A coma is a deep sleep caused by brain injury, illness, or medical reasons. When someone falls into a coma, families seek hope and answers. At Liv Hospital, we guide patients and their families with trust and advanced, patient-centered care. We help them understand the journey ahead as science finds new ways to wake people up and help them recover.
Understanding coma and its aftermath can be tough. But with the right care and support, patients can navigate this difficult journey. We will give an overview of coma, its causes, and treatment options. We will also talk about what to expect during the recovery process.
Key Takeaways
- Coma is a state of deep unconsciousness resulting from brain injury or illness.
- Liv Hospital provides advanced, patient-centered care for coma patients.
- Recovery from a coma can be a challenging and complex process.
- Understanding the causes and treatment options for coma is key for patients and families.
- With the right care and support, patients can rebuild their lives after a coma.
Understanding Coma: A State of Deep Unconsciousness
To understand coma, we need to know its medical definition and what causes it. A coma is a deep sleep-like state that can happen for many reasons.
Definition and Medical Explanation
A coma is when someone can’t wake up and doesn’t respond to their surroundings. It’s a state of little brain activity and no consciousness. It can be caused by brain damage from trauma, infection, or substance abuse.
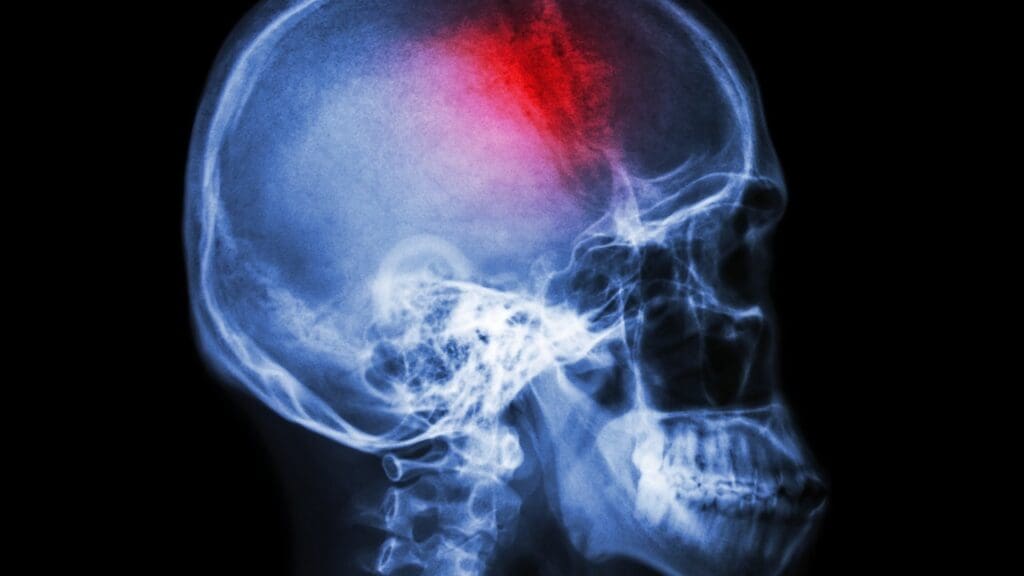
Common Causes: Traumatic vs. Medical Coma
Comas are mainly divided into two types: traumatic and medical. Traumatic comas come from head injuries or physical damage to the brain. Medical comas are due to infections, metabolic issues, or too much of a substance.
Measuring Consciousness: The Glasgow Coma Scale
The Glasgow Coma Scale (GCS) is a way to measure how awake someone is. It looks at eye opening, verbal response, and motor response. Scores range from 3 to 15, with higher scores meaning better brain function.
| GCS Component | Response | Score |
|---|---|---|
| Eye Opening | Spontaneously | 4 |
| To verbal command | 3 | |
| To pain | 2 | |
| No response | 1 | |
| Verbal Response | Oriented | 5 |
| Confused | 4 | |
| Inappropriate words | 3 | |
| Incomprehensible sounds | 2 | |
| No response | 1 | |
| Motor Response | Obeys commands | 6 |
| Localizes pain | 5 | |
| Withdrawal to pain | 4 | |
| Flexion to pain | 3 | |
| Extension to pain | 2 | |
| No response | 1 |
Doctors say the Glasgow Coma Scale is key for checking brain injury severity and predicting recovery. It helps doctors talk clearly about a patient’s condition and make the right care choices.
