Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we focus on the patient when treating abdominal aortic aneurysm EVAR. This method is less invasive and safer than traditional surgery, and it leads to better survival rates immediately after treatment.
We guide our patients through the steps of the abdominal aortic aneurysm EVAR procedure, ensuring they receive full care and support. Using advanced imaging and a stent graft, we block the aneurysm, making the treatment both safer and more effective.
Key Takeaways
- Minimally invasive EVAR procedure offers lower perioperative risk.
- Advanced imaging techniques guide the placement of a stent graft.
- EVAR provides improved short-term survival rates compared to open surgical repair.
- Comprehensive care and support are provided throughout the treatment journey.
- Patient-centered approach ensures personalized treatment plans.
Understanding Abdominal Aortic Aneurysm EVAR
EVAR, or endovascular aneurysm repair, is a new way to treat abdominal aortic aneurysms. It’s less invasive than traditional surgery. Let’s explore what EVAR is and how it works.
What is an Abdominal Aortic Aneurysm?
An abdominal aortic aneurysm (AAA) is a swelling in the main blood vessel. It runs from the heart through the belly. This swelling can grow or stay the same size, and it can burst if it gets too weak.
Because of the risk of bursting, finding and treating it quickly is very important.
Evolution of Endovascular Repair Techniques
Endovascular repair has come a long way. It started as a less invasive option compared to open surgery. Now, it uses many different devices and methods to fit each patient’s needs.
Thanks to these advancements, EVAR has become safer. It now has a lower risk of heart problems during and after surgery. This is because of better technology and techniques.
Current Statistics and Success Rates
EVAR has shown great success in treating abdominal aortic aneurysms. It has lower rates of complications and death compared to open surgery. This is true, at least in the short term.
| Outcome Measure | EVAR | Open Repair |
| Perioperative Mortality | 1-5% | 5-10% |
| Major Complications | 10-20% | 20-30% |
| Hospital Stay | 2-5 days | 7-14 days |
These numbers show how EVAR helps patients with abdominal aortic aneurysms. It reduces complications and improves their chances of a better outcome.
Benefits of Endovascular Approach vs. Open Surgical Repair

EVAR offers many benefits over open surgery, like lower death rates and quicker recovery. These advantages make EVAR a top choice for treating Abdominal Aortic Aneurysm.
Reduced Perioperative Mortality (1-5%)
EVAR cuts down on death rates by 1-5% compared to open surgery. This is a big deal because it means more patients survive the initial treatment.
Decreased Cardiac-Related Risks
EVAR also lowers heart risks, a big worry with open surgery. It’s less invasive, which means less stress on the heart.
Shorter Hospital Stay and Recovery Time
Plus, EVAR means shorter hospital stays and quicker recovery. Patients feel less pain and can get back to life faster than with open surgery.
In summary, EVAR’s benefits are clear, making it a great choice for many patients. Knowing these advantages helps doctors guide patients to the best treatment.
Patient Selection Criteria for EVAR
To get the most from EVAR, finding the right patients is key. This means checking their body’s shape and health closely. It’s all about picking the right person for this surgery.
Anatomical Requirements and Considerations
The shape of the aorta and the blood vessels are very important. Things like the size and angle of the aortic neck, any blood clots, and the health of the iliac arteries matter a lot. It’s important to measure and check these things carefully to see if a patient can use a stent graft.
Contraindications for Endovascular Repair
Some body shapes or health issues might make EVAR not work. For example, big angles in the aortic neck or very short or wide necks can be a problem. Doctors need to use their experience and judgment to decide if EVAR is right.
Expanding Eligibility with New Device Technology
New stent grafts can help more people get EVAR. These newer devices can handle tricky body shapes and long, twisted blood vessels.
Thanks to these new tools, doctors can fix more complex aneurysms. This means more people can get EVAR, which is great for their health.
Pre-operative Planning and Imaging Assessment
The success of EVAR depends a lot on careful planning before surgery and precise imaging. Advanced imaging helps place the stent graft correctly. This ensures the best results for the patient.
CT Angiography Protocol
CT angiography is key in planning for EVAR. It gives detailed pictures of the aorta and its branches. This helps us measure accurately and understand the aneurysm’s shape.
