re all about supporting these advancements. We see a bright future for this field.
Research and development will keep pushing shunt technology forward. We expect to see better designs that make patients more comfortable. These improvements will also lower the chance of complications and make shunts more effective.
We think future shunts will use the latest materials and tech. Think antimicrobial coatings and advanced valves. These features will help prevent shunt failures and improve patient outcomes for those with hydrocephalus.
As the technology evolves, we’re dedicated to top-notch healthcare for everyone. By keeping up with the latest in shunt tech, we ensure our patients get the best care possible.
What does a VP shunt look like in the brain?
A VP shunt is a device to treat hydrocephalus. It moves excess cerebrospinal fluid from the brain to the abdomen. It has a ventricular catheter, shunt valve, and distal catheter, all made of silicone or similar materials.
What are the components of a VP shunt system?
A VP shunt system has a ventricular catheter, shunt valve, VP shunt reservoir, and distal catheter. The ventricular catheter is in the brain’s ventricle. The shunt valve controls CSF flow. The distal catheter sends CSF to the abdomen.
How do shunts appear on imaging studies?
Shunts show up on CT scans, MRI, X-ray, and ultrasound. On CT scans, they look like a line in the brain’s ventricles. MRI shows them as a signal void or thin line. X-rays help spot shunt parts. Ultrasound is good for checking shunt placement in babies.
What are the different types of brain shunts used to treat hydrocephalus?
There are many brain shunts, like VP shunts, VA shunts, and lumboperitoneal shunts. Each has its own use and benefits. VP shunts are the most common.
How do shunt valves work, and what are the different types?
Shunt valves control CSF flow by opening and closing with pressure changes. There are fixed-pressure, programmable, anti-siphon, and flow-regulated valves. Each has its own benefits and challenges.
What are the latest advancements in shunt technology?
New shunt tech includes antimicrobial materials and smart shunts. These advancements aim to make shunts last longer, reduce problems, and improve patient care.
How do shunt requirements differ between children and adults?
Children and adults need different shunts because of growth. Pediatric shunts grow with the child. Adult shunts manage hydrocephalus for a long time.
What is the role of cerebrospinal fluid (CSF) in brain health?
CSF is vital for brain health. It cushions the brain, controls pressure, and removes waste. Problems with CSF can lead to hydrocephalus, needing a shunt.
Are there any alternatives to shunt placement for treating hydrocephalus?
Endoscopic third ventriculostomy (ETV) is a surgery that might replace shunts for some patients. It creates a new CSF flow path, possibly avoiding the need for a shunt.
What are the benefits of programmable shunt valves?
Programmable shunt valves can adjust pressure without surgery. This gives more control over CSF flow, possibly reducing the need for more surgeries.
References
- Hydrocephalus Association (Shunt Systems) : https://www.hydroassoc.org/shunt-systems
- Wikipedia (Cerebral Shunt) : https://en.wikipedia.org/wiki/Cerebral_shunt
- Radiopaedia (Ventriculoperitoneal Shunt) : https://radiopaedia.org/articles/ventriculoperitoneal-shunt?lang=us
- American Journal of Roentgenology (AJR) : https://www.ajronline.org/doi/10.2214/AJR.12.10270
- Don’t Forget The Bubbles (VP Shunts) : https://dontforgetthebubbles.com/vp-shunts