The Science Behind Brain Function During Coma
Understanding brain function in coma is key for doctors and families. We’ll look at brain activity changes, coma vs. other unconscious states, and if patients can hear or feel.
How Brain Activity Changes in Comatose Patients
In comas, brain activity drops a lot. EEG and fMRI show brain electrical activity changes. This shows a big drop in brain connection, marking coma.
Difference Between Coma and Other Unconscious States
Coma is often mixed up with other unconscious states. But coma is unique. It means no response or awareness. Vegetative state is wakefulness without awareness. The Glasgow Coma Scale helps measure consciousness.
| Condition | Characteristics | Level of Consciousness |
|---|---|---|
| Coma | Lack of responsiveness and awareness | Low |
| Vegetative State | Wakefulness without awareness | Moderate |
| Minimally Conscious State | Some awareness and responsiveness | Moderate to High |
Can Patients in Coma Hear or Feel Stimulation?
Studies say some comatose patients might hear or feel, but can’t respond well. This means talking to them and using sensory stimulation is important in their care.
It’s vital to treat each patient differently, as awareness levels vary greatly.
What Happens When You Go Into a Coma
When someone goes into a coma, their body changes a lot. This is because of a deep sleep-like state caused by serious illness or injury.
Immediate Physiological Changes
Right away, the body starts to change. These changes include changes in blood pressure, heart rate, and breathing. The brain’s control over these functions can be affected, making it important to watch them closely.
Can You Breathe in a Coma?
One big worry for coma patients is breathing. Some can breathe by themselves, but others need a machine to help. This depends on why they are in a coma and how much their brain is hurt.
Common Misconceptions About Coma States
There are many wrong ideas about comas that upset families. For example, some think coma patients know what’s going on but can’t talk. But this isn’t true for everyone. Some might have some awareness, but it’s different for each person.
| Physiological Change | Description | Clinical Significance |
|---|---|---|
| Blood Pressure Alterations | Changes in blood pressure can occur due to brain injury or illness. | Requires close monitoring to prevent hypotension or hypertension. |
| Heart Rate Variability | Heart rate can be affected by the autonomic nervous system’s response to coma. | Important for assessing cardiovascular stability. |
| Breathing Pattern Changes | Comatose patients may experience irregular breathing patterns. | May necessitate mechanical ventilation to ensure adequate oxygenation. |
Coma in Hospital: Medical Care and Monitoring
Hospital care for coma patients is complex. It aims to fix the cause and keep vital functions going. The team works hard to keep the patient stable and prevent brain damage.
Initial Assessment and Stabilization
The first step is a detailed check of the patient’s brain and body. Stabilizing the patient’s airway, breathing, and circulation (ABCs) is key. We also use scans like CT or MRI to find out why the coma happened.
Long-term Support Systems and Nutrition
After the patient is stable, we focus on long-term care. This includes making sure they get enough food. Nutritional support is given through tubes or IVs.
Daily Care Routines for Comatose Patients
Every day, we do things to help the patient. We turn them to avoid bedsores and do exercises to keep them flexible. We also watch for infections or other problems.
Preventing Complications
Stopping complications is very important. This means infection control, managing blood pressure, and avoiding blood clots. By being proactive, we help the patient recover better.
How Do You Wake Someone Up from a Coma?
Waking someone from a coma requires looking into medical strategies and new treatments. These methods aim to bring a person back to consciousness. The recovery time can vary a lot, based on the cause and the person’s health.
Natural Recovery Process
Some people might wake up from a coma on their own, without much medical help. The natural healing process depends on the coma’s cause, brain injury, and overall health.
Factors influencing natural recovery include:
- The severity of the initial injury or illness
- The patient’s age and general health
- The presence of any secondary complications
Medical Interventions to Stimulate Consciousness
For many, medical help is needed to wake them up. This can include medicines to reduce swelling or manage symptoms. It also includes care to keep vital functions going.