We stick to a set CT angiography protocol for top-notch images. This includes thin slices, contrast, and images from the celiac trunk to the femoral arteries.
| Protocol Component | Description | Importance |
| Thin-slice Reconstructions | 1-2 mm slice thickness | Enhances accuracy of measurements |
| Contrast Enhancement | Optimal timing for contrast injection | Improves visualization of vascular structures |
| Imaging Coverage | From celiac trunk to femoral arteries | Ensures complete view of aortoiliac anatomy |
Stent Graft Selection and Sizing
Choosing the right stent graft size is vital for EVAR success. We use CT angiography data to pick the best size and type.
We look at the aneurysm’s neck size, length, and angle. We also consider the iliac artery size and twists.
3D Reconstruction and Procedural Simulation
3D models and simulation help us plan EVAR better. They give us a clear view of the patient’s anatomy.
We use special software to make detailed 3D models. This lets us practice placing the stent graft and predict any issues.
By using these advanced imaging methods, we can make EVAR more effective. This leads to better results for our patients.
Essential Equipment and Team Preparation
To succeed in EVAR, having the right equipment and a prepared team is key. A well-organized setup and a skilled team are vital. They help navigate the complexities of endovascular repair.
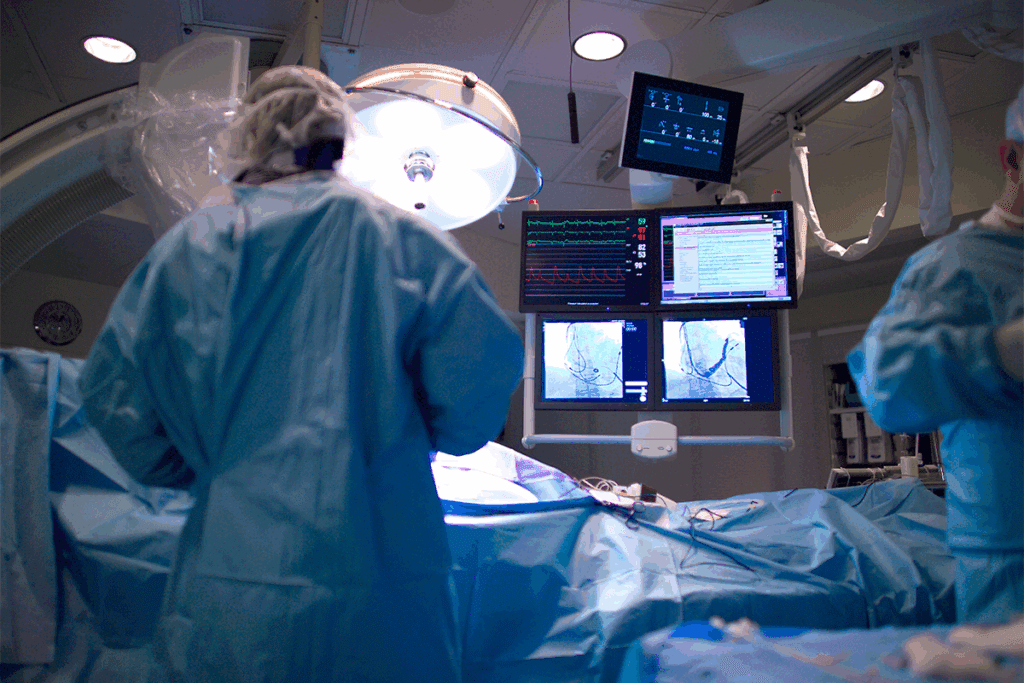
Hybrid Operating Room Setup
A hybrid operating room combines traditional ORs with advanced imaging. This setup is crucial for EVAR. It allows for real-time imaging and precise stent graft placement.
The room has a fixed imaging system, like a C-arm or ceiling-mounted angiography system. This provides high-quality images. It also has a fully equipped anesthesia workspace and advanced monitoring.
According to a study on the National Center for Biotechnology Information website, the hybrid OR setup boosts EVAR safety and effectiveness.
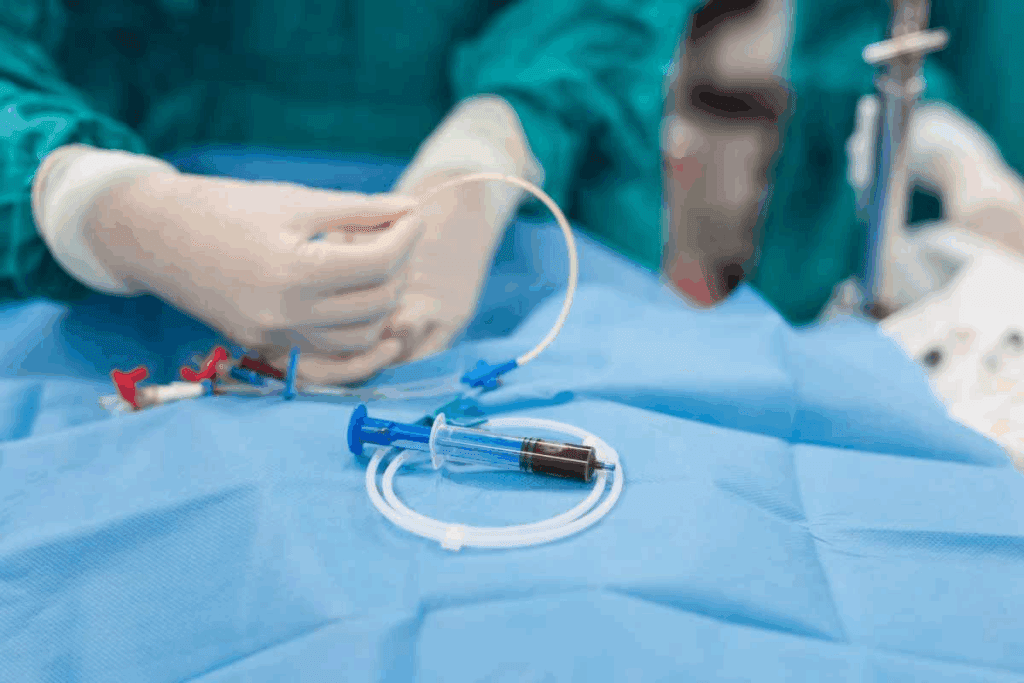
Required Endovascular Tools and Devices
The success of EVAR relies on the right endovascular tools and devices. These include stent grafts, catheters, guidewires, and balloons. The choice depends on the patient’s anatomy and the procedure’s needs.
- Stent grafts: These are used to exclude the aneurysm from circulation. Various types are available, including bifurcated, aorto-uni-iliac, and tubular grafts.
- Catheters and guidewires: These help navigate the vascular system and deliver the stent graft.
- Balloon catheters: These are for angioplasty and ensuring the stent graft fits properly against the arterial wall.
Team Composition and Roles
A multidisciplinary team is vital for EVAR success. The team includes vascular surgeons, interventional radiologists, anesthesiologists, nurses, and radiologic technologists. Each member has specific roles and responsibilities:
- Vascular surgeons and interventional radiologists: They perform the procedure, guiding the stent graft to the aneurysm site.
- Anesthesiologists: They manage patient anesthesia and hemodynamics during the procedure.
- Nurses and radiologic technologists: They assist during the procedure, manage equipment, and monitor patient vital signs.
Effective communication and coordination among team members are critical. They ensure the smooth execution of EVAR and manage any complications.
Step 1: Establishing Bilateral Arterial Access
Starting the EVAR procedure with bilateral arterial access is key. It needs skill and precision. This step is vital for putting in the stent graft and the procedure’s success.
Percutaneous vs. Cutdown Techniques
Choosing between percutaneous and cutdown techniques depends on many things. These include the patient’s body, the doctor’s choice, and hospital rules. Percutaneous access is less invasive and can help patients recover faster. On the other hand, cutdown techniques give more control and might lower the risk of problems.
| Technique | Advantages | Disadvantages |
| Percutaneous | Less invasive, quicker recovery | Potential for access site complications |
| Cutdown | More control over access site, reduced risk of complications | More invasive, longer recovery time |
Sheath Placement and Heparinization
After getting access, sheath placement is key for the stent graft. The sheath’s size and type depend on the device and patient’s body. Then, heparinization is done to stop blood clots during the procedure.
Alternative Access Routes for Challenging Anatomy
When standard femoral access is hard, other routes are considered. These include iliac or brachial access. Each has its own challenges and risks.