Common medical interventions include:
- Medication to manage pain or reduce inflammation
- Supportive care such as mechanical ventilation and nutritional support
- Rehabilitation therapies to regain lost functions
| Intervention Type | Purpose | Examples |
|---|---|---|
| Pharmacological | Manage symptoms, reduce inflammation | Sedatives, anti-inflammatory drugs |
| Supportive Care | Maintain vital functions | Mechanical ventilation, nutritional support |
| Rehabilitative | Regain lost functions | Physical, occupational, and speech therapy |
Emerging Treatments: Deep Brain Stimulation and Focused Ultrasound
New medical technologies have brought treatments like deep brain stimulation (DBS) and focused ultrasound (FUS). These aim to wake up comatose patients.
DBS involves putting electrodes in the brain to send electrical signals. FUS uses ultrasound waves to activate the brain without surgery.
Experimental Approaches in Research
Researchers are always finding new ways to help coma patients. These new treatments are tested in clinical trials. They offer hope for those with severe brain injuries.
As research keeps improving, we might see better ways to wake coma patients. This could help them recover more effectively.
Signs of Waking from Coma
Coming out of a coma is a slow process. It involves clear physical and brain changes that doctors watch closely. These signs show how well a patient is doing.
Physical Indicators of Recovery
Signs that a patient is waking up include opening their eyes and moving. They might also respond to voices. These are big steps towards recovery.
Is Coughing in a Coma a Good Sign?
Coughing is a good sign because it shows the brain is working. It means the patient might get better in other ways too. Doctors pay close attention to coughing.
Brain Activity Changes During Recovery
When patients wake up, their brain activity changes. Doctors use tests and scans to see this. These changes help doctors understand how well the patient is doing.
What Doctors Look For
Doctors watch many things, like how awake the patient is and how they think. They also look at physical responses. This helps doctors know if treatments are working and what to do next.
The Process of Coming Out of a Coma
Coming out of a coma is a complex and highly individualized process. It involves various stages of recovery. Each patient’s journey is unique and influenced by multiple factors.
Stages of Consciousness Recovery
The recovery from a coma progresses through several stages. First, patients may be in a vegetative state. They might have basic reflexes but are not conscious.
As they improve, they may enter a minimally conscious state. Here, they can show some awareness, like responding to stimuli. Further recovery can lead to a state where patients are more responsive. They can eventually regain full consciousness.
Throughout this process, medical professionals closely monitor the patient’s progress. They adjust treatment plans as necessary.
Timeline Expectations: Can Someone Wake Up After Months or Years?
The length of time a person remains in a coma can vary significantly. It can range from days to months or even years. While some patients may wake up relatively quickly, others may take much longer.
Research suggests that the likelihood of recovery decreases with time. But there are documented cases of patients waking up after extended periods.
| Time in Coma | Likelihood of Recovery |
|---|---|
| 0-3 months | High |
| 3-6 months | Moderate |
| 6-12 months | Low |
| 1-2 years | Very Low |
| More than 2 years | Extremely Low |
Factors That Influence Recovery Speed
Several factors influence the speed and extent of recovery from a coma. These include the severity of the brain injury and the patient’s age. Overall health and the presence of any underlying medical conditions also play a role.
The quality of care received during and after the coma is also important. It determines the outcomes.
Understanding these factors helps medical professionals tailor their care. They can optimize the chances for the best possible recovery.
What Happens When You Wake Up from a Coma
Waking up from a coma is a big step in recovery. But it’s just the start of many challenges. Patients slowly come back to life, facing physical, cognitive, and emotional changes.
Initial Disorientation and Confusion
Patients often feel disoriented and confused when they wake up. This is because they were unconscious for a long time. They might struggle to understand their surroundings or remember recent events.
One patient said, “I felt like I was dreaming, and everything was foggy and unclear.“
Physical and Cognitive Challenges
Waking up from a coma brings big physical and cognitive challenges. Patients may feel weak, tired, and have trouble with balance and coordination. They might also have trouble remembering things or focusing.
Rehabilitation is key in helping patients get stronger and improve their thinking skills.
Emotional and Psychological Impact
The emotional and psychological effects of waking up from a coma are significant. Patients may feel a mix of emotions, including relief, gratitude, anxiety, depression, and frustration. The recovery process can be very tough emotionally.
Memory and Identity Issues
Some patients struggle with memory and identity. They might have trouble remembering the past or feeling connected to their life before the coma.
“The hardest part was trying to piece together my life before the coma; it felt like remembering a dream.”