Knowing the details of bilateral arterial access is vital for EVAR success. Choosing the right method and managing access issues can greatly improve the procedure’s outcome.
Step 2: Diagnostic Angiography and Roadmapping
Diagnostic angiography and roadmapping are key steps in the EVAR procedure. They help place the stent graft accurately. These methods let us see the aortic anatomy and guide the stent graft into the right spot.
Catheter Selection and Positioning
Choosing the right catheter is essential for successful diagnostic angiography. We pick catheters based on the patient’s anatomy and the procedure’s needs. Catheter positioning is also critical. It must be done to get the best angiographic images.
- Catheter size and type are chosen based on patient anatomy.
- Precise positioning ensures high-quality angiographic images.
Contrast Injection Techniques
Effective contrast injection is key to seeing the aortic aneurysm and surrounding blood vessels. We use contrast injection techniques to get clear images. This helps us place the stent graft accurately.
- Contrast volume is calculated based on patient factors and procedural requirements.
- Injection rates are adjusted for optimal image quality.
Digital Subtraction Angiography Optimization
Digital subtraction angiography (DSA) is a main imaging tool in EVAR. We fine-tune DSA by tweaking parameters like frame rate and exposure settings. This ensures the best image quality.
- Frame rate adjustment enhances image clarity.
- Exposure settings are optimized for patient safety and image quality.
Mastering diagnostic angiography and roadmapping is key to a successful EVAR procedure. It leads to better patient outcomes.
Step 3: Main Body Stent Graft Deployment Technique
Deploying the main body stent graft is a key part of the EVAR procedure. It needs careful planning and execution. This step is vital for successfully excluding the abdominal aortic aneurysm.
Device Preparation and Inspection
Before we deploy the main body stent graft, we must prepare it thoroughly. We check the stent graft for any damage or defects. We also make sure all parts are there and that it fits the patient’s anatomy.
We prepare the delivery system as the manufacturer instructs. We look for any kinks or obstructions that could make deployment hard.
Navigation Through Iliac Arteries
Getting the main body stent graft through the iliac arteries is delicate. We use fluoroscopic guidance to watch its progress. We make adjustments as needed to avoid damaging the vessels.
Precise Positioning Below Renal Arteries
Positioning the main body stent graft below the renal arteries is key. We use angiographic landmarks and measure the distance to the aneurysm neck. This step is important to prevent renal artery occlusion and ensure proper exclusion of the aneurysm.
Controlled Deployment Sequence
The deployment sequence is controlled and done under fluoroscopic guidance. We watch it in real-time and make adjustments as needed. This careful approach reduces the risk of complications and ensures the stent graft is placed correctly.
By following these steps, we can successfully deploy the main body stent graft. This is essential for the success of the EVAR procedure.
Step 4: Contralateral Limb Cannulation and Completion
The contralateral limb cannulation step is key in the EVAR procedure. It makes sure the aneurysm is cut off from blood flow. Getting the contralateral limb right is essential for a complete fix.
Gate Cannulation Strategies
Gate cannulation is a precise method. It involves going through the stent graft’s main body to reach the contralateral gate. We use fluoroscopic guidance and special catheters to help get it right.
Key strategies include:
- Using a mix of guidewires and catheters to get through the graft
- Guiding with fluoroscopy to see the gate and place the catheter
- Using pre-op images to plan the best approach
Limb Deployment and Overlap Considerations
After getting to the contralateral gate, we deploy the limb of the stent graft. Getting it right and making sure it overlaps is key. This prevents leaks and makes the repair last longer.
| Deployment Consideration | Importance | Technique |
| Overlap | Prevents endoleaks | Ensure at least 3 cm overlap between main body and limb |
| Precise Positioning | Critical for aneurysm exclusion | Use angiography to guide precise placement |
Distal Extension Placement When Needed
Sometimes, we need to add a distal extension for a better seal and to stop leaks. We decide on this during the procedure.
The decision to use a distal extension is based on:
- How well the distal seal zone works
- How much disease is in the iliac arteries
- What the angiogram shows
Balloon Molding for Optimal Apposition
Balloon molding is vital for the stent graft to stick well to the artery wall. This stops leaks and makes the repair last.