This part of recovery can be hard, needing patience and understanding from everyone involved.
It’s vital to give patients full care and support when they wake up from a coma. This includes medical treatment, emotional, and psychological support. It helps them deal with the challenges they face.
Life After a Coma: The Recovery Journey
Recovering from a coma takes a lot of effort. It involves medical care, rehabilitation, and support from family. Patients face a tough journey to get back their health and freedom.
Comprehensive Rehabilitation Programs
Rehabilitation programs are key for coma recovery. They have teams of experts like physical and speech therapists. The goal is to help patients regain lost skills.
Relearning Basic Skills and Functions
Relearning basic skills is a big part of recovery. Patients might need to learn again how to dress, eat, and walk. Therapists use special methods and tools to help.Family Support and Caregiver Roles
Family support is very important in recovery. They offer emotional help, daily care, and keep patients connected. Caregivers also need help, as caring for a coma survivor is tough.
Adjusting to a New Normal
Life after a coma is hard for patients and their families. They must adjust to new challenges. Support from healthcare, family, and friends is vital.
“Recovery is not just about getting strong physically,” says John Doe, a coma survivor. “It’s also about finding emotional strength. With the right support, you can live a fulfilling life again.”
Conclusion: Understanding the Path to Recovery
Recovering from a coma is a complex journey. It depends on the brain injury’s severity and the patient’s health. We’ve looked at coma’s definition, causes, treatments, and recovery stages.
Knowing about coma recovery is key for patients and their families. The road to recovery is long and tough. But, with proper care and support, patients can make big strides. Some even progress after years in a coma.
Waking up from a coma is just the start. Patients then face physical, mental, and emotional hurdles. Rehabilitation programs are essential in helping them regain basic skills.
By grasping what coma is and how recovery works, we can better support patients and their families. Our aim is to offer top-notch healthcare and support for international patients. Education and awareness are vital to achieving this.
What happens when you are in a coma?
Being in a coma means you’re very deep asleep and can’t wake up. You can’t respond to anything around you. We watch your health closely and give you care to help manage your situation.
Can someone wake up from a coma?
Yes, some people can wake up from a coma. How likely and when it happens depends on the cause, brain injury, and health. We use different treatments to help wake you up and support your recovery.
What happens when you wake up from a coma?
Waking up from a coma can be confusing and challenging. You might feel disoriented and struggle with basic skills. We offer rehabilitation to help you regain these skills. Our team also supports you and your family during this time.
Is coughing in a coma a good sign?
Coughing in a coma is a good sign. It means your body’s reflexes are coming back. We watch your body’s responses and brain activity to see how you’re doing and adjust your care.
Can you breathe in a coma?
Some coma patients can breathe on their own, while others need a machine to help. We check how you’re breathing and make sure you’re comfortable and safe.
How do you get out of a coma?
Getting out of a coma is different for everyone. We use various treatments and care to help you wake up and recover. It’s a process we tailor to each person’s needs.
What happens when you go into a coma?
Going into a coma changes your body right away. Your brain, heart, and blood pressure change. We keep a close eye on your health and give you care to prevent problems.
Can patients in a coma hear or feel stimulation?
Some research says coma patients might hear or feel things, but we don’t know how common this is. We’re studying brain function in comas to learn more about what patients might experience.
How long can someone be in a coma?
How long someone stays in a coma varies a lot. It can be days, weeks, months, or even years. We support you and your family no matter how long you’re in a coma.
What is the recovery process like after a coma?
Recovering from a coma is tough. It involves getting better physically, mentally, and emotionally. We offer rehabilitation and support to help you and your family adjust to life after a coma.
References
- Live Science (How do people wake up from comas?) : https://www.livescience.com/health/how-do-people-wake-up-from-comas
- Better Health Channel (Coma) : https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/coma
- Headway (Coma Stimulation Suggested Activities) : https://www.headway.org.uk/media/12034/coma-stimulation-suggested-activities-publication.pdf
- Brain Foundation (Coma) : https://brainfoundation.org.au/disorders/coma
- UCLA College (Jump-starting the Brain of a Patient Recovering from a Coma) : https://www.college.ucla.edu/2017/02/21/jump-starting-the-brain-of-a-patient-recovering-from-a-coma