Balloon molding technique involves:
- Using a soft balloon to shape the stent graft
- Inflating carefully to avoid too much stretching
- Checking with angiography after molding to make sure it’s sealed
Managing Complications During Abdominal Aortic Aneurysm EVAR
It’s important to handle complications during EVAR to keep patients safe and ensure the procedure works. We need to tackle endoleaks, manage access site issues, prevent renal artery blockage, and know when to switch to open repair.
Identifying and Addressing Endoleaks
Endoleaks are a big problem in EVAR. They happen when blood keeps flowing outside the stent graft but inside the aneurysm sac. We sort them into types based on where they come from.
| Type | Description | Management |
| Type I | Leak at the attachment site | Additional stent grafting or ballooning |
| Type II | Retrograde flow from branches | Observation, embolization |
| Type III | Leak through graft fabric or junctions | Additional stent grafting |
Managing Access Site Complications
Complications can happen at the access site, whether it’s percutaneous or open surgery. We must act fast to manage these issues.
- Hematoma formation
- Vascular injury
- Infection
To handle access site problems, we focus on careful wound closure, using closure devices, and keeping an eye on patients post-op.
Renal Artery Occlusion Prevention and Treatment
Renal artery blockage is a serious issue that can come from placing stent grafts. We avoid it by planning carefully and placing stent grafts accurately.
If it happens, we treat it by getting blood flow back to the renal arteries. This might mean stenting or surgery.
Conversion to Open Repair: When and How
Sometimes, we need to switch to open repair because of complications or if endovascular repair fails. We do this if we see endoleaks, aneurysm growth, or other issues that can’t be fixed with EVAR.
Conclusion: Post-EVAR Care and Long-term Surveillance
Good care after EVAR is key for the best results. We stress the need for ongoing checks after EVAR to catch any problems early.
These checks include watching for endoleaks, aneurysm growth, and stent graft health. This care helps spot issues quickly. It also lowers the chance of bad outcomes.
By focusing on post-EVAR care and sticking to a follow-up plan, we can make EVAR more successful. Keeping an eye on patients long-term is a big part of caring for them well.
FAQ
What is an EVAR procedure?
EVAR stands for Endovascular Aneurysm Repair. It’s a way to treat an abdominal aortic aneurysm (AAA) without a big surgery. A stent graft is put through the arteries to block the aneurysm from growing or bursting.
What are the benefits of EVAR compared to open surgical repair?
EVAR is better because it’s less risky and you can go home sooner. It also means less heart problems. These reasons make EVAR a good choice for many patients.
What are the anatomical requirements for EVAR?
For EVAR to work, the aorta needs to be the right size and shape. The iliac arteries also need to be big enough. These details help pick the right stent graft for you.
What is the role of pre-operative planning and imaging assessment in EVAR?
Before the surgery, we use CT scans and 3D models to plan. This helps pick the right stent graft. It makes sure the graft fits perfectly, which is key for success.
How is bilateral arterial access established during EVAR?
We use special techniques to get access to both arteries. This might be through a small cut or a needle. Sometimes, we need to find other ways to get in, depending on your body.
What are the possible complications during EVAR, and how are they managed?
Complications like leaks or blockages can happen. We have ways to fix these, like adding more stents or using special techniques. This keeps the aneurysm from getting worse.
What is the importance of post-EVAR care and long-term surveillance?
After EVAR, we keep an eye on you with regular checks. This makes sure the repair is working right. It also catches any new problems early.
How is endoleak managed during EVAR?
If there’s a leak, we figure out why and fix it. This might mean adding more stents or using special treatments. Quick action is key to stop the aneurysm from getting worse.
What is the role of a hybrid operating room in EVAR?
A hybrid room is great for EVAR. It has top-notch imaging and a clean area for surgery. This lets us place the stent graft exactly right and handle any problems that come up.
How is patient eligibility for EVAR determined?
We check if you’re a good fit for EVAR based on your body and health. New technology has made more people eligible for this safer option.
References:
- Björck, M., Wanhainen, A., & Koelemay, M. (2024). Endovascular aneurysm repair: Current status and future perspectives. The Lancet, 403(10387), 753-765. Retrieved fromhttps://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)02027-7/fulltext






